Treatment
Treatment focuses on the following:
• Administering appropriate antibiotic therapy
• Observing respiratory status and indicators of the effectiveness of therapy
• Administering oxygen
• Administering adequate fluid intake to ensure hydration
• Providing adequate nutrition via small, frequent meals
• Positioning to aid breathing
• Turning, coughing, and deep breathing
• Maintaining accurate intake and output (I&O) records
• Providing frequent mouth care for comfort
Antibiotics have revolutionized the treatment of pneumonia. They are usually administered IV for rapid action and to maintain a blood level that is effective in eradicating the causative organism. In 24 to 48 hours, the fever usually disappears and the other symptoms dramatically decrease.
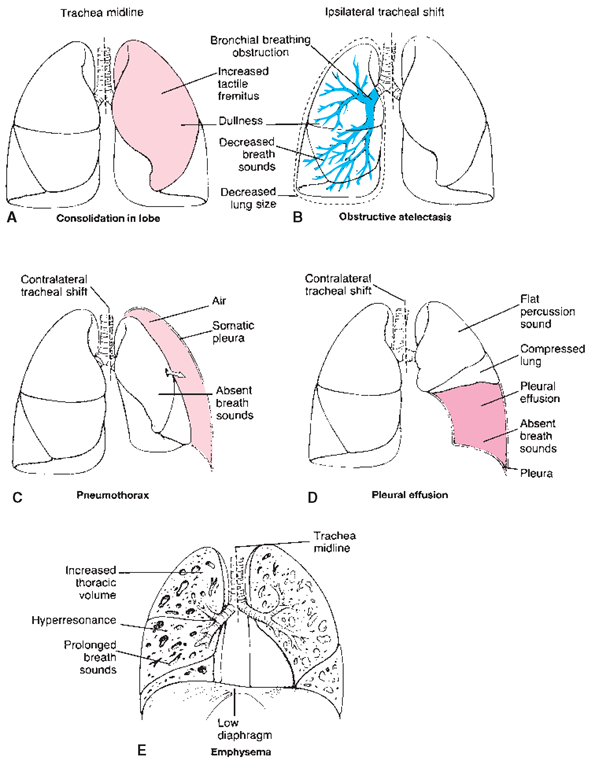
FIGURE 86-3 · Respiratory system disorders and their comparative effects on the lungs. (A) Consolidation within a lobe: trachea in center, dull sound in affected lobe. (B) Obstructive atelectasis: trachea shifts to affected (ipsilateral) side; decreased lung size, decreased breath sounds. (C) Pneumothorax: trachea shifts to other (contralateral) side; breath sounds absent on affected side. (D) Pleural effusion or hemothorax (fluid or blood pooling in pleural cavity): trachea shifts to other side; absent breath sounds in affected lobe; lung compressed.(E) Emphysema: enlarged (barrel) chest, prolonged breath sounds, hyperresonance (echo), trachea in center.
Nursing Considerations
In Practice: Nursing Care Guidelines 86-4 outlines nursing considerations for the client with pneumonia. Activity is gradually increased as the body convalesces slowly and builds resistance. A CXR is taken to make sure that the infection in the lungs has cleared completely.
Complications
Complications from pneumonia seldom occur today, except in older, debilitated, or immunocompromised clients. If the infection does spread, it also may cause inflammation of the pleura, the middle ear (otitis media), sinusitis, or bronchitis.
Pleurisy
Pleurisy, an inflammation of the pleura (the double membrane covering the lungs), can be a complication of pneumonia, caused by a spread of the infection from the lungs. The pleura becomes thickened, and the two membrane surfaces scrape together.
The client feels sharp pain with every breath. Later, as fluid forms, the pain diminishes, and a dry cough replaces it, accompanied by SOB and exhaustion after the slightest effort. (Pleuritic pain may occur with other diseases, such as rheumatic fever, systemic lupus erythematosus, and polyarteritis.)
Treatment of pleurisy is similar to that of pneumonia: bed rest and restriction of activity, along with anti-inflammatory agents. Encourage the person to cough, but because coughing may be painful, apply hot or cold packs over the area or have the person lie on the affected side for comfort.
IN PRACTICE :NURSING CARE GUIDELINES 86-4
CARING FOR THE PERSON WITH PNEUMONIA
• Always wash your hands and wear gloves, if indicated. Rationale: Handwashing and gloves help to prevent the spread of infection.
• Be alert for increasingly labored respirations. Rationale: If the person has difficulty breathing, he or she is given oxygen, usually by mask or cannula.
• Adjust the client’s position. An orthopneic position may be necessary. Rationale: Proper positioning helps the person to be more comfortable and to breathe more easily.
• Place a pillow lengthwise under the back. Rationale: This action encourages fuller chest expansion.
• Place a blanket around the shoulders if the person has chills. Rationale: A blanket provides comfort and warmth, minimizing energy expenditure.
• Keep the client’s bed dry Rationale: Wet bed linens can chill the client.
• Take the client’s vital signs at least every 4 hours. Rationale: Frequent monitoring is necessary to allow for prompt detection and early intervention if problems arise.
• Attempt to control fever and discomfort with acetaminophen or ibuprofen, if ordered. Tepid sponges may also be ordered. Rationale: Fever is often very high and can be dangerous.
• Maintain the intravenous (IV) site or heparin lock. Rationale: This client is probably receiving IV antibiotics.
• Put side rails up if any sign of confusion exists, especially in the older person. Rationale: The high fever, medications, and disease process may contribute to confusion and lead to injury.
• Encourage the client to cough and to expectorate secretions while splinting the chest. Rationale: Keep the lungs as free of secretions as possible. Splinting the chest helps to relieve the discomfort of coughing.
• Encourage deep breathing. Aerosolized treatments or incentive spirometry may be prescribed. Rationale: The lungs must be expanded as much as possible.
• Measure intake and output (I&O) and daily weights, if ordered. Rationale: Some clients may have edema. Others will need total parenteral nutrition (TPN) to maintain hydration and nutrition.
• Give small amounts of fluids frequently Rationale: Fluids help to encourage hydration.
• Provide frequent mouth care; put water-soluble lubricant (not oily) on the client’s lips. Rationale: A fever causes the mucous membranes to be very dry; probably this person also has been breathing through the mouth. Oil might be aspirated and is not used with oxygen.
• Keep the client’s surroundings quiet. Rationale: Rest promotes healing.
When fluid collection in the pleural space increases, the person is said to have a pleural effusion (see Fig. 86-3D). The client may exhibit the same symptoms as those seen with pleurisy but he or she often becomes dyspneic and has a rapid pulse. Pleural effusion can result from congestive heart failure, pulmonary infections (including TB), and malignancies. Treatment relates directly to the underlying cause and may be geared toward specific symptoms.
Histoplasmosis
Histoplasmosis, which mimics “summer flu” and is often misdiagnosed, is caused by inhaling spores of the fungus Histoplasma capsulatum. The spores are carried in dust from soil rich in the fungus, such as that in chicken houses, barns, or bat caves. The disease is not passed between individuals. Typically, only the lungs are infected; if other organs are infected, the disease is referred to as disseminated histoplasmosis and can be fatal if left untreated. The disseminated disease is more commonly seen in individuals who have cancer, AIDS, or are otherwise immunocompromised. In the United States, histoplasmosis is most common in the eastern and central states. Positive skin tests may be common in up to 80% of the endemic population of these areas. Prevention is possible by wearing appropriate personal protective equipment.
Special Considerations: LIFESPAN
Histoplasmosis
Very young children and older men are most likely to contract histoplasmosis, and they are especially susceptible to the form that spreads (disseminates) from the lungs to other body parts.
Signs and Symptoms
Many infected individuals have no obvious symptoms. Respiratory symptoms, such as chest pains, dry cough, or nonproductive cough, may develop. Many people are infected with the disease without knowing it because symptoms are so mild. Most people recover after a few weeks. Histoplasmosis can resemble tuberculosis. Chest x-rays typically show a distinct pattern. The lungs become inflamed because of invasion by foreign material, which damages the lymph glands and lungs. In more severe cases, weight loss and weakness occur, requiring a very long convalescence. In the chronic form, the disease spreads throughout the body, causing weight loss, bleeding, and other severe problems. Scar tissue and calcium deposits may form. Occasionally, histoplasmosis is fatal.
The fungus may be identified by isolation in culture and, occasionally, both sputum and urine must be cultured. A skin test, administered intradermally, can indicate the presence of the fungus.
Treatment
In the disease’s mild form, treatment is similar to that for the flu. Usually, symptoms clear by themselves. In more severe cases, amphotericin B (Fungizone) or another antifungal medication is given IV for several weeks.
Tuberculosis
Tuberculosis (TB), an infectious disease, is caused by the acid-fast bacillus Mycobacterium tuberculosis. This organism encases itself in a waxy coating (spore) that makes its destruction difficult. When found in the lungs, the bacilli are encased in a lump called a tubercle. The tubercle (known as the primary lesion or primary TB) may remain inactive for life. Many people have tubercle bacilli in their bodies, but do not actually have active TB. Active TB develops when disease, poor nutrition, stress, or a multitude of other factors lower the person’s resistance. The organisms multiply and become active. It is possible to stop the destructive progress of the disease to the point where it is not infectious and remains inactive.
Tuberculosis spreads by inhalation of infected droplets that a person with an active infection releases into the air. Physical contact with an infected person and contact with contaminated utensils or equipment can spread TB. The tubercle bacilli most frequently attack the lungs, but the blood can carry the organisms to other body parts, including the kidneys, spine, brain, and the bones.
Persons with the following conditions or status and who have compromised (weak) immune systems have an increased risk for TB infection:
• HIV (coinfection with TB)
• Substance abuse
• Chronic renal failure
• Infants, youth, or advanced age
• Immunosuppression from steroids or cancers
• Diabetes mellitus
• Unclean living conditions or crowded living conditions with one or more occupants having TB
• Homelessness
• Poor diet
• Immigrants from parts of the world with endemic tuberculosis
Key Concept The number of cases of TB has increased dramatically during the last several decades because of the increase in multidrug-resistant TB organisms, increasing numbers of persons with HIV infection, substance abuse, homelessness, and poor compliance with medication treatment plans. Healthcare workers must maintain diligence and use appropriate personal protective equipment (e.g., specialized masks) when working with known or suspected respiratory diseases such as TB.
Types
Latent and Active TB. For most individuals who inhale TB bacteria and become infected, the body’s defense mechanisms surround the bacteria to prevent it from growing and spreading. The bacteria remain in a dormant spore state (alive but inactive). This condition is called latent TB infection.
Typically individuals with latent TB:
• Have no symptoms
• Do not feel sick
• Are not infectious to other individuals
• Usually have a positive skin test reaction
• Can develop active TB disease if they do not receive treatment for latent TB infection
For most individuals in the United States and Canada who have latent TB, the TB bacillus remains inactive for a lifetime without causing disease.
Active TB occurs if the individual’s defense mechanisms become weakened, at which point the body may not be able to control and segregate the TB spore. When the capacity of the body’s defense mechanisms is compromised (weakened), the TB bacillus will start to grow, invade, and destroy tissues, especially the lungs. Latent TB commonly becomes active TB in individuals who are immunocompromised.
Pulmonary Tuberculosis. When the bacillus enters the lungs, it precipitates an infection called pulmonary TB. It may be so mild that it produces no symptoms, in which case the infection clears and the person is unaware that he or she was infected. However, the tuberculin test is positive, and a CXR will reveal a small scar, a sign that at some time the bacillus was active, but now is considered latent TB. The scar is the result of efforts of the white blood cells to surround and destroy the bacilli. Active TB will result if the person’s resistance is lowered. The capsule enclosing the tubercle breaks down and the bacilli spread and cause active illness.
Pott’s Disease and Miliary Tuberculosis. Tuberculosis of bones and joints is another form. Should the bloodstream carry bacilli to the spine, the resulting disease is called Pott’s disease. The vertebrae collapse, and there is pronounced spinal curvature (kyphosis or humpback). This disease rarely occurs in the United States or Canada today. Seeding by the bloodstream may carry the bacilli to other bones and joints, especially the hips and the knees. If disease spreads throughout the body, it is called miliary TB.
Infection may spread to the oviducts, ovaries, and uterus; surgical removal of the diseased organ may be required. The gastrointestinal tract, the kidneys, and the meninges are other possible sites.
Atypical Tuberculosis. Atypical TB is often spread to individuals who are immunosuppressed. Coinfection with HIV has become more common because of the increased numbers of persons infected with HIV. It may also occur in the person undergoing chemotherapy or radiation treatment for cancer. Atypical TB is highly resistant to treatment.
Multidrug-Resistant Tuberculosis. Multidrug-resistant TB is on the rise. In a small percentage of cases, the treatment regimen does not successfully eliminate the TB. This may be owing to the client’s noncompliance with the medication program, the medication may not be absorbed properly, or the individual may have contracted TB from a person with multidrug-resistant TB. This type is very difficult to treat. The individual will remain on different medications for a much longer period.
Signs and Symptoms and Diagnosis
Tuberculosis usually develops slowly. Signs and symptoms of pulmonary TB include:
• Cough
• Lack of pain (presence of pain may indicate extension to the pleura)
• Thick sputum (possibly blood streaked)
• Expectoration of blood (indicating pleural hemorrhage)
• Positive or negative sputum culture
• Fatigue
• Gradual weight loss (may lead to emaciation, if not treated)
• Low-grade fever, especially in the afternoon
• Nocturnal diaphoresis (profuse sweating at night)
• Severe chest pains, persistent cough, and dyspnea as disease progresses
IN PRACTICE :IMPORTANT MEDICATIONS 86-1
DRUGS OF CHOICE FOR TUBERCULOSIS (TB)
There are several approved drugs for treating TB, including the core drugs listed below. The initial phase is 2 months, which is followed by a continuation phase of 4 or 7 months.
• isoniazid/INH (Nydrazid, Laniazid)
• ethambutol (Myambutol)
• pyrazinamide/PZA (PMS Pyrazinamide, Tebrazid, Zinamide)
• rifampin (Rimactane, Rifadin)
• streptomycin
The tuberculin skin test may indicate the presence of the tubercle bacillus in the body, but the positive test result is not necessarily an indicator that the person has active TB. In conjunction with preliminary tuberculin tests, CXR and positive sputum cultures for the tubercle bacillus are the most reliable means of detecting pulmonary TB.
Treatment
Medication therapy is the specific treatment for active TB, regardless of the organ involved. The goal of medication therapy is to arrest the growth of the bacillus so that natural body defenses (leukocytes and antibodies) can take over and eliminate the disease (In Practice: Important Medications 86-1).
Tuberculosis infection is usually treated with isoniazid (INH) alone because it is quite effective. INH has few toxic effects, although in rare instances it has been known to cause anemia, neutropenia, gastrointestinal distress, and hepatitis. In combination with other medications, INH is prescribed in almost all cases of TB disease. Rifampin is highly effective in the treatment of TB as well; however, it is more toxic than INH and much more expensive. Ethambutol is usually given with INH and has low toxicity. Vitamin B6 is commonly given with INH in the treatment of TB to prevent peripheral neuropathy.
Special Considerations: LIFESPAN
Tuberculosis
The initial treatment of tuberculosis in children and pregnant women will be with INH alone for 6 to 9 months. Sputum cultures must be followed up closely.
The regimen for medication administration is important and must be followed faithfully. It may be necessary to treat the client with two to four medications for a period of 6 to 12 months. Treatment time may be longer for immunosup-pressed individuals, possibly taking as long as 2 years for those with drug-resistant TB.
Surgical procedures include total pneumonectomy (removal of an entire lung), partial pneumonectomy (removal of the affected part of a lung), lobectomy (removal of a lobe of a lung), and wedge resection or segmental resection (removal of one or more bronchopulmonary segments). Because effective medications are now available, surgery is rarely necessary.