COMMON SURGICAL TREATMENTS
Thoracentesis
Thoracentesis involves puncturing the chest wall to remove excess fluid or air from the pleural cavity. It is done for diagnostic purposes or to relieve breathing difficulties in clients with TB, cancer of the lung, pleural effusion, pulmonary edema, and chest injuries. Using sterile technique, the physician inserts a trocar (large needle with obturator, a guide) into the pleural cavity. The obturator is removed, and fluid is withdrawn. The specimen is collected in a sterile container and measured. The specimen is then sent to the laboratory for analysis. The fluid is considered contaminated, and appropriate infection control measures should be taken.
IN PRACTICE: NURSING CARE GUIDELINES 86-1
ASSISTING WITH POSTURAL DRAINAGE
• Always wash hands. Rationale: Handwashing helps prevent the spread of infection.
• Always wear gloves and handle all soiled tissues as contaminated material. Rationale: This client may be infectious. Observe Standard Precautions.
• Explain to the client why the head-downward position is necessary for much of the treatment. Rationale: This position may be uncomfortable, but if the client understands the reason, he or she will be more likely to cooperate.
• Improve drainage by striking the client between the shoulder blades with cupped hands (pummeling) or by vibrating the client. Rationale: These techniques help to loosen the secretions. Be sure to receive instructions in these techniques.
• Have tissues available. Rationale: The person will probably cough up secretions.
• Have pillows and pads available. Rationale: The various positions are easier to assume if a movable bed and pillows are available.
• Perform this procedure before the person eats. Rationale: The client may gag, choke, or vomit. Performing postural drainage before eating helps to prevent vomiting and aspiration.
• Give the client oral hygiene following the procedure. Rationale: The stagnant or infected mucus may have a foul taste and odor.
• Dispose of all materials properly and wash hands. Rationale: Proper disposal of materials and handwashing help reduce the risk of infection transmission.
• Document the procedure and the client’s reactions. Rationale: Documentation provides for communication and continuity of care.
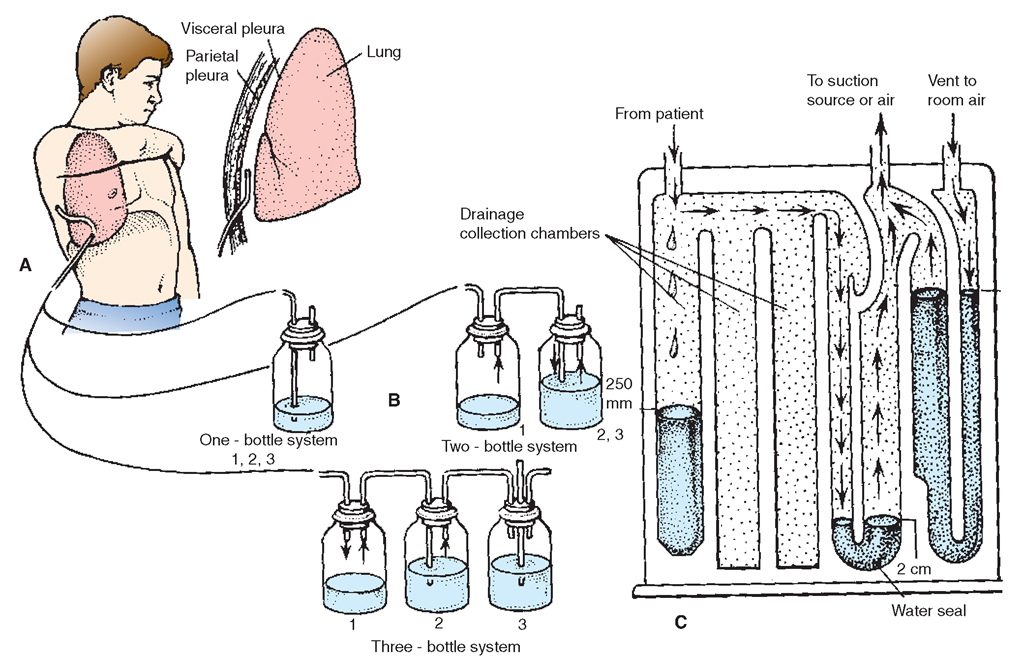
FIGURE 86-2 · Chest drainage systems. (A) Strategic placement of a chest catheter in the pleural space. (B) Three types of mechanical drainage systems. (C) A Pleur-Evac operating system: (1) the collection chamber, (2) the water-seal chamber; and (3) the suction control chamber The Pleur-Evac is a single unit with all three bottles identified as chambers.
Throughout the procedure, assist the client and offer support. The procedure is similar to abdominal paracentesis.The person will be most comfortable in a sitting position while leaning on a padded overbed table. The physician will need very little assistance, but the client will need considerable emotional support.
Nursing Alert Because a thoracentesis is an invasive procedure, the client must sign an informed consent before it can begin. Watch the client carefully after the test for signs of fluid leakage or infection. A rare but serious complication is pneumothorax (accumulation of air in the pleural space). Clients may have some pain, which analgesics can usually relieve.
Be sure to watch for respiratory depression when clients are receiving medications.
Generally, after the procedure, the individual can breathe more easily because the pressure of the fluid, which often causes respiratory distress, has been relieved.
Paracentesis
Paracentesis is defined as the puncturing of a body cavity for aspiration of fluid; however, this process most commonly refers to puncture of the abdominal cavity. Abdominal distention caused by excess fluid immobilizes the diaphragm and interferes with breathing. Therefore, removing fluid from the abdomen can relieve breathing difficulties.
Nursing Alert A large amount of fluid withdrawn (>1,000 mL) during paracentesis or thoracentesis can result in vasodilation and hypovolemia (decreased circulating fluid volume). These situations can cause syncope (temporary loss of consciousness, fainting) and shock. Take the client’s blood pressure and pulse immediately after paracentesis or thoracentesis and every 15 minutes until readings are stable and within acceptable levels.
Thoracotomy
Lung surgery is done through a thoracotomy, an incision into the thorax or chest cavity.
Caring for the Client After Chest Surgery
Teach the client deep-breathing techniques, as well as range-of-motion (ROM) exercises, before chest surgery. The extent of the client’s participation in postoperative care will directly reflect the quality of preoperative instruction given. Postoperative exercises can be vital to recovery and help prevent complications.
IN PRACTICE :NURSING CARE GUIDELINES 86-2
CARING FOR THE PERSON WHO HAS HAD CHEST SURGERY
• Always wash hands and wear gloves. Rationale: Handwashing and gloves help to prevent infection transmission.
• Turn the client often. Rationale: Turning helps to facilitate drainage and prevent hypostatic pneumonia and other complications. The wound will drain the most when the client is lying on the affected side; however, because this can be uncomfortable, coordinate turning to this side with the time when the pain medication effectiveness is optimum.
• Be sure the client turns and coughs and uses the incentive spirometer as ordered. Rationale: These actions help to prevent stasis of secretions.
• Monitor for signs of dyspnea, changes in rate of respiration, cyanosis, increased heart rate, chest pain, restlessness, orthopnea, or hemoptysis. Rationale: These symptoms could indicate that the chest suction is malfunctioning.
• Help the client to sit comfortably in the chair while the chest suction is operating. Rationale: Getting the client out of bed helps to minimize the risk for developing complications, in particular, respiratory complications. Sitting in the chair helps to promote lung expansion.
• If the client is up walking with tubes and drainage bags or bottles, be sure that the hemostatic clamps go along. Rationale: The client must always be within reach of the clamps in case of accidental dislodgement of tubes.
• Make sure the client is passing flatus rather than having gas pains or distention difficulties. Rationale: Abdominal distention can cause difficulty in breathing and extreme discomfort.
• Encourage ambulation and exercise. Rationale: Ambulation and exercise help the client recover more quickly and decrease any risks of complications.
• Maintain a level of comfort acceptable to the client, so that deep breathing and coughing can and will be done. Rationale: Ease of breathing enhances the client’s ability to comply with treatment.
Provide routine preoperative and postoperative care (In Practice: Nursing Care Guidelines 86-2).
The immediate postoperative concern for the person who has had lung surgery is to maintain an adequate airway. Direct care at preventing respiratory complications.
Record vital signs frequently; turn the client often to prevent complications of immobility. Encourage the client to breathe deeply and to cough at least every 2 to 4 hours and to use the incentive spirometer. Coughing is easiest if the person is in an upright position and he or she splints the incision with a pillow.
The client must exercise soon after surgery because many muscles are incised during chest surgery, and function must be restored; exercise also prevents complications related to immobility. Carry out passive ROM exercises for the client; within a few days he or she should be able to participate actively in ROM. Full ROM exercises, including isometric (muscle-setting) exercises, must be provided for the shoulder and arm on the operative side; these exercises may be initiated immediately following surgery. Discontinue any exercises that cause pain or great resistance. Do not overextend or overtire the client’s muscles.
Nursing Alert If a person with any disorder of the respiratory system is receiving a narcotic, be particularly watchful for respiratory depression. Depressed respirations can be an undesirable side effect in anyone, but the situation is most dangerous for the client whose respiratory function is already compromised.
Chest Suction. Following most types of lung surgery, the client will have large catheters called chest tubes inserted into the chest cavity and attached to suction. The breathing mechanism of the lungs works because the pressure of the chest cavity is lower than the pressure of the air outside the lungs. This negative pressure creates a vacuum, which causes air to rush into the lungs and keep them inflated. After the chest cavity has been opened, a vacuum must be created within the chest to re-establish negative pressure. The purpose of suction is to restore the negative pressure within the chest cavity and reinflate the lungs or to prevent loss of negative pressure and keep the lungs inflated. In addition, secretions and blood that may have accumulated in the chest cavity must be removed.
Closed Water-Seal Drainage. The most common method of re-establishing negative pressure is by closed water-seal chest drainage. In this procedure, one or more catheters are inserted into the chest cavity. If more than one catheter is inserted, each may be connected to a separate suction setup, or they may all be joined and attached to one suction setup.
Nursing Alert Maintain the integrity of the suction apparatus and water seal at all times. Refill the water chamber if the fluid level gets low. Report at once any client who complains of severe pain or dyspnea. If a bottle or connection breaks, the closed system will be disrupted, and this is an emergency! Clamp the chest tubes immediately and summon help.
The water-seal drainage system must remain closed (airtight) so that no air is allowed to enter the chest cavity; otherwise, the lungs collapse. By putting the drainage tubes under water, air is prevented from backing up into the chest. One widely used apparatus of disposable chest drainage systems is called the Pleur-Evac (see Fig. 86-2C).
This system comes assembled and sterile with instructions for use. It can be connected to suction and provides a water seal. When the chamber is full of blood, it is discarded and replaced with a new one; this is done only by a trained professional.
Nursing Implications. Monitor the client closely for signs of shock, dyspnea, pain in the chest, or a rapid increase in chest tube drainage, and report these symptoms immediately. Rationale: The most serious postoperative complications are hemorrhage into the lung cavity (hemothorax) or collection of air in the pleural cavity, causing collapse of all or part of a lung (pneumothorax). In hemothorax, the fluid (blood) collects in the lower part of the pleural cavity. In pneumothorax, the air rises to the top. In Practice: Data Gathering in Nursing 86-1 highlights danger signs for a person with a chest tube. In Practice: Nursing Care Guidelines 86-3 outlines care measures.
IN PRACTICE :NURSING CARE GUIDELINES 86-3
CARING FOR THE PERSON WITH CHEST SUCTION
• Always wash your hands and wear gloves. Rationale: Handwashing and gloves help to reduce the risk for infection.
• Never attempt to set up any chest suction without assistance. Rationale: In most facilities, at least two people must check a suction setup before it can be connected to the client. This is a safety precaution.
• Never disconnect or change chest suction without being absolutely certain about what to do. Rationale: The person’s life depends on the ability to maintain the integrity of the pleural space.
• Never disconnect chest tubes! Rationale: These tubes provide the suction that keeps the lungs inflated. If they are disconnected, the lungs will collapse.
• Keep clamps or hemostats with the client, either clipped to the bedding or to the client’s gown (when using the three-bottle system). With the disposable system, a clamp is attached with the tubing. Thus, additional clamps are not necessary If the client gets out of bed, the clamps go along. Rationale: The tubes are clamped as an emergency measure in case the tubes become accidentally disconnected.
• If the tubes become disconnected, double-clamp all tubes close to the chest wall and summon assistance immediately Rationale: This is an emergency situation requiring prompt intervention. If air enters the chest cavity, the person’s lungs will collapse!
• Be aware that clamping chest tubes for more than a few minutes may cause a tension pneumothorax. Rationale: If any untoward symptoms occur, call for help immediately.
• Never empty drainage in a closed system. Note the amount as ordered. Discard the entire system when full. Rationale: The integrity of the closed system must be maintained to prevent lung collapse.
• Never use pins to fasten the tubes to the bed. Rationale: A pin might puncture the tube.
• Never change a chest dressing. Rationale: The dressing may help maintain the integrity of the chest wall.
• Never take the plugs out of the bottles without assistance and never pull on chest tubes. Rationale: These actions may result in air entering the chest cavity.
• Tape all connections to make sure they are airtight. Rationale: Taping connections reduces the risk that the tubes may become disconnected.
• Keep in mind that chest tubes do not need to be stripped (cleared) unless there are clots or very thick drainage. In this case, stripping the tubes may be necessary to maintain patency Hold the tube in place while stripping or milking it, stripping no more than 7 to 9 inches at a time, using short strokes rather than one long stroke. Rationale: Holding the tube between the hands and the client’s chest prevents pulling on the tubes and possibly displacing them. Using short strokes helps to prevent possible tearing of the pleura.
• If a chest tube becomes kinked, report it immediately Rationale: Kinking could disrupt the system and prevent drainage.
• To set up the drainage after the tube is inserted, wrap a piece of cloth tape around the tube and then attach the tape to the edge of the bed, so the tube hangs straight down into the bottle. Keep the remainder of the tubing in the bed with the client. Rationale: Straight drainage provides the best drainage flow. The excess tubing allows the client to turn in bed and move about.
• Be sure the client does not lie or pull on the tubing. Rationale: This might obstruct the flow of the drainage.
• Keep drainage containers lower than the level of the client at all times. Rationale: This position facilitates drainage and prevents backflow.
• If possible, use the disposable closed system instead of the bottle system. The bottle system is rarely used today. Rationale: The plastic container is much less likely to break, and the tubes are more secure in the drainage container.
• Observe and report accurately Notify the healthcare provider if there is a marked change. Rationale: The amount, color, and consistency of the drainage are vital information.
• Observe for excessive bleeding or for abrupt absence of drainage. Rationale: Hemorrhage is a dangerous complication, and abrupt absence of drainage often means that the system is not operating properly.
• Document any changes in respiratory status, or respiratory distress, and any milking of the tubes. Rationale: Documentation provides for communication and continuity of care.
• Put a piece of tape on the drainage bottle to indicate the fluid level, and record the level of the drainage, as ordered. Rationale: The tape identifies the level of drainage, allowing output to be determined.
• Discard all drainage tubes and other equipment as required by Standard Precautions. Rationale: Proper disposal of equipment helps prevent the spread of infection.
NURSING PROCESS
DATA COLLECTION
Carefully observe the client with a respiratory disorder for changes in respiratory status. Document abnormal findings and notify the charge nurse and/or the healthcare provider of changes that indicate potential respiratory difficulties, such as dyspnea, tachycardia, tachypnea, or skin color changes. Because adequate oxygenation is vital to life, a disorder in the respiratory system can quickly become life threatening. An initial nursing observation with documentation establishes a baseline for future comparison and determines the presence of suspected complications. Report any changes in the baseline level.
When monitoring and charting a client’s respiratory status, note the client’s breathing and oxygenation level (see In Practice: Data Gathering in Nursing 86-2).
In addition, observe the individual’s emotional response to the disorder or disease. Does the client need assistance to meet daily needs? Does the disorder affect social activities or self-esteem? Is the person anxious or fearful about the outcome?
IN PRACTICE: DATA GATHERING IN NURSING 86-1
DANGER SIGNS FOR A PERSON WITH A CHEST TUBE
Be alert for the following:
• Leakage of air into the drainage system, whether in a simple water-seal type or a mechanical suction type, is indicated by constant bubbling in the water-seal system or bottle, after the client’s lungs initially have been expanded. There will be bubbling in the control bottle—the one connected to suction. If bubbling in the control bottle stops, the suction pressure is too low.
• Air leaks can occur at the chest tube insertion site, in connections, in the bottles, or in the stoppers in three-bottle suction; or in the closed drainage system itself.
• To check the location of an air leak, pinch the tubing for a few seconds at intervals between the chest tube and drainage connection. If the bubbling stops, the air leak is due to the system (check all connections). If the bubbling continues, pinch off tubing at intervals between the client and the system; when the pinching is between the source of the air leak and the water chamber the bubbling will stop.
• Keep all tubes, bags, and other devices below the level of tube insertion. Rationale: This position prevents reflux.
• If the client shows signs of cyanosis or dyspnea, or complains of chest pain, investigate the situation immediately This is an emergency!
Noting Alterations in Respiratory Status
Various events, such as illness or injury, can alter a client’s respiratory status. Table 86-1 lists possible alterations from eupnea (normal breathing).
Aspiration. Pathologic aspiration is the inhalation or movement of fluid, mucus, or another unwanted substance into the lungs. It can cause lung disorders or death.
Hyperventilation. In hyperventilation, the person breathes abnormally quickly or deeply, resulting in too little carbon dioxide in the blood.
IN PRACTICE: DATA GATHERING IN NURSING 86-2
THE CLIENT WITH A POSSIBLE RESPIRATORY DISORDER
• Note respiratory rate, depth, and character
• Determine respiratory status
• Observe for signs of respiratory distress, dyspnea, or poor oxygenation
• Be alert for signs or symptoms of hypoxia (lack of oxygen)
• Note any symptoms, such as cough, hemoptysis, cyanosis
• Listen to lung sounds and breath sounds
• Check results of skin tests related to tuberculosis or other lung conditions
• Observe mouth and throat by visualization and palpation
BOX 86-1.
Signs and Symptoms of Hypoxia
• Short of breath on exertion
• Tachycardia
• Mild increase in blood pressure
• Cool, moist skin
• Confusion
• Delirium
• Difficulty in problem solving
• Loss of judgment
• Euphoria
• Unruly or combative behavior
• Sensory impairment
• Mental fatigue
• Drowsiness
• Cyanosis
• Stupor and coma (late)
• Hypotension (late)
• Bradycardia (late)
The usual cause is anxiety or overexcitement. The hyperventilating person may have muscle spasms, dizziness, or faintness because of excessive oxygen and the depletion of carbon dioxide in the body. The easiest treatment is asking the client to breathe into a bag. The air the client rebreathes will contain excess carbon dioxide, replacing that which was lost.