PREOPERATIVE NURSING CARE
Before surgery, the surgeon or anesthesiologist writes orders indicating exactly what medications and physical preparation the client needs. In most cases, this preoperative preparation is carried out at home. It is important to teach the client to carry out preoperative orders exactly, because they affect the surgery’s success. While teaching preoperative care, remember the feelings of the client and family and their need for reassurance. Many clients are admitted to the healthcare facility the day of surgery and often will not arrive on a nursing unit until the surgery is completed. In emergency surgery, the preoperative period may be very short. Within these constraints, remember to provide emotional support to all clients.
Key Concept It is important to keep in mind the hierarchy of basic human needs, as defined by Maslow, when performing pre- and postoperative nursing care. The physiologic needs (e.g., oxygen, food, water elimination, sleep) must be met first to sustain life. Much of the immediate postoperative care is concerned with these physiologic needs. During the perioperative period, the nurse can help the client to feel safe and secure with empathic teaching and support. The client’s friends and family can assist the client to feel loved and cared for Finally the client is encouraged to participate in his or her own care as much as possible, to enhance self-esteem and self-actualization.
Nursing Alert In most instances, the client is instructed to stop taking aspirin, ibuprofen (Motrin, Advil), and other nonsteroidal anti-inflammatory drugs (NSAIDs) or any specific agents affecting blood coagulation for at least 7 to 14 days before surgery to reduce the risk of excessive bleeding. Certain herbal supplements are mild anticoagulants and they can also contribute to the risk of bleeding. These include camomile, cat’s claw, feverfew, garlic, ginger, ginkgo, ginseng, goldenseal, grape seed extract, green tea leaf, horse chestnut seed, and turmeric. The preoperative client usually is advised to stop taking these herbal supplements as well.
Preoperative Checklist
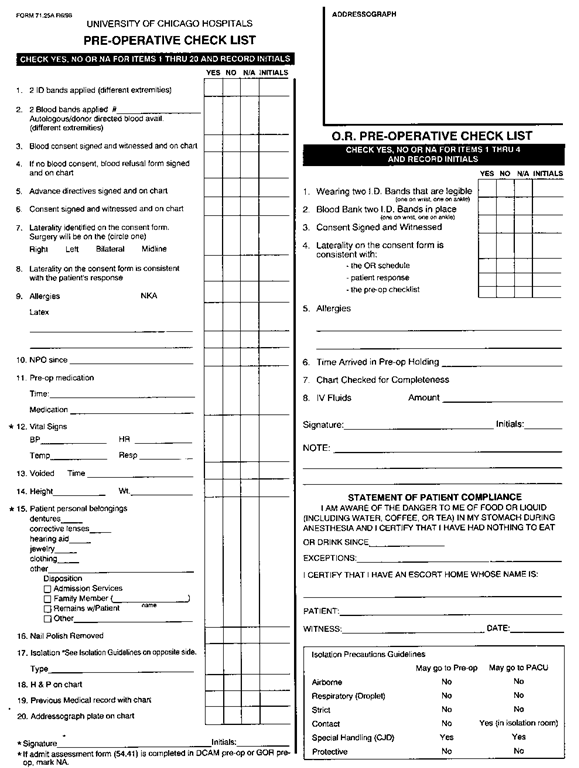
Each healthcare facility has a preoperative checklist to use in the care of all clients requiring surgery and certain other procedures, such as electroconvulsive therapy (ECT). This checklist identifies assessments, medications, and other physical preparations that must be completed before the client is anesthetized. Be sure that all items are checked off before the client is transported to the surgical suite. The list may be shortened if ambulatory surgery is done or if the client is to have a local anesthetic. In Practice: Nursing Care Guidelines 56-2 discusses the organization of preoperative nursing care and lists items regularly included in the checklist. Figure 56-2 shows an example of a paper preoperative checklist. This checklist can also be a part of the computerized client record.
Nursing Alert Be sure the client has signed the operative permit before giving any presedation medications. The client is not considered to be responsible after being medicated and cannot legally sign the operative permit. If the permit is not signed before medication is given, the surgery must be postponed. Obtaining the client’s permission for surgery is the responsibility of the surgeon; the nurse double-checks to make sure this has been done. Remember the concept of informed consent; the client must understand what is being done and why The client and/or family must be able to verbalize the type of surgery being done, and this statement must agree with the records and consent forms.
Nursing Alert If surgery must be cancelled because of an error, such as inappropriate or incorrect signing of the operative permit or the absence of ID name bands, this is considered a sentinel event and must be reported and investigated.
Preoperative care must be performed correctly and completely, and checklist items must be documented accurately. A preoperative goal is for the client to be in the best possible physical and emotional condition for surgery. A well-prepared client is more likely to have successful surgery and an uneventful course of recovery, leading to optimum rehabilitation. Remember that nearly all routine preoperative preparation is done at home before surgery. The client must be carefully taught all necessary procedures and their underlying rationales.
Key Concept Each step in preoperative preparation has a purpose. If any steps are omitted, the clients safety is jeopardized. The client will perform many of these steps at home if being admitted on the day of surgery It is the nurse’s responsibility to interview the preoperative client to make sure all steps in the preoperative preparation have been completed.
Nursing Alert All clients coming to a short-stay or day surgery unit must provide the name of a responsible adult escort or driver to take them home. If the client does not have an escort, most types of surgery will be cancelled. Rationale: It is not safe for a person to drive for at least 24 hours after anesthesia. Judgment and reaction times are impaired by the medication.
Client and Family Support
The client who faces surgery may be apprehensive. Most people fear pain. Some are concerned about losing consciousness; others are afraid they will die. Some are fearful of cancer or of being disabled. The client who has had previous surgery may compare the previous experience with this one. If the previous experience was difficult, the client may be particularly frightened.
The client usually meets with the surgeon immediately before surgery, as well as the anesthesia personnel. The client or family may wish to speak with their spiritual advisor or with a facility chaplain. Help to arrange this meeting.
Preoperative Teaching
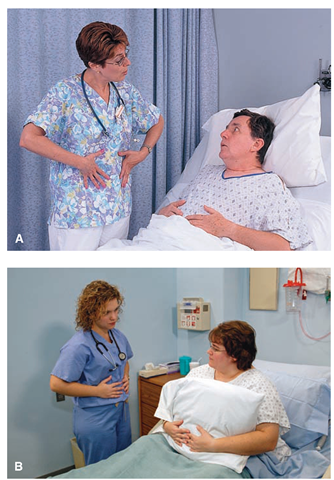
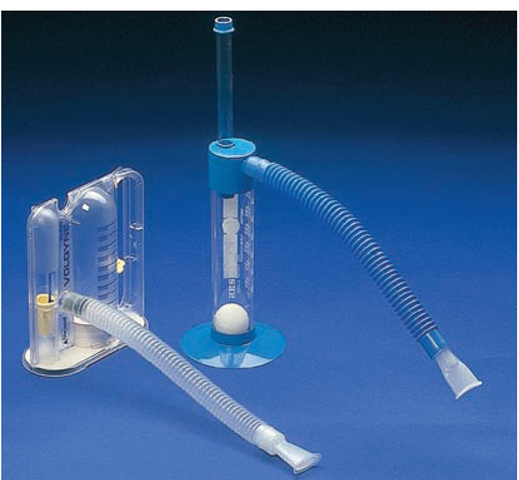
Explaining what will happen during and after surgery is most helpful in preparing the client and family. Those who understand these procedures are usually more relaxed and cooperative. Teach the client and family what to expect when the client returns from the OR. Explain about any equipment (e.g., a catheter, chest tubes, IV lines) or suction that might be present after surgery. Teach the client how to perform breathing exercises (Fig. 56-3) and how to use equipment such as the incentive spirometer (Fig. 56-4). Offer to tape the client’s wedding ring in place if it is not to be removed.
IN PRACTICE NURSING CARE GUIDELINES 56-2
ORGANIZING PREOPERATIVE NURSING CARE
General Measures
♦ Check the client’s record and note the preoperative orders.
♦ Make sure the client has completed any at-home preparation.
♦ Make sure the client has remained NPO (nothing by mouth) for the required length of time.
♦ Ensure that the client has signed the surgical permit and that it has been witnessed. Nursing students should not witness legal papers of any type.
♦ Determine if the client has an advance directive, such as a living will. If so, a copy of this document must be in the client’s record.
♦ Check for special forms. If there is a special situation, such as the client who refuses to receive blood, the client must sign a form to that effect, and this form must be in the client’s record.
♦ Prepare the operative area, as ordered. Usually the nursing staff is responsible only for supervising a shower with a prescribed antimicrobial scrub, if ordered. The actual surgical preparation and shave is usually done in the operating room.
♦ Keep in mind that in the event of brain surgery the client’s head may be shaved. Make sure that the client and family are aware of this beforehand. Let them know that the hair will be saved to make a wig if needed. In some cases, the eyebrows will be shaved or the eyelashes will be cut. The client needs to know what to expect.
♦ Check the client’s medical history for any essential respiratory cardiac, or other drugs he or she takes routinely Notify the physician of these medications. The client may need to take these drugs on the morning of surgery despite NPO status.
♦ See that all specimens and blood samples have been collected and sent to the laboratory
♦ Make sure that the history and physical examination are recorded in the client’s record.
♦ Check that results of all testing are on the chart; this includes laboratory tests, electrocardiogram (ECG), and sometimes a chest x-ray
♦ Give a sedative, if ordered.
♦ Withhold fluids and foods, as directed. Usually the client is NPO for at least 8 hours before surgery
♦ Make sure that client allergies are noted and that the client is wearing an “allergy” ID band, whether or not he or she has allergies. The client must also wear a facility identification band, usually on both wrists, to ensure proper identification.
♦ Give preoperative instruction and provide emotional support to the client and family
Immediately Before the Operation
♦ Check to make sure that the client is wearing his or her ID band. Ask the client his or her name as well. Surgery will be cancelled if the client is not properly identified.
♦ Record the client’s temperature, pulse, and respiration (TPR), blood pressure (BP), and the existence or absence of pain.Report immediately any deviation from normal to the surgeon.
♦ Determine and document the client’s fall risk status. If the client is a fall risk, a fall risk ID band must be worn, and this must be noted in the client’s record.
♦ Check that the client is wearing two special blood identification tags if the client has any possibility of receiving blood. The client’s blood must be typed and cross matched before surgery and this information must be in the client’s record.
♦ Make sure the client’s weight is recorded on the chart in pounds and kilograms. This helps to determine drug dosages.
♦ Help the client with bathing and other hygiene measures. Be sure the client removes all clothes before going to surgery and wears only a clean gown provided by the facility In some cases involving local procedures, the client may continue to wear street clothes. If clothes have been removed, carefully label them and store them in a safe place. If the client is to be admitted to the facility transfer the clothing to the new room.
♦ Ask the client to remove any prostheses, braces, splints, wigs, barrettes, bobby pins or hair pins, hair scrunchies, contact lenses, hearing aids, false eyelashes, and glasses. Make sure to check for jewelry in any body piercings; these items must be removed. If the client will be expected to participate, such as in brain or eye surgery hearing aids are usually left in place.
♦ Remove the client’s jewelry and valuables, itemize them, and put them in the vault or give them to the client’s family Be sure to include the client’s wedding band. If the client does not want to remove the wedding band, be sure to bind or tape the ring securely to the client’s hand. Carefully document what has been done with the valuables. If the client’s family takes valuables home, have them sign for the items.
♦ Help the client put on antiembolism stockings, if ordered.
♦ Help the client to void immediately before going to the Operating Room (OR). If the client is unable to void, report this and document it on the record.
♦ Pull the hair back and cover it with a surgical cap or a cotton towel if the client has long hair Hair should be washed the evening before surgery if possible.
♦ Remove any complete or partial dentures and place them in a denture cup with clear water Include removable bridges, retainers, and other dental appliances. Label the cup and its cover and put it in a safe place.
♦ Remove the client’s lipstick, makeup, and nail polish. Remove artificial nails, if possible. The anesthetist must be able to observe the client’s nail beds and lips. The oximeter sensor may not register properly if nail polish or artificial nails are present.
♦ Account for all items on the preparation checklist. Be sure the list is signed and attached to the client’s chart or entered into the computerized record. If a paper chart is used, be sure it is sent with the client to the OR. (This checklist must be completed by 6:00 am if the client is first on the OR schedule.) The nurse can carry out some procedures the evening before if the client is scheduled for early surgery and is in the facility overnight. In most cases, a nursing student is not allowed to do the final sign-off on the chart; learn the rules of the healthcare facility
♦ Help ensure the client’s safety by giving preoperative medications, as ordered, after completing all personal care and making sure that the checklist is completed and signed. The client must not be active or sign anything after taking a sedative.
♦ Be sure the side rails are up and the bed is in low position.
♦ Be sure that all preoperative charting is up to date and signed before the client goes to the OR.
♦ After the client goes to the OR, notify the Inpatient Unit so personnel there can begin to prepare the unit for his or her postoperative return. If the client will recover in a short-stay unit, prepare the recovery area.
Note: Some of the above procedures are done in the operating suite if the client is admitted to the facility the morning of surgery Many of these procedures are carried out by the client at home if the client will not be admitted to the hospital or if the client will be reporting directly to the Surgery Department on the day of surgery It is important to note that the time constraints are severe in preoperative nursing. The nurse must be efficient, but thorough.
FIGURE 56-2 · An example of a preoperative checklist. Often, this form is provided on the computer.
FIGURE 56-3 · Preoperative teaching is vital. (A) Teaching deep breathing.B) Teaching the client how to splint the incision with a pillow to minimize postoperative pain.
Key Concept Preoperative teaching is vital because clients go home so soon after surgery.
FIGURE 56-4 · Two types of incentive spirometers with spacers and mouthpieces.
Nursing Alert If a client will be on a ventilator or otherwise unable to speak after surgery make arrangements for a communication system. Allow the client to practice this system preoperatively
Explain preparation procedures to the client as they are performed, and tell the client how each step helps both client and surgeon. Preoperative teaching concentrates on several major points (see In Practice: Educating the Client 56-1 and Box 56-3).
To help prepare the family, explain that the client will be taken to surgery 30 to 60 minutes before the scheduled surgical procedure. In some cases, a family member can stay with the client in the preparation area until he or she is taken into the OR. Inform the family that after surgery the client will be taken to the PACU or PAR area, where specially trained personnel will observe the client until vital signs are stable and consciousness returns. If the family understands these procedures, they will be less upset by the length of time the client is gone. Inform the family where they may wait for news about the procedure. Usually, the surgeon speaks with the family immediately after surgery. If the client is to be transferred to another unit after surgery, the family must know where the client will be.
IN PRACTICE EDUCATING THE CLIENT 56-1
PREOPERATIVE INSTRUCTION
In the time available, perform as much preoperative teaching as possible. Remember that all teaching must be carefully documented.
• Explain the reasons for special equipment at the bedside.
• Describe what equipment is likely to be present for the client in the postoperative period.
• Describe and allow the client to practice how to turn in bed without assistance.
• Allow the client to practice all procedures, as needed.
• Describe discomforts to expect and how to alleviate them. Emphasize the use of medications to prevent pain, rather than waiting until pain exists.
• Show and practice with the client how to splint the incisional area (Fig. 56-3B).
• Demonstrate and allow the client to practice deep-breathing exercises (Fig. 56-3A).
• Explain the use of the incentive spirometer and allow the client to practice (Fig. 56-4).
• Demonstrate and practice other exercises to be performed postoperatively
• Describe the amount and kind of ambulation allowed or expected after surgery Explain the reasons for early ambulation.
• Provide a description of the Operating Room and the Postanesthesia Care Unit. Sometimes, especially for children, a preoperative tour of these areas is helpful.
• Describe appropriate wound care and show the client the supplies that will be used.
• Discuss optimum nutrition.
• Explain the importance of communication.
• Provide the client with written instructions to supplement the verbal instruction.
BOX 56-3.
Steps in Teaching a Client
♦ Organize your teaching.
♦ Explain what you are going to do.
♦ Demonstrate the procedure.
♦ Have the client return the demonstration; make sure that the family caregiver can also accurately perform the procedure, if required.
♦ Supervise the client’s practice until the client/caregiver can perform it independently.
♦ Reinforce successful behavior
♦ Review the procedure.
If you cannot answer a client’s questions or do not understand equipment that will be used, be sure to ask someone who is knowledgeable to help.
Nursing Alert Explain to the client and family where the family lounge is located. Make sure they know where to find food, coffee or soda, newspapers, computer access, and telephones. Suggest that they bring along something to do while they are waiting.
Gathering Data Preoperatively
Prompt, accurate gathering of information about the client before surgery helps to ensure a successful outcome for the client.
Observation
Observe the client carefully during preparation for surgery. Record any unusual reactions or observations in the client’s record and report them to the charge nurse or surgeon at once.