Assessing Fetal Well-Being
The well-being of the fetus is of utmost concern during the course of labor. The best indicator of fetal health is the fetal heart rate (FHR). The normal FHR is 120 to 160 beats per minute (bpm).
The frequency with which the FHR is evaluated should depend on the absence or presence of risk factors. FHR evaluation may be done using a fetoscope to perform intermittent auscultation; an electronic monitor may be used for continuous monitoring or periodic test strips. Electronic monitors can be used externally or internally. To permit internal electronic monitoring, the membranes must be ruptured.
Intermittent Auscultation. When there are no risk factors with the mother or the fetus, the standard practice is to evaluate and record the FHR at least every 30 minutes during Stage I, and at least every 15 minutes during Stage II. When risk factors are present, the FHR should be evaluated at least every 15 minutes during Stage I, and every 5 minutes during Stage II.
Key Concept The most important factor in fetal monitoring is the relationship between the fetal heart rate and the contractions of the uterus.
Electronic Fetal Monitoring. Continuous electronic monitoring of the FHR during labor is routine in many facilities. The purpose of the fetal monitor is to record the rate and quality of the fetal heartbeat during contraction and relaxation. It can give an early warning of fetal distress so that corrective measures can be started immediately. The nurse will periodically print out (run off) strips of the monitor’s graphic record and place them into the woman’s chart as part of the documentation of labor. Documentation of periods of distress is particularly important and needs to be placed in the permanent record (see In Practice: Nursing Procedure 66-1). An electronic fetal monitor is usually used in the following situations:
• If the fetus seems to be in distress
• If the delivery is being induced
• If the woman has a chronic health problem
• If a complication of pregnancy exists
External monitoring of the FHT is most commonly used. This approach is based on the Doppler effect, in which high-frequency ultrasound waves directed to the fetal heart bounce back to a transducer strapped onto the woman’s abdomen. The receiver amplifies the fetal heart sounds. The signal is converted to sound and is printed on electrocardiograph paper. In addition, a pressure-sensitive device, called a tocodynamometer, is used to monitor the frequency of contractions. When placed directly over the woman’s fundus (upper curve of the uterus), the device transfers an electrical impulse to the monitor, creating a readout. The tocody-namometer does not give information about the strength of uterine contractions. The relationship between the fetal heartbeat and uterine contractions can be studied because the information is printed simultaneously.
Advantages of external monitoring are that it is noninvasive, has no contraindications, and is easy to apply. Disadvantages include the need for frequent adjustments and its sensitivity to fetal and maternal movements.
If the external monitor’s printout signals a fetal or maternal problem, an internal or direct monitor is used because it is more accurate. An electrode, such as the scalp clip or spiral, is passed through the woman’s dilated cervix and carefully attached directly to the presenting part of the fetus. The internal monitor can provide precise information, including a fetal electrocardiogram. The external sensor may still be used to measure the frequency and length of uterine contractions, or a catheter (intrauterine pressure catheter) may be inserted into the uterus so that the intensity of contractions may also be measured.
The advantages of internal monitoring include a high-quality tracing and fewer artifacts (interference from other sources) than external monitoring. The disadvantages are that membranes must be ruptured, the cervix must be dilated, and the presenting part must be accessible.
Evaluation of Fetal Monitor Information. As a nursing student or licensed practical/vocational nurse, you most likely will not be responsible for the interpretation of electronic fetal monitoring. However, you should understand basic theory and terminology. Notify the team leader immediately if any signs of fetal distress appear on the fetal monitor, such as:
• Accelerations: Accelerations are brief increases of the FHR of 15 bpm or more. It is a sign of a healthy fetus for the FHR to accelerate after movement or stimulation. Any acceleration of 60 bpm or more is considered a complication, and the fetus may be in danger.
• Decelerations: Decelerations (slowing) of the FHR are categorized according to when they occur in relation to a contraction. Some decelerations are expected; others are warning signs of possible problems. An early deceleration begins early in the contraction, hits its low point at the peak of the contraction, and returns to baseline at the end of the contraction; it mirrors the contraction pattern. Early decelerations are caused by vagal nerve stimulation, resulting from pressure on the fetal head, and are considered a normal response of the fetus to labor. A late deceleration begins as the contraction eases, and lasts longer than the contraction—into the resting phase of the uterus. This is a sign of a possible problem and should be reported to your team leader.
• Decreased variability: Little to no fluctuation in the FHR on an internal electronic monitor tracing is a danger sign and may indicate an abnormality in the fetal nervous system. It might also indicate that the mother has taken or been given central nervous system depressants. Report this observation to the team leader for further evaluation.
Nursing Alert Variable decelerations in fetal heart rate occur anytime during or after contractions. They usually indicate umbilical cord compression and can usually be altered by changing the woman’s position or by giving her oxygen. Late decelerations begin late in the contraction, and the fetal heart rate recovery occurs after the contraction is over Decelerations are related to placental insufficiency and indicate fetal distress. The fetal heart rate should not fall below 100 bpm.
Nursing Care During Stage II
Maternal Care
Either a licensed practical nurse or licensed vocational nurse (LPN/LVN) or RN will assist in delivery. If you are assigned to assist during the birth, you most likely will help with the transfer to the delivery room (in a traditional labor and delivery suite) and then stand at the woman’s side, instructing her on how to breathe and when to push, and informing her of what is occurring. If you are assisting the birth attendant, you may be responsible for handing him or her necessary equipment, medications, and other items. If you are caring for the newborn, you will need to make sure that the infant is breathing and kept warm.
Aseptic conditions must be maintained during delivery. You and any of the woman’s support people will wear a clean scrub suit, a cap to cover your hair, and a mask.
If the client is going to deliver in a hospital delivery room, she is transferred on her bed and moved over to the delivery table, with the assistance of the circulating nurse. The table, which is split across the middle, is opened (broken), and the woman’s buttocks are positioned at the break in the table. Her feet are placed in stirrups simultaneously to prevent strain on the pelvic ligaments. Perineal preparation is done to cleanse the skin and to remove secretions from the genitalia. (Shaving is rarely done today.) In some cases, a birthing chair or squat bar is used.
Coaching the Client. In Stage II, the woman actively helps the birth process. As each contraction begins, she takes a deep breath, holds it, and then pushes with each contraction. Women often make grunting noises during pushing. If the woman relaxes between contractions, she can work better when the next contraction comes. Encourage the woman to push only with contractions and to rest between them.
If a woman tells you the baby is coming, you should trust her judgment. Get assistance immediately, and check for crowning. If a delivery occurs suddenly, without advance warning and aseptic preparation, it is called a precipitous delivery (this is different from a precipitous labor, in which fewer than 3 hours elapse from the onset of labor to birth). A client may “precipitate” in the labor room bed if her claim that birth is imminent is ignored. Encourage the mother to pant or blow forcefully when told not to push. Remember that only one person should give the woman instructions: during this challenging experience, too many different voices and directions can be overwhelming.
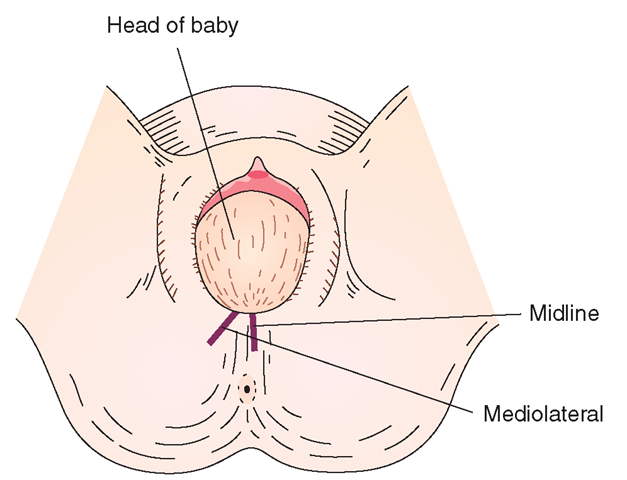
Episiotomy. Often the birth attendant makes an incision in the perineum, called an episiotomy, which enlarges the vaginal opening and allows an easier delivery of the fetus. Some birth attendants believe that episiotomy helps to preserve the structure and strength of the perineal muscles and prevents a jagged laceration or a tear extending to the anus. Other birth attendants believe that a laceration, should one occur, will be less extensive than the episiotomy. Extensive lacerations are difficult to repair and could leave permanent damage.
Note the type of episiotomy (midline, or right or left mediolateral), as well as any lacerations that occurred, on the woman’s chart (Fig. 66-5).
FIGURE 66-5 · Position of episiotomy incision in a woman during Stage II. The baby’s head is presenting to the vaginal outlet (crowning).
Neonatal Care
After the baby’s head is delivered, the birth attendant will check for any loops of cord that have become wrapped around the infant’s neck (nuchal cord) and remove them. Next, he or she will suction the nose and mouth of the newborn with a bulb syringe. The anterior shoulder is delivered, then the posterior shoulder and the remainder of the body. The newborn cries out, and the lungs expand. The time of delivery of the baby should be noted for legal records. This entire portion of the delivery often takes only a few seconds.
The baby may be handed to the mother immediately, before the umbilical cord is clamped. Assist the mother in placing the baby on the bare skin of her chest. Dry the baby, remove any damp towels or sheets, and cover the baby with a clean, dry cloth. Most babies calm quickly after experiencing the warmth of the mother and the security of her embracing arms. You should observe for the infant’s breathing pattern and suction the mouth if needed.
When the umbilical cord stops pulsating, two Kelly clamps are applied to it, and the birth attendant or baby’s father cuts the cord between them. An umbilical clamp is later applied near the baby’s abdomen. Make certain it is attached securely but does not pinch any skin folds. Some hospitals and birth attendants prefer that the infant be stabilized first in a radiant warmer. After the newborn is stable, the parents may hold the infant. However, healthcare personnel are responsible for the newborn’s care. Newborns must be kept warm, yet parents should have time to hold and to bond with them. Overhead warmers allow you to observe the newborn. Observations of the newborn include assessment of the Apgar score at 1 and 5 minutes of life.
For each delivery, a staff person skilled in neonatal resuscitation should be available to provide resuscitation if needed. If the infant is depressed or not fully responsive to stimulation, the neonatal resuscitation expert should be called immediately. Every minute is critical; never delay summoning help in the hopes that the baby’s condition will improve.
Nursing Care During Stage III
Stage III is relatively short, but may be a dangerous period for the mother because of the possibility of hemorrhage. The nurse should record the following information about the delivery of the placenta:
• The exact time the placenta was delivered
• Whether the placenta was delivered spontaneously or removed manually
• Which side of the placenta presented
After the placenta is delivered, an oxytocic medication may be administered to assist the uterus to contract and to minimize the risk of bleeding. You may be instructed to administer these oxytocics or to massage the fundus gently to minimize blood loss.
After the birth attendant has examined the cervix and vagina and sutured the episiotomy or lacerations, the vulva and perineum should be cleansed. If stirrups were used, remove the mother’s legs from them.
Key Concept Bring the mother’s legs down from the stirrups slowly and together Rationale: Doing so helps to avoid further trauma and discomfort.
Change the woman’s gown, apply perineal pads, and cover her with a warm blanket. Some healthcare facilities transfer women to a recovery room; in others, women recover in the room where they deliver.
Before the woman leaves the delivery or birthing room, complete the necessary documentation. Box 66-3 lists information required for the health record.
Nursing Care During Stage IV
Following delivery, the woman might feel chilled and shake uncontrollably, possibly in response to a cool room, sudden hormonal shifts, or the sudden change in intra-abdominal pressure after the fetus and placenta are expelled. Be sure she has several warm blankets available if needed.
BOX 66-3.
Necessary Documentation for Delivery
♦ Complete information about the type of delivery and procedures used; who was present
♦ Sex and condition of the baby (include Apgar score)
♦ Time of birth
♦ Time at which the placenta was expelled and presentation; indicate manual removal or spontaneous delivery
♦ Condition of the fundus
♦ Any medication administered
♦ If an episiotomy was done, and its type
♦ Condition and vital signs of the mother
♦ Measured maternal blood loss
♦ Any other events (e.g., maternal incontinence, infant resuscitation, perineal tears)
Many healthcare facilities have a recovery room where the mother and newborn are taken after delivery and where the mother and father can fondle and care for their newborn during the first hours. In some facilities, the newborn is first taken to the nursery for an initial admission examination and then returned to the recovery room. Others admit the newborn when the mother arrives in the postpartum area.
Immediately following delivery, the woman may experience extreme fatigue, close to exhaustion, just as she would after any extremely vigorous physical activity or hard work. At the same time, she is usually relieved and excited. She is usually interested in seeing and holding her newborn and having a visit with her partner. The bonding between parents and newborn should be encouraged immediately. Allow time for the family to be together as soon as possible. If both mother and infant are stable, you should provide the family with privacy during this time. Observe the mother closely for several hours after delivery for signs of complications. In addition, document any maternal complaints.
Observations and Data Gathering
Check the mother’s blood pressure and pulse at least every 15 minutes for the first 1 or 2 hours or until it is stable and then every half hour for 1 hour or longer. Usually after the first 12 hours, you will check vital signs every 4 hours for 12 hours and then every 8 hours if no difficulties arise.
When taking vital signs, also check the fundus of the uterus and the perineum. The reason for keeping a close check on the fundus is to ensure that it remains firm and contracted. If it becomes soft and boggy, hemorrhage could occur. Teach the mother to assess her own uterine fundus. If nursing measures are not effective, the physician may order administration of an IV or intramuscular (IM) oxytocic drug. Common oxytocic drugs are oxytocin (In Practice: Important Medications 66-1) and methylergonovine maleate (In Practice: Important Medications 66-2).
A rising fundus may indicate uterine hemorrhage. If the fundus does not become firm with massage, report this finding immediately. A fundus located to the right of the midline often indicates a full bladder. Voiding will usually return the fundus to its earlier location. If this does not occur, notify the team leader. Check the perineum to make sure the stitches are intact. Be sure no excessive bleeding, edema, or bruising is found.
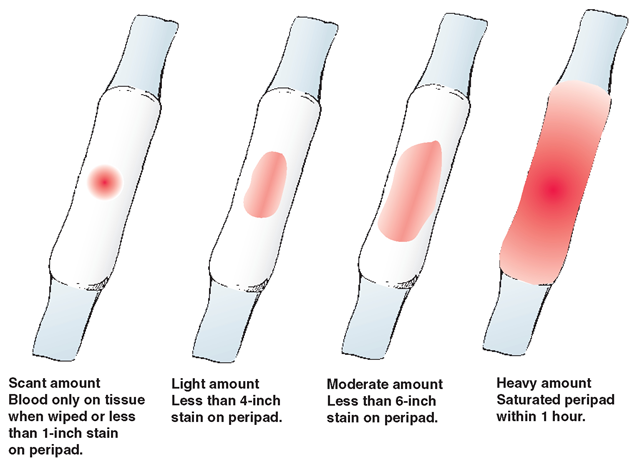
Lochia is the vaginal discharge that occurs following delivery. It consists of blood and the tissues of the uterine lining as it breaks down. Immediately following delivery, lochia is bloody and should be moderate in amount. While wearing gloves, check lochia during the immediate postpartum period. Observe the amount, character, and color. The amount is described as scant, light, moderate, or heavy; it should have a fleshy or metallic, never foul, odor (Fig. 66-6).
Observe and record the woman’s first voiding after delivery. Failure to void may indicate swelling or injury to the urinary system. Report if the woman feels the urge to void but is unable to do so or if the fundus shifts to one side. If she is unable to void within 6-8 hours after delivery, catheterization may be necessary.
Maternal and Newborn Feeding
The new mother may be thirsty and hungry after delivery. Encourage her to drink fluids to replace those lost during labor and delivery; she can have solid foods as tolerated.
IN PRACTICE: IMPORTANT MEDICATIONS 66-1
OXYTOCIN (PITOCIN)
Dose
Labor induction: Initial dose of 1-2 mU; increased 1-2 mU/min until an adequate labor pattern is achieved; maximum recommended dose is 20 mU/min
Labor augmentation: Initial dose: 0.5-1.0 mU; increased 1-2 mU/min until an adequate labor pattern is achieved; maximum recommended dose is 20 mU/min
Postpartum: 10-20 mU intramuscular (IM) or intravenous (IV) after delivery of the placenta
Expected effect: Used to initiate (induce) labor or augment labor contractions that are weak or ineffective; also used after the delivery of the placenta to contract the uterus
Adverse side effects
Mother: Unpredictable individual response; hypertonic uterine contractions; tetanic uterine contractions; cervical and vaginal lacerations; amniotic fluid embolism; water intoxication
Fetus: Fetal distress, birth injury
Nursing Considerations
• Contraindications to use: Any obstruction that would interfere with the descent of the fetus; hypertonic or uncoordinated uterine contractions; fetal distress; any contraindication for vaginal birth
• Amount and rate of administration must be carefully controlled; this can be done effectively only by use of the IV route, using an infusion pump.
• Type of solution, amount of oxytocin added, and rate of infusion vary according to agency protocols or physician preference.
• Evaluate fetal heart rate every 15 minutes when given during labor.
• To prevent water intoxication, give in electrolyte solution, avoid infusing high volumes of fluid, and avoid using high doses of oxytocin for prolonged periods.
IN PRACTICE :IMPORTANT MEDICATIONS 66-2
METHYLERGONOVINE MALEATE (METHERGINE)
Dose: 0.2 mg intravenous (IV), intramuscular (IM), or oral (PO) (IV only for emergencies)
Expected effect: Strong, persistent uterine contractions that last for hours
Adverse side effects: Hypertension is primary side effect; may also cause headache, some chest pain, palpitations, and dyspnea
Nursing Considerations
• Methylergonovine should never be given until the fetus and placenta have been delivered.
• Check the woman’s blood pressure before giving the medication; if elevated, do not administer this drug.
If the mother plans to breastfeed, encourage her to put the newborn to her breast in the delivery or recovery room. The newborn usually is alert at this time, and the stimulation of the breast encourages the secretion of natural oxytocin to contract the uterus.
Transfer From the Recovery Room
The mother remains in the recovery room or is closely observed in the birthing room long enough to ensure that her condition is satisfactory (usually 1 to 2 hours). When her condition is stable, she is transferred to a postpartum room if she delivered elsewhere.
Record complete information about the delivery and other procedures on the woman’s health record before she is moved. Check the charting from the delivery room and the recovery room to make sure the record is complete. Transfer this documentation with the woman (see Boxes 66-3 and 66-4).
FIGURE 66-6 · Determine the volume of lochia by peripad saturation.
BOX 66-4.
Necessary Documentation Regarding the Postpartum Woman
Assessment of the fundus:
• Firmness (consistency)—firm, boggy (and result of massage)
• At center or deviated (location)
• Height (position)
Height of the fundus. One possible way of documenting fundal position is shown below:
2/U = 2 finger widths over umbilicus 1/U = 1 finger width over umbilicus UU = fundus at level of umbilicus U/1 = 1 finger width below umbilicus U/2 = 2 finger widths below umbilicus
Lochia:
• Rubra, serosa, alba (character)
• Excessive, moderate, scant (amount)
• Odor