Additional Transmission-Based Precautions
In special cases, additional precautions may be necessary. The infection control committee will usually be involved in making this decision and in deciding what precautions are to be taken. Nurses will require special instruction before caring for these clients.
Key Concept Each healthcare organization has its own established local protocols for clients requiring additional Transmission-Based Precautions.
ISOLATION
Standard Precautions and Transmission-Based Precautions are the currently followed isolation guidelines. Historically, two primary types of isolation systems were used in healthcare: category-specific isolation and disease-specific isolation. Although Standard and Transmission-Based Precautions have replaced the routine use of these systems, some facilities still use them in addition to Standard and Transmission-Based Precautions.
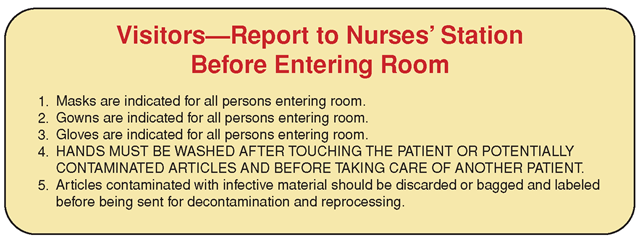
FIGURE 42-3 · An instructional card is placed on the door of the room of a client in a specific type of isolation.
In category-specific isolation, specific types of isolation (e.g., respiratory, contact, enteric, strict, or wound) are identified, using color-coded cards (Fig. 42-3). This form of isolation is based on the client’s diagnosis. The cards are posted outside the client’s room and state that visitors must check with nurses before entering.
Disease-specific isolation uses a single all-purpose sign. Nurses select the items on the card that are appropriate for the specific disease that is causing isolation.
Nursing Measures in Isolation
Setting Up a Client’s Room for Isolation
Clients who require isolation usually are confined to their rooms. The goal is to protect other clients, keep the client’s environment contaminated only to that client, and facilitate concurrent and terminal disinfection. All healthcare facilities have policies and procedures for isolation and for the use of specific PPE. Check the healthcare facility’s policies and procedures for specific measures to follow if the client needs to be brought out of the room for a treatment or test.
Education and Preparation
When setting up the client’s room, explain the isolation precautions to the client and family. They will need to understand the reasons for these preventive procedures. Explain that children are usually not allowed to visit a client with a disease requiring special precautions, because children are so susceptible to infection. Additionally, some children will not be able to follow the special instructions.
Barrier techniques and PPE may frighten clients, who may fear their disease and believe that others are afraid to come near them. These clients may experience loneliness and miss the companionship of others. Make every effort to visit and communicate with clients in isolation as much as possible. Organize your workload so you can remain in their room for longer periods. Even when you are not going into the room, stop by and say hello.
Special Considerations: LIFESPAN
Nursing Procedures in Pediatric Infection Control
A higher percentage of pediatric admissions involve communicable diseases than do adult admissions. Often, members of the pediatric population are not immune to such diseases. If such diseases are not contained, an outbreak can result. Keep in mind the following:
• Children are at greater risk of acquiring viral infections than are adults.
• Young children may not be able to understand good handwashing and barrier precautions; they require adult supervision.
• Environmental surfaces must be kept as clean as possible, because children may have physical and oral contact with them. Children may also put toys and other objects into their mouth. Some toys may be shared in playrooms. Shared toys must have cleanable surfaces. Stuffed animals and dolls usually are not permitted in the healthcare facility, because they cannot be adequately disinfected.
• Barrier techniques are important to employees who care for children because children require close contact (e.g., rocking, cuddling, and feeding).
Supplies
The client’s room is usually equipped with a bedpan and urinal; wash basin and soap dish; water pitcher and glass; emesis basin; toilet and facial tissues; toothbrush and dentifrice; and personal items, such as shaving equipment, comb, hair pick, and/or brush, deodorant, shampoo, and cosmetics. (Disposal of these items is necessary on the client’s discharge.) Provide the client with a telephone and television, if possible. Additional items include paper towels; plastic or paper bags to line the wastebasket for trash disposal; washable blankets, pillows, and bedspreads; and impervious laundry bags, as well as the usual linens needed for a client unit. A sink with foot or knee control and a covered linen bag and stand are ideal. This client should have a private bathroom and shower.
Items to place outside the client’s room or in an anteroom include a bedside stand or cabinet stocked with PPE as required for the client’s condition. A sink is usually available or nearby for handwashing. Hand sanitization materials must also be readily available. Other items include clean laundry bags, large trash bags, biohazard bags, and tape or tags and marking pens for marking contaminated bags. Healthcare facilities require a sign for the door; the sign will vary depending on the specific precautions the client’s condition requires.
Nursing Alert If you will be working in a pediatric unit, determine your immune status regarding the communicable diseases of childhood.You may require immunization to prevent exposure and infection. Some procedures may be slightly different in pediatrics.
Administering Medications in Isolation
Follow Standard Precautions when administering medications. Use and dispose of disposable materials in the client’s room. The following suggestions review general pointers for medication administration and add specific suggestions for clients in isolation.
• Unwrap medications, but take the packages with you when going into the client’s room. Rationale: Unwrapping will be difficult to do after you put on gloves. The client may question the medication; you will need the packages for reference.
• If you will need juice or applesauce in which to mix medications, take it with you into the room. If using a medication tray, be sure it is disposable.
• Do not take medication administration cards or records into the client’s room. It is safest to print out the medication administration record (MAR) take it into the client’s room, and dispose of it in there after giving the medications.
• If you are not going to give personal care to the client, you may only need to wear gloves and a mask, if required. Do not touch the client or anything in the room, and be sure to scrub carefully.
• If you are giving an injection, wear gloves (per Standard Precautions). Wear a gown and mask as the client’s condition indicates. Place needles and syringes into the sharps disposal container in the client’s room. To avoid an accidental needlestick, do not break or recap needles, or detach them from syringes. Most facilities use some type of “safety syringes” (see Figs. 64-3 and 64-4A) or have safety caps available (see Fig. 64-4B).
• Use disposable medication cups.
• Use and discard intravenous (IV) solution bags in the client’s room.
• Generally, glass items are not used in isolation. If they must be used, dispose of them in a separate bag, clearly marked “glass.” This must be double-bagged out of the room (see discussion later in this topic). Rationale: These measures will protect housekeeping staff from injury and will ensure safe disposal of biohazardous materials.
• Dispose of all materials in the client’s room. The trash will be double-bagged out of the room and properly handled by the facility’s housekeeping department.
Sending a Specimen to the Laboratory
Before collecting a specimen, label the container. After collection, place the container on a clean paper towel in the anteroom and carefully scrub the container outside the room, after removing your gloves and doing a thorough handwashing. Then, place the specimen into a sealable plastic bag identified with the standard “biohazard” label. It may also be necessary to inform laboratory personnel of specific suspected microorganisms, such as MRSA or VRE (see Fig. 41-2). Wash your hands again. In some cases, the specimen must be doublebagged. Take or send the specimen to the laboratory as soon as possible. Remember to touch the request cards or sheets and the outside of the bag only with your clean hands.
Taking Vital Signs
Usually, necessary equipment to take vital signs is kept in the client’s room and is disinfected when the client no longer is infectious or is discharged. Follow these guidelines when taking vital signs of a client in an isolation room:
• Use the equipment in the room. Do not bring items in with you.
• Wear gloves and whatever other PPE is indicated.
• Remember that there is usually a clock on the wall, so you will not need to use your watch. If you do need to use a watch, however, place it on a paper towel and touch only the bottom of the towel with your contaminated hands, or seal the watch in a plastic bag. Pick up the watch after you have scrubbed outside the room.
• Use disposable thermometers, cuffs, and stethoscopes if available. Many facilities use temperature indicator dots or other disposable systems for measuring the client’s temperature. A blood pressure apparatus is usually on the wall. The cuff and stethoscope are disinfected or discarded when the client is discharged.
Nursing Alert If a drug-resistant organism such as vancomycin-resistant enterococcus (VRE) or methicillin-resistant Staphylococcus aureus (MRSA) is present, all equipment remains in the isolated client’s room.
• If checking the client’s blood sugar, use the client’s own machine or obtain a separate machine to be used while that client is in isolation. When the client comes out of isolation, the machine must be thoroughly disinfected.
Using Double-Bagging
Although refuse and linen from all clients are considered contaminated, in some types of isolation these items are “double-bagged” out of the room. Two nurses must carry out the double-bagging procedure. The nurse inside the room is considered “contaminated” and the nurse outside is considered “clean.” Both nurses wear gloves and, if specified, gowns and/or masks. The contaminated nurse places dirty items into a bag and closes the top. This entire bag, inside and out, is considered “contaminated.” The clean nurse, outside the room, has a second bag that is considered “clean.” He or she folds the top of the clean bag down on the outside to make a collar or cuff. The clean nurse keeps his or her hands protected by this cuff. The contaminated nurse then places the contaminated bag inside the clean bag, while the clean nurse holds the clean bag (Fig. 42-4).
The contaminated nurse touches only the inside of the clean bag; the clean nurse touches only the outside of the clean bag and does not touch the contaminated bag. The clean nurse folds over the top of the clean bag, seals it carefully, and labels it, touching only the outside of the bag. After this is completed, both nurses wash their hands thoroughly.
FIGURE 42-4 • Double-bagging laundry out of an isolation room. The nurse in blue is considered to be the "clean” nurse. The "contaminated” nurse in the room wears gown, gloves, and a mask.
Transporting the Client to Other Departments
In rare cases, transporting the client to another part of the healthcare facility for a special procedure or x-ray is necessary. Take the following special precautions when transporting a client in isolation to another area:
• Wear PPE as needed.
• Make sure the client wears appropriate PPE, as indicated by his or her condition.
• Control and contain any of the client’s drainage.
• Drape the wheelchair or stretcher with a clean sheet or bath blanket. Wrap the client with the clean material.
• Make sure to escort the ambulatory client to any examinations.
• Notify the other department that the client requires special precautions so personnel can prepare and perform accordingly.
• Carefully disinfect the wheelchair or stretcher after use.
Caring for the Client’s Body After Death
If a client who is in isolation dies, you must take special precautions to prevent the spread of infection. Follow any particular protocols of your facility. Note that many healthcare facilities follow these precautions for all clients who die. In Practice: Nursing Care Guidelines 42-1 describes care of the body of the person who was in isolation.
Protective (Reverse or Neutropenic) Isolation
Sometimes, the client must be protected from the outside environment. In such a case, isolation procedures are reversed: other people’s microorganisms are kept away from the client. This type of isolation is known as protective isolation (also called reverse or neutropenic isolation). Protective isolation attempts to prevent harmful microorganisms from coming into contact with the client. Box 42-1 lists general procedures for protective isolation.
IN PRACTICE: NURSING CARE GUIDELINES 42-1
CARING FOR THE BODY OF A DEAD PERSON WHO WAS IN ISOLATION
• Follow the measures for caring for the dead person’s body that are listed.
• Wear a gown and gloves. A mask may be required in some cases.
• Wrap the body while you are in the room. Usually you will place it in a plastic zippered bag.
• Transfer the body to a cart that has been draped with a clean bath blanket or sheet. A clean person outside the room will wrap the clean blanket around the body
• Environmental services (housekeeping) personnel will decontaminate the room according to the facility’s procedures.
• If you are the person caring for the body inside the room, remember that you are considered contaminated. You must wash your hands thoroughly and properly dispose of gloves and gown (and mask) when leaving the room. Afterward, you may touch only the outside of the wrapping or shroud.
• Label the body stating the type of isolation or causative disease. The pathologist treats all bodies as if they have an infectious disease, but must know if a specific infection is present.
• Check your healthcare facility for special procedures.
Clients who need protective isolation have a weakened immune response. They may become infected; however, they may not show classic signs and symptoms of infection because they lack the white blood cells necessary to create the normal inflammatory response. Individuals who may require placement in protective isolation include those who have experienced burns or bone marrow transplants. Clients with acquired immunodeficiency syndrome (AIDS), who are undergoing chemotherapy for cancer, who have received large doses of corticosteroids, or who are experiencing low resistance from another cause (e.g., agammaglobulinemia) may also require protective isolation.
BOX 42-1. General Procedures in Protective/Neutropenic Isolation
• The client requires a private room or total neutropenic unit, such as a Burn Unit.
• Healthcare workers and visitors may not enter if they have a cold, influenza, or other communicable disease.
• Anyone entering the room must wear a mask and practice strict handwashing before coming into contact with the client. In some cases, such as in a Burn Unit, all staff and visitors may be required to wear gowns and gloves.
• The client cannot receive fresh fruit, fresh vegetables, or flowers.
• Rectal temperatures, enemas, suppositories, intravenous and intramuscular injections, and other invasive procedures are to be avoided, if possible.
• The tympanic/ear probe or forehead sensor for monitoring the client’s temperature is recommended. Measure the client’s temperature at least every 4 hours.
• A blood culture may be necessary if any reason exists to suspect infection.
• In some cases, special linens and specially laundered scrub suits and shoe covers are used. Some facilities require special hair covering. Staff working in these units often wear lab coats when leaving the units.
• Special air purification measures are used.
ANTIBIOTIC-RESISTANT ORGANISMS
The two most common antibiotic-resistant organisms are MRSA (methicillin-resistant staphylococcus aureus) and VRE (vancomycin-resistant enterococcus). Other multidrug resistant organisms (MDRO) also exist and are becoming more common.Because these organisms are not easily treated by antibiotics, they are becoming more and more dangerous to healthcare clients.
MRSA. Clients with MRSA are placed on contact precautions and must have a private room. Newborns of mothers with MRSA are usually roomed-in with the mother. All people, including visitors, must wash hands; gloves and a gown must be worn if there will be any contact with the client. Following is a common routine for MRSA isolation:
Surveillance cultures are done at least 7 days apart and at least 7 days after completion of clinical treatment. Cultures are taken in nares (nostril) and/or specific wound or drainage sites. In most facilities, these cultures must be negative three times in order to discontinue the isolation. Certain clients are not eligible to come out of isolation during their hospital stay. These clients include residents of long-term care facilities, and those with chronic skin breakdown (e.g., decubitus ulcers) or open wounds, wound drainage, and clients with long-term invasive devices, such as percutaneous endoscopic gastrostomy (PEG) tubes.
VRE. Most of the procedures for clients with VRE are similar to those for MRSA. These cultures are obtained from the perirectal (around the rectum) area and/or an open wound or drainage site.
Nursing Alert If there is an outbreak of MRSA or VRE within a facility, special measures are followed. These are prescribed by the facility under the guidance of the state or province’s Board of Health. In some cases, healthcare workers must be screened, as well as clients.
KEY POINTS
• Infection is best controlled by prevention—breaking the links in the chain of infection.
• The Joint Commission requires every healthcare facility it accredits to have an infection control plan.
• One duty of an infection control committee is to monitor and evaluate infections in clients or in staff who are exposed.
• Transmission-Based Precautions are designed to prevent the spread of specific infections. They include airborne, droplet, and contact precautions. The specific type of Transmission-Based Precautions for a particular client is used in conjunction with Standard Precautions.
• Barrier techniques are designed to prevent microorganisms from leaving a client’s room.
• Before entering a client’s room, determine the necessity of using PPE and other equipment.
• Special filtered respirator masks are often required when caring for a client with known or suspected TB.
• Isolation procedures vary among healthcare facilities. Know your facility’s specific procedures.
• Protective isolation helps prevent organisms from coming into contact with clients.
• Isolation is often frightening and misunderstood by clients and families.