COLD
Cold causes vasoconstriction (shrinkage of blood vessels), decreasing blood flow to an area, and slowing the body’s metabolism and its demand for oxygen. The therapeutic goals of cold applications include controlling hemorrhage, reducing edema, easing inflammation, and blocking pain receptors.
Rationale for Cold Application
Cold application prevents escape of heat from the body by slowing circulation, which also relieves congestion and often relieves muscle pain. A cold application:
• Slows or stops bleeding
• Slows bacterial activity in clients with an infection
• Relieves pain following some types of surgery, tooth extraction, headache, or muscle or joint injury
• Reduces swelling in injured tissues, including sprains and fractures
• Prevents peristalsis in clients with abdominal inflammation
• Relieves pain in engorged breasts
• Controls pain and fluid loss in the initial treatment of burns
• Diminishes muscle contraction and muscle spasms
• Slows the basal metabolism for certain types of surgery.
Cold application is more effective than heat for sprains or other soft tissue injuries and is the preferred treatment within the first 48 hours after injury. Cold is applied to prevent swelling (edema); however, cold application usually will not reduce edema that is already present. Methods of cold application include the use of a compress, icecap, ice collar, ice pack, sponge bath, and hypothermia (cooling) blanket. In Practice: Nursing Care Guidelines 54-2 lists important considerations when applying cold therapy.
IN PRACTICE: NURSING CARE GUIDELINES 54-2
APPLYING COLD THERAPY
• Stop the cold application immediately if the client complains of numbness or the skin appears white or spotty. Rationale: Cold numbs nerve endings.
• As cold decreases the flow of blood in one area of the body, flow increases to other areas. Rationale: This explains why cold or chilling drafts striking the body often cause congestion in the nasal passages.
• Continued application of cold affects deeper tissues. It is important to monitor the client closely. Rationale: Prolonged exposure to extreme cold may cause serious injury.
• Cold often is applied to a sprain, strain, fracture, or burn. Rationale: This helps remove blood and lymph congestion in the area and reduces pain.
Nursing Alert The application of cold can cause frostbite, which can be very serious. Frostbite may require extensive debridement, surgery (including amputation), and/or infections (including gas gangrene).
NCLEX Alert Cold therapies are often integrated into NCLEX situations and options. It is critical that you know when and why cold applications are more beneficial than heat therapies such as in the first hours after a bone fracture or muscle injury. It can be hazardous to apply heat when cold therapy is needed. It is very important that you understand why a particular cold therapy is chosen (i.e. the rational for use), what are the expectations of cold therapy (e.g. vasoconstriction, decrease swelling, slow bleeding, et al), and how to prevent complications for the chosen version of therapy Safety and client teaching issues regarding application of equipment and monitoring for complications are also common NCLEX concerns.
Specific Cold Therapies
Cold, Moist Compresses
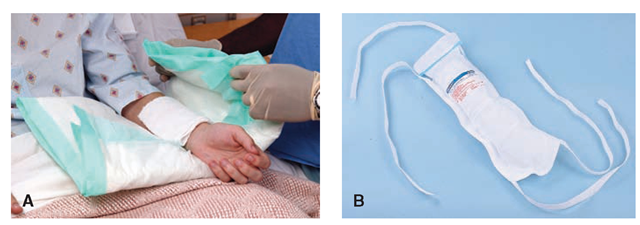
Cold, moist compresses are used to reduce swelling and inflammation in soft tissue injuries or after tooth extraction. The size of the compress depends on the area to be treated. Gauze 4- X 4-inch pads are frequently used for tooth pain. They are applied externally and are changed frequently because they warm rapidly, thereby losing their effectiveness. In Practice: Nursing Care Guidelines 54-3 provides information about applying cold compresses. Figure 54-3 illustrates both moist and dry cold applications.
Icecap or Ice Collar
The icecap, ice collar, or ice bag is a dry cold application. The icecap, used for the head, has a wide opening that allows it to be filled easily with ice chips, as does the ice collar, a narrow bag curved to fit the neck. Single-use ice bags are frequently used. The primary provider may prescribe dry cold to treat a specific area of the body. However, an ice bag is often used for a headache or in an emergency, such as a sprain or nosebleed, without an order (see In Practice: Nursing Procedure 54-5).
IN PRACTICE :NURSING CARE GUIDELINES 54-3
APPLYING COLD MOIST COMPRESSES
• Wear gloves if the client has an open wound or has had surgery. Rationale: This helps prevent infection transmission.
• Put the compresses in a basin containing pieces of ice and a small amount of water Rationale: Ice water soaks and cools the compresses faster than plain ice does.
• Explain to the client that the treatment will relieve discomfort. Rationale: A relaxed client will feel relief sooner than a tense client.
• Wring the compresses thoroughly and apply. Rationale: If ice water drips, it may startle the client.
• Change compresses frequently. Rationale: Compresses warm rapidly as they absorb body heat.
• Continue the treatment as ordered, usually for 15 to 20 minutes. Repeat every 2 to 4 hours as ordered. Clients who are able can apply the compresses themselves. Rationale: Applying the cold application for the specified time promotes treatment effectiveness and helps prevent injury.
• Properly dispose of gloves, if used, and wash the hands. Document the treatment, noting duration and the client’s reaction. Rationale: Proper glove disposal and handwashing help prevent infection transmission. Documentation promotes communication and continuity of care.
Nursing Alert If the skin becomes mottled or numb, remove the ice pack immediately Rationale: This indicates that the pack was too cold.
Single-Use and Refreezable Ice Packs
Healthcare agencies and emergency services often provide ready-for-use ice packs. These ice packs also are used by sports teams, hikers, and camping organizations. Sometimes, these can be refrozen, but only for one client. Rationale: Using the pack for multiple clients could promote the spread of pathogens.
Most emergency ice packs release a chemical that causes the bag to become cold when a capsule is broken or crystals are activated when the bag is shaken. They can be used only once.
Key Concept Some gel-filled packs also are available.These packs can be frozen or heated and used as either a cold or hot pack. These packs are reusable for only one client. Be aware that some of these bags may be frozen or heated in the microwave. Read the manufacturer’s instructions carefully. Be aware that the bag can explode in the microwave!
Tepid Sponge Bath
A tepid sponge bath is a bath with water below body temperature, between 80°F and 95°F (26.6°C to 35°C). This type of bath may be ordered to reduce a client’s elevated temperature. The first effect of this water on the skin is blood vessel constriction.
FIGURE 54-3 · Cold applications are often used to reduce pain and swelling or to arrest bleeding. (A) The cold compress is a moist cold application (Timby, 2005). (B) An ice pack or ice bag filled with crushed ice is a dry cold application.
Nursing Alert Many ice bags, particularly those with the capsule or crystals, become very cold. They can cause frostbite fairly quickly Therefore, use extreme caution when applying these. If the client’s skin becomes blanched or red, discontinue treatment immediately and check for further instructions.
In the event of client complaints of burning pain, treatment should be stopped immediately and the provider notified. Rationale: Burning pain indicates tissue ischemia (lack of blood supply) and may lead to tissue necrosis (tissue death). Untreated, this can lead to gangrene and necessitate amputation.
Nursing Alert Do not use alcohol. Rationale:
Alcohol cools too much because it evaporates very quickly.
A tepid sponge bath may be temporarily soothing, but may not produce a marked temperature drop unless used for an extended time, about 30 minutes. Tepid sponge baths are inadvisable for people with inelastic arteries (hardening of the arteries—arteriosclerosis), clients with arthritis or lowered resistance to disease (as a result of immunosuppression), and very young children. Rationale: The water has the initial effect of depressing body systems. See In Practice: Nursing Care Guidelines 54-4.
Nursing Alert Constantly assess the client’s core body temperature with an electronic thermometer during the sponge bath. If the client begins to shiver or if the core temperature falls to within I.50F of normal (approximately 38.7°C. or I00°F.), discontinue the treatment and report the findings to a supervisor.
If hyperthermia (elevated temperature) becomes life threatening, other treatments are usually used to lower temperature more quickly and permanently. In these situations, an ice mattress or hypothermia blanket may be used.
Hypothermia Blanket
A hypothermia blanket (cooling blanket) is a mattress pad through which very cold water flows continuously. Hypothermia blankets may be used in surgery to slow body processes or elsewhere in the facility to lower dangerously high body temperatures. (NOTE: Today, it is more common to warm clients during surgery, to help prevent hypothermia and infections.) Hypothermia blankets are equipped with electrical control units that can be set to a desired temperature. It is important to follow the agency’s protocol and the primary provider’s orders. Check frequently to make sure that the client’s core temperature does not fall too low.
The client’s core body temperature is checked constantly when using the hypothermia blanket, as it is when performing the tepid sponge bath.
Cold Humidity
Cold humidity is commonly ordered for clients with breathing disorders. In most facilities, air conditioning and heating systems provide a constant level of humidity. But if the humidity level is not high enough, an auxiliary humidifier may be placed in the room. Some clients need constant cold humidity in higher concentrations. A child may be placed in a croupette or a humidity (mist) tent. Oxygen administered to all clients must be humidified to prevent drying of the mucous membranes of the nose and throat. If the client has a tracheostomy, a “trach mask” may be placed over the opening to provide humidity, either with or without auxiliary oxygen. A face tent, which may be used to provide a high concentration of moisture in the inhaled air, is also available.
Key Concept The hypothermia blanket is used cautiously to treat uncontrollable hyperthermia. Risk occurs because the cold interferes with the normal febrile (fever) response. Fever-producing pathogens cause the body’s temperature regulatory center (the hypothalamus) to produce a new body temperature set point in the body’s effort to fight off the pathogen’s negative effects. (Normally the set point of body temperature is 370C or 98.60R) When the hypothalamus raises this set point to a higher temperature, the body attempts to reach this new set point with mechanisms that begin the febrile response— shivering and peripheral vasoconstriction. Using a hypothermia blanket during this response decreases the actual body temperature, moving it further away from the set point. This may cause an even more severe febrile reaction. In addition, fever sometimes is helpful, because it has the effect of destroying pathogens.
Nursing Alert When using any method for cooling the client’s body have bath blankets readily available for use in case of chilling. Be aware that body temperature can continue to fall after the treatment is discontinued. Stop the treatment and check with the provider when the client’s temperature approaches the preprescribed level (approximately 38.70C [I000F]).
IN PRACTICE :NURSING CARE GUIDELINES 54-4
GIVING A TEPID SPONGE BATH TO REDUCE BODY TEMPERATURE
• Explain the procedure to the client. Rationale: The bath is less likely to be effective if a client is nervous or fearful.
• Give the client an opportunity to void or defecate before the bath. Rationale:The client will be more comfortable. It is important to avoid having to stop and restart the bath.
• Take the client’s temperature and record it. Rationale: The baseline temperature is important.
• Continued monitoring of the client’s temperature during the procedure is required. Rationale: Temperature monitoring provides objective data about the effectiveness of the bath, thus helping to prevent reducing the client’s core temperature too much. Remember, temperature will continue to drop after the bath. A continuous electronic thermometer is usually used.
• Note whether the client has had an antipyretic (e.g., aspirin or ibuprofen) to reduce fever Rationale: Such medications may influence the sponge bath’s effectiveness.
• Add tepid water to the bath basin, 26.6°C to 35°C (80°C to 95°F). Use a bath thermometer Rationale: These temperatures are below normal body temperature, so they will be effective in lowering the client’s fever. However, they are not so cold as to be dangerous.
• Place moist, cool cloths—wrung out just enough to prevent dripping—in the client’s axillae and the groin. Rationale: The blood vessels in these areas lie close to the skin. Water evaporation will be rapid there.
• Be aware that the client’s first reaction to a tepid sponge bath is a sensation of chilliness, which disappears as the body adjusts. Therefore, continue the bath long enough to allow for this adjustment (at least 25 to 30 minutes).
• Sponge each limb for at least 5 minutes and the back and buttocks for at least 10 to 15 minutes. Rationale: Sponging for this length of time is necessary for fever reduction.
• Stop the procedure if the client becomes very chilled or begins to shiver. Rationale: People respond to treatments differently. Stopping the procedure, due to complaints of chilling or evidence of shivering, prevents possible hypothermia.
• Stop sponging as soon as the client’s temperature approaches the normal range (about 38.7°C or I00°F, orally). Give the client a bath blanket. Rationale: The client’s temperature will continue to drop after the bath is completed. Stopping the bath when the client’s temperature is still above normal body temperature prevents it from dropping too low.
• Wash the hands. Document the treatment, noting the client’s reactions. Be sure to record the temperatures before, during, and after the procedure. Rationale: Handwashing helps prevent infection transmission. Recording the client’s responses to treatment is vital, especially if the procedure needs to be repeated.
• Take the client’s temperature 30 minutes after you complete the bath. Report the temperature immediately if it has fallen too low (below about 37.5°C or 99.5°F). Rationale: The body takes about 25 to 30 minutes to fully respond to cold applications.
KEY POINTS
• A major goal in healthcare is the maintenance of normoth-ermia.
• Heat dilates surface blood vessels.
• Whenever heat is applied, take measures to prevent burns.
• Warm, moist applications heat the skin more quickly than dry heat applications.
• Water temperature for a soak should be no higher than 105°F (41 °C).
• A sitz bath applies heat and water to the pelvic, perineal, and perianal area.
• Cold constricts surface blood vessels.
• Cold, moist compresses are applied to small body parts.
• A tepid sponge bath may be used to reduce body temperature temporarily.
• When cold is applied, it is important to prevent undue chilling and/or frostbite.
• Several methods may be used to administer heat or cold treatments.