Learning Objectives
1. Define homeostasis in relationship to fluid and electrolyte balance. Describe negative and positive feedback.
2. Describe the intracellular and extracellular fluid compartments, including components of each and the respective portion of total body weight that each represents. Name the most important cation and anion in each.
3. Describe how the thirst center, atrial natriuretic peptide, and the RAA system help regulate fluid balance.
4. Explain “third-spacing” and describe four ways edema can occur. State three procedures to teach a client who needs to decrease/prevent edema.
5. Identify four functions of water.
6. Name three major electrolytes necessary for neuronal and muscular function. Describe two nursing actions to help maintain their balance.
7. Differentiate between freely permeable and selectively permeable membranes. Discuss factors affecting permeability.
8. Contrast the transportation of fluids and other molecules by way of diffusion, osmosis, filtration, and active transport.
9. List normal sources of water gain and the mechanism of water loss in the body. Identify normal daily intake and output for an average adult.
10. Describe major components and actions involved in maintaining acid-base balance, including the significance of arterial blood gas values as an indicator of imbalance.
11. Explain why infants, young children, and the elderly are at risk for fluid and electrolyte imbalances. Describe two nursing implications to assist seniors to maintain fluid and electrolyte balance.
|
IMPORTANT TERMINOLOGY |
||
|
acid |
edema |
ion |
|
anasarca |
electrolyte |
isotonic |
|
anion |
feedback |
osmosis |
|
ascites |
filtration |
permeability |
|
base |
hypertonic |
salt |
|
buffer |
hypotonic |
solute |
|
cation |
insensible |
solvent |
|
dehydration |
interstitial |
third-space (fluid) |
|
diffusion |
intravascular |
|
|
Acronyms |
|
|
|
ABGs |
H + |
Na+ |
|
ADH |
HCl |
NaCl |
|
ANP |
HCO3- |
NaOH |
|
Ca+ + |
H2O, HOH |
Na2SO4 |
|
Ca3[PO4]2 |
HPO4", |
NS |
|
CaCl2 |
h2po4~ |
O , O2 |
|
CaCO3 |
ICF |
OH1 |
|
Cl1 |
K+ |
PaCO2 |
|
CSF |
KCl |
PaO2 |
|
ECF |
mEq |
pH |
|
Fe+ + |
Mg+ + |
RAA |
|
GI |
mL |
I 4 04 5 |
Virtually every tissue and organ in the body has an active role in maintaining homeostasis (balance or stability). Body fluids, composed of water and substances dissolved and suspended in it, form the environment of each body cell. Fluids move into and out of cells, bringing with them enzymes, hormones, and nutrients, as well as removing waste products (end products of metabolism). This continual movement of fluids is necessary to maintain homeostasis. This topic reviews the importance of water and selected electrolytes and major systems of fluid transport within the body.
HOMEOSTASIS
Homeostasis is the dynamic process through which the body maintains balance by constantly adjusting to internal and external stimuli. (Home/o means constant or sameness and the suffix, -stasis, means controlling; therefore, homeostasis means “controlling sameness.”) This provides temperature regulation and stability, regulation of body glucose (sugars), timing of sleep cycles, and other life-sustaining processes. The concept of homeostasis is the basis for understanding most physiologic processes. For the body to maintain homeostasis, it must be able to sense minute (tiny) changes and react appropriately. To do so, the body has sensors and integrating centers that involve all body cells and systems.
Negative and Positive Feedback
All components of the body constantly send tiny signals that cause responses. Simply stated, feedback is the relaying of information about a given condition to the appropriate organ or system.
Key Concept Receptor (sensing component) —» control center (brain) —» appropriate response (effector—muscles, organs, hormones) S change (positive or negative feedback) = homeostasis.
Negative feedback occurs when the body reverses an original stimulus to regain physiologic balance (homeostasis). Body systems resist deviations, normally allowing for small variations only. Blood pressure control and maintenance of normal body temperature are examples of negative feedback systems. Illness interrupts negative feedback; healthcare measures attempt to restore and maintain homeostasis (equilibrium) as much as possible.
In positive feedback, the body enhances or intensifies an original stimulus. The body senses deviations, but positive feedback generally is not homeostatic. In fact, the body often responds by increasing the deviation. An example of helpful positive feedback is blood clotting following an injury. Another normal example is a woman in labor. When labor begins, impulses are sent to stimulate the release of the hormone oxytocin, which increases uterine contraction strength and frequency. An example of dangerous positive feedback is a very high fever, which can spin out of control. Therefore, in some situations, positive feedback systems can lead to greater instability or death.
Systems Involved in Feedback
The major systems involved in feedback are the nervous and endocrine systems.The nervous system regulates homeostasis by sensing system deviations and sending nerve impulses to appropriate organs; the endocrine system uses the release and action of hormones to maintain homeostasis.
Key Concept An individual must maintain internal homeostasis to maintain health.
BODY FLUIDS
Fluids make up a large portion of the body (approximately 50%-60% of total body weight). Body fluids are composed of water and electrolytes (substances that dissolve in water).
Location of Fluids
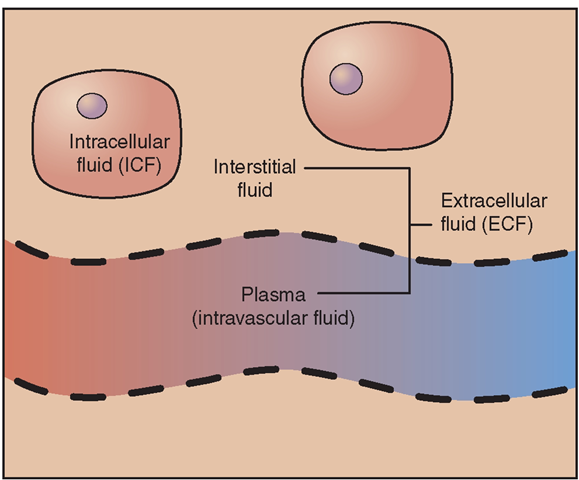
Body fluids are divided between two main compartments: the intracellular fluid (ICF) and the extracellular fluid (ECF). ICF, which is the fluid inside the cells, constitutes about one half to two thirds of the total body fluid in an adult. ECF, which is the fluid outside the cells, constitutes about one third of the total body fluid in an adult. Fluids continuously move between compartments (Fig. 17-1). The compartments contain slightly different components, and several homeostatic mechanisms work to maintain the correct balance of fluid to solid substances within each compartment.
Intracellular Fluid
Intracellular fluid functions as a stabilizing agent for the parts of the cell and helps to maintain cell shape. ICF also assists with transport of nutrients across the cell membrane, in and out of the cell. The liquid portion of cytoplasm is called cytosol. Cells vary in water content. Skeletal muscle contains about 75% water; fatty tissue contains about 10% water (with the remainder being lipids [fats]). If a person’s body is 60% water, the ICF is 40% of total body weight. The major ions in ICF are potassium, magnesium, and phosphate (and proteins).
Extracellular Fluid
Extracellular fluid appears mostly as interstitial (tissue) fluid (IF) and intravascular (IV—within blood vessels) fluid.
FIGURE 17-1 · Major fluid compartments. Intracellular fluid (ICF) is fluid within cells. Extracellular fluid (ECF) is fluid outside of cells. The ECF includes interstitial fluid surrounding the cells, and plasma, the fluid component of blood. (In addition, specialized ECF includes synovial fluid, CSF, aqueous fluid in the eye, and some specialized GI secretions.) Fluid continually moves between the major compartments.
Interstitial fluid is found between cells. Intravascular fluid is the watery fluid in blood known as plasma. Specialized ECFs, also called transcellular fluids, are usually within epithelial-lined spaces; these include synovial fluid in joint cavities, CSF (cerebral spinal fluid) in the brain and spinal cord, and aqueous (ocular) fluid in the eyes. Some additional ECFs are located in the gastrointestinal (GI) tract, liver, biliary tract, and lymphatic vessels. Bladder urine is also considered a transcellular fluid. Major ions in ECF are sodium, chlorine, and carbonate.
The volume of ECF is the most important regulated aspect of body fluid balance. Without adequate ECF, the body cannot maintain normal blood pressure. A significant loss of ECF volume can drop blood pressure to a life-threatening point where cells can no longer function, due to a lack of oxygen and nutrients. This results in a condition known as hypovolemic shock.Too much ECF can place a person in a fluid overload state, leading to high blood pressure and risk for conditions such as congestive heart failure.
Key Concept ECF is the fluid that is most important in fluid balance.
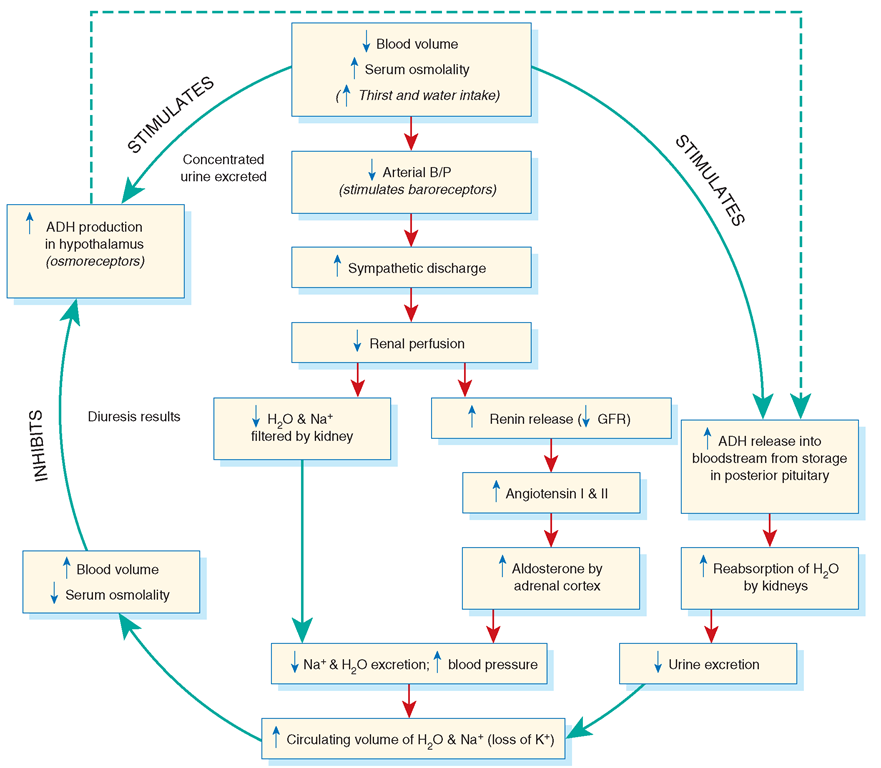
The body monitors ECF volumes closely and sends messages to the brain, kidneys, and pituitary gland to maintain control. Primary mechanisms involved in regulation include the actions of the thirst center in the hypothalamus; release of antidiuretic hormone (vasopressin—ADH) from the pituitary gland; effects of the renin-angiotensin-aldosterone (RAA) system; and release of the atrial natriuretic peptide (ANP) hormone by the heart (Fig. 17-2).
The Thirst Center. The thirst center in the hypothalamus stimulates or inhibits the desire for a person to drink. Excessive fluid intake (polydipsia), particularly of plain water, can cause severe electrolyte imbalance.
FIGURE 17-2 · Fluid regulation cycle, including antidiuretic hormone (ADH) and the renin-angiotensin-aldosterone (RAA) system.
Antidiuretic Hormone. ADH (vasopressin) is released from storage in the posterior pituitary gland as part of the negative feedback mechanism in response to conditions within the cardiovascular system. ADH regulates the amount of water the kidney tubules absorb (reabsorption) and is released in response to low blood volume (as seen in low blood pressure or hemorrhage) or in response to an increase in concentration of sodium and other solutes (increased plasma osmolarity) in the intravascular fluid (blood plasma). When ADH is released, urine production is decreased and water reabsorption is increased.
The RAA System. The RAA system controls fluid volume. When blood volume decreases, blood flow to the renal (kidneys’) juxtaglomerular apparatus is reduced, activating the RAA system. Renin is released by the kidneys, causing secretion of angiotensin I, which is converted to angiotensin II (by an enzyme) in the lungs. Angiotensin II causes both vasoconstriction (which increases blood pressure) and the secretion of aldosterone by the adrenal cortex. Aldosterone causes increased reabsorption of sodium and water by the kidneys in an attempt to increase blood volume. (Water “follows” sodium [salt], which is explained later in this topic). Excretion of potassium is also increased in an attempt to restore homeostasis (see Fig. 17-2).
Atrial Natriuretic Peptide. The heart also plays a role in correcting overload imbalances, by releasing ANP from the right atrium. ANP promotes renal diuresis (kidney excretion) of sodium and water.
Normal Intake and Output
An adult human at rest takes in approximately 2,500 mL of fluid daily. Approximate levels of intake include fluids 1,200 mL, foods 1,000 mL, and metabolic products 300 mL. Daily output should approximately equal intake. Normal output occurs as urine, breathing, perspiration, feces, and in minute amounts of vaginal secretions.
Key Concept Amount of fluid taken in must approximately equal the amount lost to maintain homeostasis. The term euvolemic refers to normal body fluid volume.
Special Considerations: LIFESPAN
Risk for Fluid Volume Deficit
Infants have considerably more body fluid by percentage than adults do, most of which is extracellular fluid (ECF). They are at an increased risk for fluid volume deficit because ECF is lost more easily than intracellular fluid (ICF). Also, immature kidney function places infants and young children at risk for alterations in fluid and electrolyte levels.
Overhydration and Edema
Overhydration is an excess of water in the body. Edema is the excess accumulation of fluid in interstitial (tissue) spaces, also called third-space fluid. Edema is caused by a disruption of the filtration and osmotic forces of the body’s circulating fluids. Some causes of edema include obstruction of venous blood or lymphatic return, increased capillary permeability or increased capillary pressure, external pressure (e.g., tight binders or casts), and inflammatory reactions. Increased sodium intake, urine retention, and endocrine disorders can also cause edema. A loss of plasma proteins also leads to edema. Box 17-1 discusses some causes of edema.
BOX 17-1.
Sample Causes of Edema
Increased Capillary Pressure
Arteriolar dilatation
Allergic responses (e.g., hives, angioneurotic edema) Inflammation Venous obstruction Hepatic obstruction Heart failure Thrombophlebitis External pressure Tight clothing or casts Increased vascular volume Heart failure
Increased levels of adrenocortical hormones Premenstrual sodium retention Pregnancy
Environmental heat stress Effects of gravity
Prolonged standing or sitting
Sitting with legs crossed or pressure behind the knees
Decreased Colloidal Osmotic Pressure
Decreased production of plasma proteins Liver disease
Starvation or severe protein deficiency Increased loss of plasma proteins Protein-losing kidney diseases Extensive burns
Increased Capillary Permeability
Inflammation Immune responses Neoplastic disease (cancers)
Tissue injury and burns
Obstruction of Lymphatic Flow
Infection or disease of the lymphatic structures Surgical removal of lymph nodes
Some edema is localized, such as that caused by inflammation in an injured ankle. Edema can also be systemic (throughout the body), symptomatic of serious medical problems. Many conditions, such as kidney disease, congestive heart failure, or malignancies (cancer), can result in systemic edema. Treatment of edema is directed at treating the underlying cause. Diuretics, medications that stimulate urination, are commonly given for systemic edema. (This causes an increase in loss of body fluids and salts via the kidneys.)
Some body fluids are not available for functional use. These are extracellular fluids that occur within interstitial spaces in various parts of the body. Excess fluid accumulations in interstitial spaces are often caused by inflammatory conditions. Examples include pleural effusion (accumulation of fluid between the pleura of the lungs) or pericardial effusion (accumulation of fluid within the pericardial sac around the heart). Disease processes, such as ascites (an excess amount of peritoneal fluid) and anasarca (severe generalized edema), also result from abnormal fluid shifts. Fluid volume excess is the descriptive term in the nursing care plan referring to excess intravascular and/or interstitial fluid.
Key Concept In edema, the body attempts to restore homeostasis by increased secretion of natriuretic ("salt-losing”) peptides, decreased ADH, increased urine output, and reduced thirst.
Dehydration (Impaired Fluid Homeostasis)
Many disorders result in a deficiency of body water or excessive loss of water (dehydration). In dehydration, water output is greater than intake. Dehydration can be associated with sodium loss or disturbance of another electrolyte, such as potassium. External causes of dehydration include prolonged sun exposure and excessive exercise, as well as diarrhea, vomiting, and burns. In some cases, inappropriate use of diuretics, malnutrition, excessive fasting, anorexia, or bulimia causes dehydration. Decreased fluid intake, fever, gastrointestinal suction, certain medications, and hemorrhage may also contribute to dehydration, as well as stimulant or alcohol abuse. Certain disorders, such as electrolyte dysfunction and Addison’s disease, can also be causes. Diabetes (both mellitus and insipidus) and related factors, such as hyperglycemia and glycosuria, may also cause a fluid deficiency.
Early in dehydration, the person feels thirsty and drinks more fluid. If fluid intake cannot keep up with fluid loss, dehydration increases in severity. The body compensates by reducing urine output and sweating. Water moves from the ICF compartments into intravascular fluids. If dehydration is not corrected, body tissues begin to dry out and malfunction. Brain cells are particularly susceptible to dehydration; one early sign of severe dehydration is mental confusion. Untreated, this can progress to coma. Dehydration can also cause severe damage to organs such as the kidneys and liver, owing to low blood pressure caused by reduced circulating blood volume. As in edema, treatment of dehydration is first directed at the underlying cause. Supplemental fluids and electrolytes are often administered. Fluid volume deficit is the descriptive term for dehydration.
Nursing Alert Thirst is a primary indicator of hydration status. Therefore, assess your clients for thirst as an early symptom of dehydration.