Hypothermia
Hypothermia occurs when the body loses heat faster than it can burn food (fuel) to replace it. It is caused when a person is exposed to extreme or fairly extreme cold or is chilled sufficiently long to lower his or her core (internal) body temperature to a dangerous level. A critical level of hypothermia can lower the core temperature to as low as 94°F (35°C) or lower. Profuse sweating over time can also cause hypothermia. Windy or wet conditions greatly accelerate the onset of hypothermia. Hypothermia caused by such external forces is known as accidental hypothermia. Hypothermia also occurs when the body’s temperature regulation malfunctions. In addition, temperature is sometimes intentionally lowered to make surgery safer. This procedure is called induced or surgical hypothermia. Induced hypothermia confined to one body part is called local hypothermia.
Accidentally lowering the body’s core temperature even a few degrees can result in serious symptoms and even death. Symptoms of hypothermia include sleepiness, slow and clumsy movements, shaking, cardiac dysrhythmia, loss of reflexes and slowed reaction times, impaired judgment, confusion, and respiratory failure. Hallucinations may occur. If the person is in water, drowning is very possible as a result of weakness and confusion. In a first-aid situation, the initial warning signs are confusion, disorientation, slurred speech, obvious shivering, and lethargy. Check also to see if the person complains of blurred vision, dizziness, tiredness, or feeling very cold.
Key Concept Preventing hypothermia is important, especially for individuals, such as campers and hikers, engaged in outdoor activities. Because major heat loss occurs via the uncovered head (which acts like a chimney), wearing a hat is very important. Wool clothing helps because it is warm even when wet. Wearing layered clothing also is beneficial because the air pockets between layers serve as insulation. Eating enough food and obtaining adequate fluids are also important. Warn campers and hikers to remain dry and to avoid sitting on wet surfaces, cold ground, rocks, or cold metal surfaces. Snow should not be eaten for fluid, but should be melted and warmed first.
Definitive diagnosis of hypothermia is based on an accurate measurement of core temperature. Special monitoring equipment is necessary because normal clinical thermometers often do not register low enough to measure core temperature accurately.
Treatment of Hypothermia
Gradual rewarming is necessary. Rationale: When the body is rewarmed too quickly, cold blood returns to the heart, causing severe dysrhythmia and sometimes cardiac arrest. The person’s cardiac status is continually monitored during rewarming.
On a first-aid basis, get the person into warm, dry clothing. Cover the person’s head, hands, and feet. A ground cover provides a barrier against moisture and insulates against cold materials under the person. Keep the person awake until medical assistance arrives. Remove wet clothing. Warmed beverages also help if the person is alert and can swallow.
If the client is unconscious, immediate transfer to a healthcare facility is vital. There, the body is warmed until the core temperature is approximately 94°F (35°C). Then the extremities are warmed. Warmed blankets and warming lights are used. Sometimes, the person is placed in warm water. In addition, warmed oxygen and warmed IV infusions may be given. Blood may be circulated through a pump oxygenator and warmed before returning it to the body’s core circulation. Warm fluids may be instilled into the gastrointestinal (GI) system. Treatment continues until the body’s core temperature is near normal (98.6°F; 37°C).
Nursing Considerations
The person with severe hypothermia must be moved very carefully to prevent cardiac dysrhythmia or arrest. During the rewarming process, nursing care includes careful monitoring of vital signs and IV infusion, close observation of skin condition, special mouth and eye care, and measurement of oral and IV intake and urine output. Monitor the body’s core temperature by using a special electronic thermometer. The person who has an IV infusion may suffer from complications including bleeding and gastric distention.
Nursing Alert Hypothermia that accompanies frostbite is a medical emergency Give immediate emergency care in any case of hypothermia. A person with severe hypothermia is not considered dead until he or she has been rewarmed and still shows no signs of life. Because of the increased risk for cardiac standstill (cardiac arrest), CPR is not usually recommended for this person until he or she is in the ED. Remember that the air temperature does not have to be extremely cold for hypothermia to occur
Heat-Related Injuries
Heat-related injuries are most likely to occur on days of high humidity, with temperatures from 95°F to 100°F (35°C to 37.8°C), and no breeze. Rationale: The body’s major defense against heat accumulation is sweating; evaporation of sweat helps cool the body. When humidity exceeds 75%, particularly when there is no breeze, evaporation decreases. The heat index is expressed in terms of “the temperature feels like,” a combination of heat and humidity. The higher the heat index, the more likely are heat-related injuries to occur. Heat injuries typically occur in early summer before people have acclimated themselves to high temperatures. Such injuries can also occur inside enclosed areas, when the outside temperature is low but other heat sources increase a person’s internal heat load. For example, on a bright day, a parked car can quickly become a fatal enclosed area for children and pets because of the radiant heat produced by the sun. Heat produced in some work areas also can cause illness. Any enclosed area where equipment and lighting produce a large amount of heat that accumulates has the potential to cause heat-related illness.
Although sensitivity to heat varies among individuals, certain groups are particularly susceptible. Studies have identified infants, older adults, the very obese, chronic abusers of drugs or alcohol, and persons with underlying illnesses as being at the highest risk for heat-related injuries. Military personnel and athletes are also vulnerable because of the tendency to over-exercise in the heat, sometimes in heavy clothing.
Heat Cramps
Heat cramps are severe muscle spasms that usually occur after hard exertion. They are frequently found in physically fit young people, who have been sweating profusely and drinking plain water. These cramps can occur in cool environments, as well as hot ones, and are usually located in the legs, arms, or abdomen. The person may show signs of heat exhaustion (see discussion below) in addition to heat cramps.
Heat cramps are relieved by drinking very dilute salt solutions. Give the person a mixture of up to % teaspoon of salt per quart of water or another balanced salt solution. Commercial products such as sports drinks (e.g., Gatorade) also contain extra sodium and other electrolytes. If symptoms continue longer than an hour, seek medical advice. Salt tablets are not recommended because they are gastric irritants. Moving the person to a cooler environment is helpful, but make sure the person’s head is uncovered, and keep him or her calm. Explain what is happening. Tell him or her to avoid exertion for the next 12 hours.
For the future, suggest that the person add some salt (but not too much) to food before exertion. The person should also drink adequate liquids (not just plain water) and stop exercising if he or she feels ill. Misting the skin with water also helps.
* Key Concept Persons in cooler climates,such as mountain climbers, may experience heat cramps because they are dressed too warmly causing excessive sweating. Massaging cramped muscles will not cure heat cramps and, in fact, may increase the pain.
Heat Exhaustion
Heat exhaustion often occurs in physically fit people who are exerting themselves in a hot environment over a length of time. Under such conditions, these people do not take in sufficient water and sodium to replace lost fluids and electrolytes, resulting in a serious blood flow disturbance similar to shock. Pure forms of heat exhaustion are rare. Heat exhaustion that occurs quickly is likely to be related to water depletion. Another type of heat exhaustion, called salt-depletion heat exhaustion, develops over time. True heat exhaustion is rarely life threatening.
As a person loses large amounts of water and salt through sweating, blood flow decreases, if water is not replaced. Decreased blood flow affects brain, heart, and lung functioning. When a person loses salt as well as water, heat cramps may occur, along with headache, dizziness, anxiety, nausea, and weakness. Other symptoms of heat exhaustion include excessive sweating, faintness, hypotension, loss of appetite, and unconsciousness (usually brief). Fainting or unconsciousness is most common when the person is standing because blood pools in the legs, interfering with blood flow to the brain. Skin is pale, cool, and usually sweaty; body temperature may be subnormal, and blood pressure is low. The person’s eyes are dilated, breathing is rapid and shallow, and pulse is slow and weak. The person may have difficulty walking.
Treatment for heat exhaustion includes cooling the person without chilling him or her. Move the person to a cool place and remove and loosen as much clothing as possible. Apply cold, wet compresses to the skin. Fanning is helpful. Have the person lie down with the head about 8 to 12 inches below the feet. Rationale: Doing so will help increase circulation to the brain. Water replacement and rest will usually relieve symptoms of heat exhaustion caused by water depletion. However, the salt-depleted person will usually need sips of a salt solution, given slowly over a period of time. With any doubts about the person’s condition, transport him or her to a healthcare facility immediately. Rationale: Telling the difference between heat exhaustion and heat stroke may be difficult. If blood pressure and pulse remain low for more than half an hour to 1 hour, suspect heat stroke.
Heat Stroke
Heat stroke is a potentially life-threatening condition. This condition often develops rapidly and requires immediate treatment. Classic heat stroke occurs when the body’s heatregulating mechanisms fail and core temperature soars. When a person’s core temperature reaches 105ºF to 110ºF, sweating stops, brain cells become damaged or destroyed, and death results. Classic heat stroke usually occurs during a summer heat wave with high temperatures and humidity. Classic heat stroke most often affects the poor, those living in poorly ventilated housing and without air conditioning, older individuals who do not take in enough water, and chronically ill persons, who often are taking medications that contribute to heat stress. However, the recent death of a professional football player points to the dangers of extreme heat and humidity for all people, regardless of age or physical conditioning.
Nursing Alert Certain illnesses, such as cystic fibrosis and scleroderma, restrict the client’s ability to sweat.
These individuals are more susceptible to heat stroke.
Exertional heat stroke develops from an increased internal heat load due to muscular exertion, along with high external temperature and humidity. It usually occurs rapidly (within a few hours) in young, healthy, athletic individuals, simply because their heat-regulating systems become overwhelmed. In about half the cases of exertional heat stroke, the person is sweating.
Persons with classic heat stroke usually are brought to the healthcare facility because of hypotension, fever, and coma. Persons with exertional heat stroke are usually brought in because of bizarre behavior or collapse. Both forms of heat stroke can be life threatening and require immediate medicalcare. Rationale: The longer a person goes without treatment, the greater the danger.
Persons suffering from either form of heat stroke share many of the symptoms of heat exhaustion. However, some distinct differences exist (Table 43-1). Persons suffering from heat stroke have hot skin, and usually a high body temperature—above 106ºF (41.1ºC). Persons suffering from heat exhaustion have cool skin and normal or even slightly below normal body temperature.
After activating the EMS, first-aid treatment for heat stroke includes rapidly cooling the person to at least a temperature of 101ºF. Place the person in a cool, shady place and remove his or her clothing. Wrap the person in cold, wet sheets or spray the body with a cold mist of water. Place ice packs on the person’s forehead, under the armpits, and at the neck and groin. If the person is conscious, give sips of cold liquids containing a dilute salt solution. Tell the person not to drink too quickly (to prevent nausea). Prevent shivering. Monitor the person’s airway, breathing, and circulation. If necessary, begin CPR. Watch for seizures. Immediately transport the person for emergency care.
Nursing Alert If the person suffering from any type of heat-related illness vomits, stop giving fluids. The person needs IV fluid replacement. This is usually the only time a person with heat exhaustion needs to be hospitalized. Any person with
heat stroke needs immediate medical attention.
|
ELEMENT |
HEAT EXHAUSTION |
HEAT STROKE |
|
Skin |
Cool |
Hot |
|
Sweat |
Person may or may not sweat. |
Classic heat stroke—person is usually dry Exertional heat stroke—person is usually sweating. |
|
Body temperature |
Normal or below normal |
High (often >106°F) |
|
Symptoms |
Headache, nausea, dizziness, weakness, faintness, pale skin, weak pulse, tachycardia, anorexia, hypotension, brief periods of unconsciousness, rapid breathing |
Classic heat stroke—hypotension, fever, coma Exertional heat stroke—confusion, bizarre behavior, collapse |
|
Treatment |
Cool the person without chilling; elevate his or her feet. Water depletion—give water Salt depletion—give salt solution. |
Cool person rapidly, monitor airway and circulation, observe seizure precautions. |
|
Medical attention |
Seek medical attention if in doubt. |
Seek medical attention immediately in all cases. |
Burns
Burns occur from many heat sources.
The most common emergency cases of burns are caused by thermal, electrical, chemical, and radiation sources. Flames, steam, hot liquids, and hot objects may cause thermal burns. Electrical power sources or lightning may cause electrical burns. Strong chemicals can cause severe chemical burns to the skin, respiratory system, or eyes. Radiation sources (e.g., power plants) may cause radiation burns; sunburns also fall in this category.
First Aid for Sunburn
Too much exposure to the ultraviolet rays of the sun or a sun lamp causes sunburn. Although a person of any skin tone can be sunburned, the effects on an individual vary with the person’s skin tone and previous levels of sun exposure. It is important to apply sun block before spending any length of time in the sun, particularly if the person is susceptible to sunburn. Excessive exposure to the sun is also known to cause certain types of skin cancer.
The person who is sunburned will have reddened skin and may have a fever. Blisters and peeling may develop later. First aid for sunburn involves neutralizing the burning effects. This can be done with vinegar, milk, or certain commercial preparations. The sooner these measures are applied, the less chance exists for long-term damage to occur. In cases of severe sunburn or if the person develops a fever, he or she should receive emergency medical care.
First Aid for Other Types of Burns
The seriousness of a burn is estimated by its depth, percentage of the body burned, location, age of the victim, and any underlying complications.The following are examples of special considerations:
• A burn that involves more than 10% of the body’s surface is extremely serious.
• Any second- or third-degree burn is serious.
• Burns to the hands, feet, mouth, throat, and perineum are serious.
• Full-thickness, circumferential burns to the limbs or chest are particularly dangerous because they can restrict circulation and breathing.
• Diabetic persons of any age have more difficulty recovering from burns because their bodies heal more slowly; they may also have underlying circulatory or other difficulties.
• Any underlying injury can affect a person’s recovery after a burn.
• A person with a compromised immune system is at a particularly high risk for infection following a burn.
In Practice: Nursing Care Guidelines 43-2 summarizes immediate first-aid measures for burns.
Associated problems often cause more harm than the burn itself. Be alert for inhalation injuries and breathing problems, as well as for broken bones or other injuries. Check for the signs of possible inhalation injury including:
IN PRACTICE :NURSING CARE GUIDELINES 43-2
PROVIDING EMERGENCY FIRST AID FOR BURNS
♦ Stop the burning process by removing the heat source. Make sure burning clothing is cooled. Do not remove burning fabric or other materials, unless they fall off. Rationale: Some synthetic materials continue to smolder or melt and must be neutralized; however, removing the clothing could tear the person’s skin and damage it further.
♦ Remove as much clothing in the burned area as is possible, if it is not stuck to the skin. Tight clothing can be especially dangerous later. Rationale: Often, swelling occurs. Tight clothing contributes to swelling by hampering circulation. Removal of clothing also helps to cool the person. (Make sure the person does not become chilled.)
♦ If rescuers arrive within a few minutes, flood the area with cool water Do not apply ice. Rationale: The goal is to cool the area to stop the burning and to reduce the incidence of scarring. Ice may further irritate the burned area by cooling it too quickly.
♦ Continue to flood the area with cool water Rationale: Cool water helps control pain; discontinuation may increase pain temporarily because of damaged nerve endings.
♦ Flood most chemical burns with a gentle, continuous flow of plain water until emergency help arrives. Rationale: Flooding with water will help stop the burning process and cool the area. It will also help dilute and wash away caustic chemicals.
♦ Always check a chemical container for directions on emergency treatment. Rationale: Some chemicals react adversely when in contact with water.
♦ Watch for shivering if you are using water to cool a burn covering more than 10% of the body Change to dry sterile dressings if shivering occurs. Rationale: Exposure to cold may cause hypothermia.
♦ Do not put anything other than water or a specifically prescribed substance on a burn. Rationale: Materials such as salves, ointments, or butter occlude the burn so it becomes difficult to examine. These substances promote infection and pain on removal.
♦ Remove the injured person’s jewelry. Put it in a safe place. Rationale: It can remain hot and continue the burning process. Swelling usually occurs later, making it impossible to remove rings or other jewelry; if left on, jewelry can cut off circulation.
♦ Monitor the person’s airway breathing, and circulation. Be prepared to initiate CPR. Rationale: Respiratory or cardiac arrest (or both) can occur from shock.
♦ If the burn is extensive, cover it with a dry nonstick, sterile dressing. Do not use gauze. Rationale: Gauze will peel off additional tissue and cause more damage. For all large burns, use only a dry sterile dressing, following removal of the heat source and cooling down period. Rationale: The dressing will help prevent infection.
♦ Keep dressings cool and wet. Be sure to keep person warm and monitor for hypothermia. Rationale: Wet dressings may promote hypothermia.
♦ Prevent contamination of the wound as much as possible. Rationale: Infection is a major hazard with burns.
♦ Treat for shock. Rationale: Pain, loss of body fluids, and anxiety contribute to shock.
♦ Determine what first-aid measures others have already given. Rationale: Some of these measures may be dangerous. Emergency and medical personnel need to be aware of what has been done.
• Burned or singed nasal hairs or burns in or around the mouth
• Flecks of soot in the client’s saliva
• Smell of smoke on the client’s breath
• Hoarse voice
Remember, a person can experience a burn internally, such as from inhaling hot air or smoke or from swallowing a caustic substance. These injuries can be life threatening. The trachea and lungs can be burned or severely eroded. The gases in smoke can replace the air in the lungs, rendering the person unable to oxygenate his or her blood. In any case of suspected inhalation injury, immediately transport the person for emergency care.
Nursing Alert If a burned person was trapped in a confined space and exposed to chemicals or smoke, suspect smoke or heat inhalation injury
Inflicted Burns
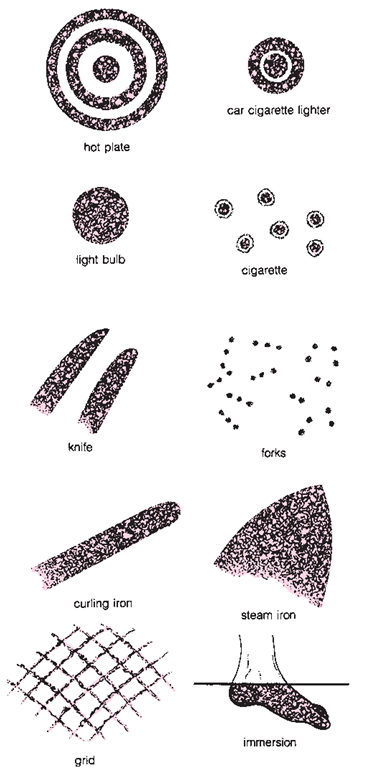
In certain mental disorders, such as borderline personality disorder, a burn may be self-inflicted by the person. Also, a common method of child abuse is to inflict a burn on a child, often in a location that is covered by clothing. Figure 43-9 illustrates suspicious burn patterns. Any such burn pattern should be immediately investigated and reported to the authorities, particularly in the case of a child or vulnerable adult (mentally challenged, mentally ill, frail elderly).
Near Drowning
Drowning is suffocation from submersion in liquid. Near drowning implies that recovery has occurred after submersion. Most drownings occur in swimming pools, lakes, rivers, and oceans. However, children can drown in the toilet, bathtub, wading pool, or a bucket. Assess victims of near drowning for associated injuries or illnesses, such as cardiac arrest, airway obstruction, head injury, spinal injury, and internal injuries. Long-term brain damage may result from extended anoxia (absence of oxygen). Submersion in cold water may also cause hypothermia; however, individuals submerged in cold water may survive because when body temperature is lowered, metabolism slows, which decreases the brain’s need for oxygen. Victims of near drowning may appear dead because of the reduction in brain and cardiovascular function. However, rescuers should initiate and continue lifesaving measures, including CPR, until the person can be evaluated with instruments such as an electroencephalogram. People may respond to prolonged resuscitation efforts without sustaining brain damage after near drowning. This is particularly true of children. Treat all near drowning victims for hypothermia and shock. Maintain respirations and blood pressure until the person is cleared medically.
Musculoskeletal Injuries
Musculoskeletal injuries are those involving bones, muscles, or joints.
FIGURE 43-9 · Look for specific patterns in burns, some of which indicate that they are self-inflicted or inflicted by an abuser. All instances of suspected abuse must be reported to the appropriate authorities.