SUDDEN DEATH AND LIFE SUPPORT
Sudden death occurs any time breathing and the heartbeat stop abruptly or unexpectedly (cardiopulmonary arrest). It is important for all nursing students and graduate nurses to maintain current certification in CPR, to be able to assist in a sudden death emergency.
Causes of sudden death include:
• Electrocution and severe electric shock
• Drowning and near drowning
• Anaphylaxis (severe allergic reaction)
• Drug overdose
• Poisoning
• Shock
• Myocardial infarction (heart attack)
• Stroke (cerebrovascular accident)
• Total airway obstruction or suffocation
• Smoke inhalation, carbon monoxide poisoning, inhalation of other gases
• Severe trauma
• Adverse reaction to general anesthesia
Two definitions for death exist: clinical and biological. Clinical death occurs when a person’s breathing and heartbeat stop. This type of sudden death may be reversible, with prompt action by people trained in basic and advanced life support. The term biological death refers to permanent damage and death of most brain cells, due to lack of oxygen. Biological death is irreversible.
Basic Cardiac Life Support
Basic life support (BLS), also called basic cardiac life support (BCLS), includes rapid entry into the EMS, performance of CPR, and use of techniques to clear an obstructed airway.
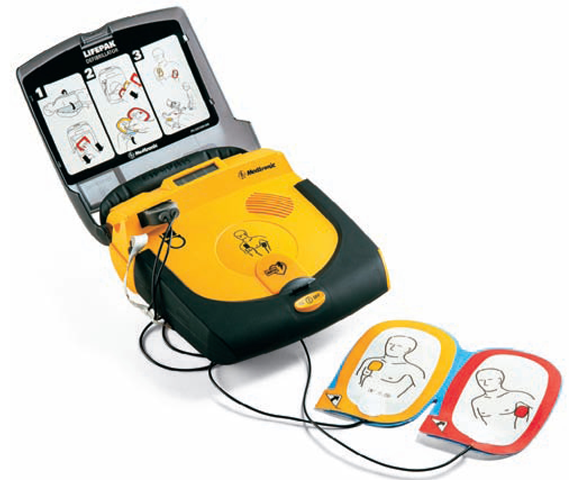
The automated external defibrillator (AED) or public external defibrillator is considered the definitive initial treatment of victims in cardiac arrest (Fig. 43-6). The American Heart Association has expanded its standard of care to include the AED in BCLS.
FIGURE 43-6 · Many people in the community, such as police officers, school employees, and the general public, have been trained to use the automated external defibrillator (AED). The paddles are applied, and the machine gives prompts to the rescuer as to what to do. Many public places have an AED onsite.
The AED is a portable unit, with electronic paddles that attach to persons who are pulseless, unresponsive, and not breathing. The unit analyzes the heart’s rhythm and indicates the appropriate action to take. If it detects a shockable dysrhythmia, the unit will indicate that a shock is necessary and will automatically charge itself for delivery when the button is pushed. If an AED is available when you are involved in an emergency, defibrillation should be initiated before beginning CPR. The AED is best used by trained personnel, but can be used by the general public if a trained person is not available. Training in the use of the AED is often included in CPR classes for healthcare personnel.
Cardiopulmonary resuscitation is a technique that artificially supports circulation and ventilation for a victim of cardiopulmonary arrest. It helps to provide oxygen to the brain, heart, lungs, and other organs until advanced life support can be given. CPR must be performed immediately after cardiac and respiratory arrest, or it will not reverse clinical death and biological death will follow. The American Heart Association and the American Red Cross have established guidelines for CPR. They make changes as new medical and emergency techniques are developed. All healthcare workers are expected to keep up to date on the latest techniques. To maintain CPR certification, a refresher course is required every 2 years.
Compression-Only CPR
Recently, the concept of Continuous-Chest-Compression or Compression-Only CPR has been introduced for the victim of respiratory arrest. It is intended to be used by lay people. This procedure is not recommended in unwitnessed collapses or with unresponsive infants or children. It also should not be used if the collapse appears not to be related to a heart disorder; this would include choking, drowning, or drug overdose. If an adult is seen to collapse, the EMS system is activated first. Then, if the victim is not responsive and not breathing, an airway is established and continuous chest compressions are given at about 100 per minute until a trained person can take over. In this case, rescue breathing is not done.
Advanced Cardiac Life Support
Emergency medical technicians (EMTs), paramedics, and many nurses are trained in advanced cardiac life support (ACLS) techniques. ACLS includes starting intravenous (IV) lines, administering fluids and medications, using defibrillation and cardiac monitoring, administering oxygen, and opening and maintaining the airway, sometimes by inserting a tube into the person’s trachea, called intubation.
In the healthcare facility, nurses usually perform rescue techniques under a primary healthcare provider’s supervision or have standing orders in case of respiratory and/or cardiac arrest. At the scene of an accident or in the client’s home, however, the nurse does not have such orders and must function as a lay rescuer or first-aid person.
Continued Assistance
As soon as medical or paramedical assistance arrives at the scene of an accident, the nurse’s role is to assist.
The Client at Home
When providing care to a client at home, plans for emergencies are included in the client’s initial plan of care. Keep in mind the following:
• Know the client’s DNR (do not resuscitate) and DNI (do not intubate) status before beginning care. If the client is DNR/DNI, a copy of the documentation must be in the home-care records.
• Review plans for resuscitation with the client and family before administering even routine care. The client’s family must be comfortable with the DNR/DNI status if this is the case.
• Carry a pocket mask and gloves at all times, in case of emergency.
• Teach the family how to perform CPR if the client is “full code” (not DNR/DNI). This is a helpful skill for all people.
Unless specified as DNR or DNI, the client receiving home care is to be resuscitated. In this case, if the client goes into cardiac or respiratory arrest while you are in the home, do the following:
• Have a family member call 911.
• Begin CPR immediately. (It is important for all home care personnel to have this training.)
• Before the ambulance arrives, have a family member turn on the porch light and watch for the ambulance.
• Ask the family to move furniture to clear a pathway to the client.
• Reassure the family after the event.
• Document the event and its outcome.
Code in a Healthcare Facility
When an emergency occurs in a healthcare facility, the nurse must activate the agency’s signal for a code. (“Code blue” or “Dr. Blue” are common signals for a cardiopulmonary emergency.)
Assisting With a Code
Obtain necessary emergency equipment: crash cart, back board, manual breathing bag, emergency medications, heart monitor, stethoscope, blood pressure and oxygen apparatus, IV lines, suctioning equipment, and oral airways. Crash carts are usually standardized throughout a facility so everyone is familiar with the setup (Fig. 43-7). The carts may be equipped with color-coded resuscitation tape (Broselow tape) for pediatric emergencies; this color-coded system gives equipment sizes, drug doses, and defibrillation settings based on height and body build.
During resuscitation attempts, the nurse assists the code team. Duties include locating emergency medications and administering them as ordered; helping set up emergency IV, suction, or oxygen equipment; keeping records of medications and treatments given; and calling in other personnel as needed.
If resuscitation measures are successful, the person’s pulse will resume, pupils will constrict, color will improve, and breathing will begin. The person may cough, move, or vomit.
FIGURE 43-7 · The crash cart contains emergency medications and equipment. A backboard is often attached to the cart or hanging nearby.
If assisting a code team and suction is available, turn the client’s head to the side and suction the mouth. Do not place fingers in the client’s mouth. If it is necessary to open the client’s mouth, use an instrument, such as a tongue depressor or a spoon. Always wear gloves.
After the person is resuscitated, a mechanical ventilator, IV therapy, or vasopressor drugs may be needed for maintenance. Until the primary healthcare provider decides the person is out of danger, the person needs close observation in the ED or intensive care unit (ICU) in case another emergency resuscitation is required.
The entire procedure is documented, including the time the arrest was discovered and the primary provider’s estimate of when the arrest occurred; emergency measures taken by the first person on the scene; the time the code team arrived; procedures performed from that time on and by whom; medications given, stating dosages and times; the victim’s responses to medications and treatment; and laboratory work, electrocardiograms, x-rays, and other tests done. Finally, the outcome of the resuscitation efforts and subsequent nursing care, if appropriate, are noted. A report as a “sentinel event” is required by most healthcare facilities.
Key Concept A code may be called for other than a cardiopulmonary emergency For example, if a person with diabetes experiences a very low blood sugar (usually less than 35 or 40 mg/dL), he or she may become unresponsive. This is usually a code or "rapid response” situation in a healthcare facility.
In addition, a code may be called in the event of strangulation, such as the person who tries to hang himself or herself, or smothering, due to inappropriate pillow placement.
FIRST-AID MEASURES
All nurses are expected to know basic first-aid measures. This knowledge will also prove beneficial to the nurse in his or her role as a parent, sports coach, or neighbor. No one can predict when an injury or sudden illness will occur or when a person may be called on to assist.
Key Concept Remember: You are expected to perform first aid only to the level of your training and experience, and local laws.
Chest, Back, Neck, and Head Injuries
Do not attempt to move or transport any injured person, particularly a person with a chest, back, neck, or head injury, until the EMS team arrives, except in unusual situations. If the person must be moved, only persons who have special instruction and equipment should do so. The only time unqualified people should attempt extrication is when the person is in great danger if he or she is not moved. For example, you may be on a canoe trip or mountain climbing in the wilderness without available EMS assistance, or the person may be in a dangerous situation such as a burning building, a car under water, or a car that may explode. In this case, the person must be moved, even though moving him or her might aggravate the injuries. In cases such as these, you will need to supervise the cautious extrication (emergency removal) of the victim.
Moving any injured person requires the utmost care. Careless transport can compound an injury. When moving a person with a neck injury to a stretcher, immobilize his or her neck and back first, then keep the body straight. Sometimes, if the person is lying in an abnormal position, putting that person on the stretcher in this same position may be easier and safer than trying to straighten the body. Enlist as many assistants as needed to move the person effectively and safely. Rationale: Doing so protects both the injured person and the rescuer.
Chest Injuries
Blows, stabbings, shootings, and MVAs are the most common causes of chest injuries. CPR may also cause fractured ribs. Fractured ribs may injure soft tissues by puncturing a lung or tearing blood vessels. When such complications are not present, treat fractured ribs by immobilizing the person’s chest with an elastic bandage.
Chest compression that results from an explosion or an MVA may rupture a lung and cause death from hemorrhage or suffocation. Wounds that penetrate the chest are serious and require immediate first aid. An open chest wound allows air to enter the chest cavity, compressing the lungs. (The normal vacuum within the chest cavity is disrupted.) Normal breathing fails, because the lungs cannot adequately expand. This condition is called pneumothorax. Signs of pneumothorax include difficult breathing, weak and rapid pulse, restlessness, distended neck veins, hypotension, chest and shoulder pain, and cyanosis.
If it is determined that pneumothorax is present, seal the wound in any way possible: use aluminum foil, petroleum jelly (Vaseline) gauze, plastic wrap, or a rolled-up dressing. Holding something over an open chest wound for a period of time may be necessary until medical assistance can be obtained. Sealing will help the lungs re-expand. Tape a dressing on three sides so that air can escape when pressure builds in the chest. After the client arrives at a healthcare facility, chest tubes will be inserted for continuous, closed drainage.
When transporting a person whose chest has been punctured by a foreign object, make sure that the object remains in place. If the wound is open, cover it at once with an occlusive dressing. Hold the dressing in place with a gloved hand. Oxygen is helpful, and mask-to-mouth or manual breathing bag resuscitation may be needed. If the person’s condition seems to worsen, loosen the dressing to let out some air that is building up in the chest, to prevent a tension pneumothorax (described below); then reseal the wound.
A tension pneumothorax is particularly dangerous. This situation occurs when air leaks out of the lung or bronchus into the chest cavity and cannot escape. As the leak continues, air collects and pressure builds in the chest. The lung on the same side of the chest as the leak collapses because of the excess pressure. In this case, breath sounds will be greatly diminished or absent on the affected side. A tension pneumothorax that remains uncorrected will worsen, resulting in a mediastinal shift. The heart, great vessels, and trachea shift to the side opposite the injury, the unaffected side, as a result of the building air pressure on the affected side. This then prevents the unaffected lung from expanding. In addition, the amount of blood returning to the heart to be pumped to the body will diminish, as will the ability of the heart to pump, resulting in rapid progression toward death. A primary healthcare provider or emergency person may place a large-bore IV needle or chest tube through the chest wall to relieve excess air pressure.
Nursing Alert In an emergency do not remove an article puncturing the chest if it is still in place. Rationale: The article will help seal the hole; its removal may cause added damage. Surgical removal is necessary under controlled conditions.
Back and Neck Injuries
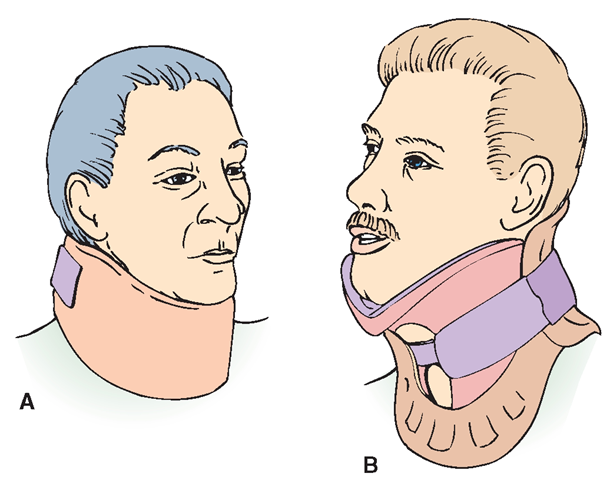
When a person is a victim of an MVA or a fall, suspect a neck or back injury. A great danger exists for further injury, particularly to the spinal cord, by moving the person without proper preparation. Always treat the person who has been injured as though he or she has a back or neck injury until such is proved otherwise. Immobilizing devices, such as the cervical collar, head blocks, or the back board, are applied by EMS personnel before the person is moved (Fig. 43-8). It is better to be too careful than to risk causing further injury. Only specially trained personnel should apply immobilizing devices except in extreme circumstances when assistance is not available.
FIGURE 43-8 · (A) A foam cervical collar. (B) A rigid cervical collar; Untrained personnel should not attempt to apply a cervical collar, except in an extreme emergency.
Head Injuries
Scalp lacerations cause profuse bleeding, making even the smallest wound appear very serious. Determining the extent and cause of the injury is important. A blow to the head that causes a laceration may also cause injury to the skull or brain. Observe for blood or fluid draining from the nose or ears (with no known injury to the nose), bruising behind the ears or under the eyes, persistent bleeding, or a change in behavior since the accident. These are all serious danger signs.
Emergency care for a potential head injury includes having the person lie flat while restricting his or her movements. Do not lower the person’s head! Keep the person warm and check for signs of increasing intracranial pressure (ICP; see below). Apply an ice pack to the area of injury. Instruct family to watch for signs of complications every 2 hours for the first 24 hours. Always advise the client to see a physician after any head injury.
Nursing Alert Any person who has a head injury no matter how minor, should be observed carefully for at least 24 hours. Late complications can occur.
Monitoring for signs of increased ICP is crucial. Serious signs of increasing ICP include:
• Confusion, disorientation, or agitation
• Loss of memory
• Any change in vision, such as blurred vision or double vision
• Decreased LOC or difficulty arousing; extreme lethargy
• Numbness, tingling, or weakness in an arm or leg
• Persistent vomiting (sometimes projectile)
• Severe headache
• Speech problems
• Seizures
If the person with a head injury must be moved, his or her head must be stabilized in a neutral position and in line with the back. Emergency personnel provide immobilizing equipment, such as cervical collars, head blocks, and short and long spine boards, which they will use to prepare the person for transport. Stabilize the person without moving him or her, until proper equipment and assistance arrive.
Cold-Related Injuries
Severe injuries, even death, can result from exposure to cold. Serious injuries can occur even if the temperature is not extreme. Factors influencing cold-related injuries include:
• Temperature
• Wind chill factor
• Wetness
• Length of exposure time
• Part of the body exposed
• Other injury or irritation, such as blisters on the feet or tight shoes
• Person’s age and mental status
• Circulatory status
• Nutritional and hydration status
• General physical condition
• Drug or alcohol use
Cold injuries can occur if body parts are exposed, because the body automatically cuts down blood flow to the peripheral structures and redirects it to the vital organs (heart and brain) if it becomes too cold.
Frostbite
Frostbite is the freezing of body tissues that results from exposure to cold temperatures. The body part becomes so cold that ice crystals form in the spaces surrounding the cells; the cells then die. The body is most vulnerable to frostbite when there is a high wind, because blood rushes to the skin to warm it, then cools quickly due to rapid heat loss. The mathematical calculation of temperature and wind speed is called the wind chill factor. Skin can freeze when the wind chill factor is below the freezing point, even if the actual air temperature is considerably higher. If the person is wet, this factor increases the possibility of frostbite.
Frostbite is most likely to affect hands, feet, noses, ears, and cheeks. Noses, ears, and cheeks are vulnerable because they are continually exposed; hands and feet are vulnerable because circulation to these areas is slowest. However, larger body surface areas can be affected as well.
Nursing Alert If you work in a public health care facility in a cold climate, you will likely see frostbite among homeless people, especially those who are mentally ill, inebriated, elderly, or physically debilitated.
When a body part becomes frostbitten, the area is first painful and then numb. The frostbitten part is pale and cool to the touch and feels like a block of wood or marble. These symptoms exist initially, regardless of how mild or severe the frostbite. In late stages, hemorrhage may occur; the part may swell and blisters may form. The skin may slough off; gangrene can occur. Box 43-3 presents degrees of frostbite. In general, frostbite looks like a burn. If it is gangrenous, it turns black and looks crusty.
BOX 43-3.
Degrees of Frostbite
♦ First degree (superficial):Temporary tenderness, reddened skin, some peeling may occur—usually no permanent damage. Sometimes called frostnip.
♦ Second degree (partial-thickness): Blisters and some tissue and nerve damage—can result in permanent hypersensitivity to cold and increased risk of future frostbite. Subsequent exposure to even mild cold can cause chilblains (painful chilling and burning sensations). Sometimes called pernio; may persist for years.
♦ Third degree (full-thickness): Tissue death—often includes nerve and bone damage. Often leads to gangrene, even if treated. Usually requires skin grafting or amputation. Often treated in a Burn Center in the same manner as a burn.
A person suffering from frostbite needs immediate assistance. Do not rub a frostbitten part to restore circulation. Rubbing, particularly with snow, will only increase the damage and can contribute to gangrene. Protect frozen body parts and handle them gently. Loosen tight clothing. Do not allow the person to walk on a frostbitten foot. Separate frozen fingers and toes with cotton wedges; however, do not use bandages, ointments, or salves.
Place frozen parts in water that is between 98°F and 104°F (36.6°C and 40°C). If a thermometer is not available, use water temperature that feels tepid (lukewarm). Rewarming the affected part in water will take about 20 to 45 minutes. The person may experience some pain as the part warms. The part will turn pink or bright red as circulation resumes. Protect the part against refreezing.
The person with severe frostbite needs immediate medical attention. It sometimes takes providers several days to assess the extent of damage. Treatment is often the same as for a burn, with treatment commonly being provided in a Burn Unit. If treatment is unsuccessful, amputation may be necessary. In severe frostbite, blisters form quickly. They should not be broken.
Immersion Foot
Immersion foot occurs most often in hikers and canoers when the feet are kept in moist, cold boots for several days. It can also occur in military personnel who spend several days in the field. In rare cases, this condition can affect the hands. The feet (or hands) should be gently warmed, cleaned, dried, and elevated. Because infection often occurs, antibiotics are often given, as well as a tetanus booster.