COLLECTION OF CLIENT DATA ABOUT PAIN
Pain is subjective; that is, only the client can describe it. Although it cannot be measured objectively, some manifestations of pain can be observed. Keep in mind that the client’s culture may also affect how the client expresses pain.The practical/vocational nurse is vital in helping to collect information regarding pain from the client.
Special Considerations: CULTURE & ETHNICITY
Expressions of Pain
The expression of pain is often related to cultural and ethnic factors.
These factors include, but are not limited, to:
• Beliefs about the causes of pain (i.e., evil spirits, punishment from God, guilt [e.g., Greek])
• Manner of expressing the pain in that specific culture (e.g., stoic— Native American; expressing pain—Jewish)
• Gender differences in the expression of pain (men versus women)
• Acceptance of traditional versus nontraditional medicine
• Belief that pain is related to the imbalance of yin and yang or hot and cold (Chinese)
• Relationship between pain and immoral behavior (Mexican)
• Spiritual and religious beliefs may contribute to high pain tolerance (African American)
Pain as the Fifth Vital Sign
The Joint Commission regulations state that pain is to be assessed whenever other vital signs are measured. That is, clients are to be asked on a regular basis if they are experiencing pain. Pain is now considered to be the fifth vital sign (temperature, pulse, respiration, blood pressure, and pain). Failure to ask about pain may result in a citation from the Joint Commission. The evaluation of pain, along with other vital signs, alerts the nurse and other healthcare providers to the necessity of addressing the client’s pain. Relief of pain helps the client to be more comfortable and to recover more quickly.
The Joint Commission has developed the following accreditation standards in an attempt to improve the management of pain (The Joint Commission, 2011):
• Patients have the right to appropriate assessment and management of pain.
• On-going pain assessment should include the nature and intensity of pain.
• Responses to evaluation of pain should be recorded in a manner that promotes regular reassessment and follow-up.
• Staff must be oriented and competent in assessment and management of pain.
• Policies and procedures supporting ordering of pain medications must be in place.
• Patients and families require education about effective pain management.
• Discharge planning should address the patient’s needs for management of pain.
Key Concept The documentation of pain includes:
• Level of pain
• Description of pain
• Action taken
• Results
Pain Rating Scales
The Joint Commission requires healthcare facilities to use pain scales to help clients determine their level of pain.
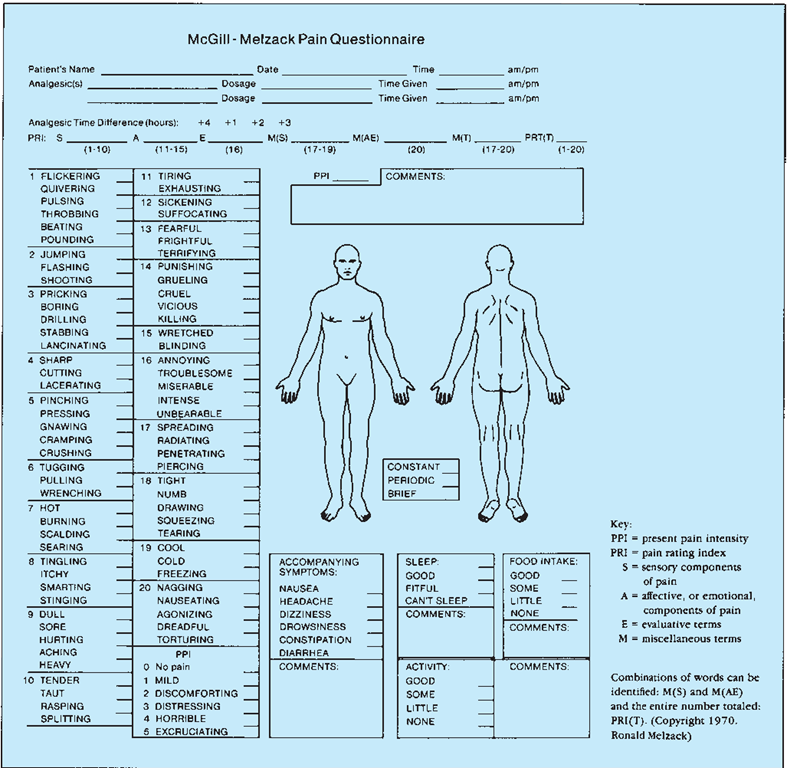
FIGURE 55-3 · The McGill-Melzack Pain Questionnaire is a comprehensive way in which to obtain information about a client’s pain.
A number of pain scales that can help in quantifying pain are presented in this topic. These scales ask clients to rate their pain, as compared with the choices on the scale.
Rating scales such as the Pain Intensity Scale or Pain Distress Scale usually are reserved for children older than 7 years and for adults. On these scales, the client is asked to rate his or her pain by choosing descriptive words, by choosing the appropriate number on a numerical scale from 0 (no pain) to 10 (unbearable pain), or to choose a location on a linear scale (visual analog scale—VAS) (see Fig. 55-2). The person must understand what each number means. A child must be old enough to understand the concepts of “more than” and “less than” to use these scales.
Another method of rating the intensity of pain uses a pain questionnaire, such as the McGill-Melzack Pain Questionnaire (Fig. 55-3).
The Wong-Baker Faces Pain Scale (a picture scale) was developed primarily for verbal children between the ages of 3 and 7 years. However, it can also be used for adults who have difficulty expressing themselves or people who do not speak the prevailing language in the facility (Fig. 55-4). The client is asked to choose the face that best describes how he or she is feeling because of the hurt or pain being experienced. The explanation given to the client states that the face on the left is happy because he or she has no pain and the face on the right has as much pain as you can imagine, although you do not have to be crying to feel this badly. It is recommended that one of the other rating scales be used for the child older than 7 years and for most adults.
FIGURE 55-4 · The Wong-Baker Faces Pain Scale is an example of a picture scale. It is recommended for children ages 3 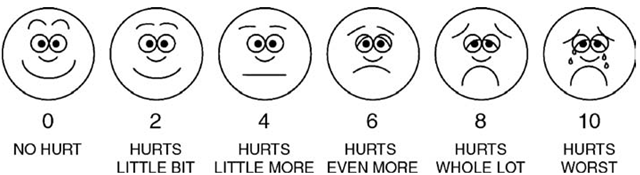 to 7. Point to each face using the words to describe the pain intensity. Ask the child to choose face that best describes own pain and record the appropriate number.
to 7. Point to each face using the words to describe the pain intensity. Ask the child to choose face that best describes own pain and record the appropriate number.
Another tool is available for use with preverbal children, usually those younger than 3 years. The nurse observes the child’s face, legs, activity, cry, and consolability (FLACC). This tool depends on the caregiver’s accurate observational skills because the child cannot verbally describe the pain (Table 55-2). Another scale that is similar to the FLACC is called NIPS (Neonatal/Infant Pain Scale). The NIPS is based on observations of facial expression, cry, breathing, arms, legs, and state of arousal.
Description of Pain
In addition to determining the level of pain, other information must be obtained from the client who alone can tell you this information.In Practice: Data Gathering in Nursing 55-1 provides more detail in the use of this memory guide.
Many terms can be used to describe pain characteristics. Examples include the following:
• Character: The client may describe the character of pain with terms such as aching, burning, cramping, crushing, drilling, dull, grinding, hammering, knife-like, mangling, penetrating, piercing, pounding, radiating, sharp, shooting, stabbing, tearing, throbbing, tingling, or undulating.
• Duration: The client may describe the duration of pain as occasional, intermittent, spasmodic, or constant.
• Severity: The intensity or severity of pain may be described as mild, slight, moderate, severe, or excruciating. (The client’s descriptions of the intensity will help the provider determine appropriate medication or other appropriate interventions.)
• Associated factors: Associated sequelae (consequences) of unrelieved pain may include visual disturbances, nausea and vomiting, fatigue, depression and suicidal thought, anorexia, muscle spasms, anger and aggression, withdrawal, tearfulness, or regression.
Key Concept After pain is identified, focus nursing care and client and family teaching on breaking the cycle of chronic pain as soon as possible.
PAIN MANAGEMENT
Successful management of pain is a primary goal of the healthcare provider and the nursing staff. A number of interventions are used in the management of pain. Pain management is very individual, and an intervention that is successful for one client may not be successful for another. Often, a number of interventions must be tried before one, or a combination, is successful. Pharmacology, the administration of medications, is often the cornerstone of successful pain management.
A number of nursing interventions may also be helpful. In addition, the primary healthcare provider may order alternative or complementary interventions that are provided by a specially trained person.
TABLE 55-2. The FLACC Nonverbal Pain Scale*
|
SCORE |
0 |
1 |
2 |
|
Face |
No particular expression or smile |
Occasional grimace or frown, withdrawn, disinterested |
Frequent to constant quivering chin, clenched jaw |
|
Legs |
Normal position or relaxed |
Uneasy, restless, tense |
Kicking or legs drawn up |
|
Activity |
Lying quietly, normal position, moves easily |
Squirming, shifting back and forth, tense |
Arched, rigid, or jerking |
|
Cry |
No cry (awake or asleep) |
Moans or whimpers, occasional complaints |
Crying steadily, screams or sobs, frequent complaints |
|
Consolability |
Content, relaxed |
Reassured by occasional touching, hugging, or being talked to, distractible |
Difficult to console or comfort |
*Score each category 0 to 2. The total score will range from 0 to 10.
This scale is appropriate for clients younger than 3 years and who are preverbal. It has been validated at ages from 2 months tc 7 years, but is usually not recommended for children who can signal or point to their level of pain on a scale, such as the Wong-Baker Faces Pain Scale. This scale may also be used for severely intellectually impaired clients. Do not use if the child is receiving paralytic medications.
IN PRACTICE DATA GATHERING INNURSING 55-1
THE PAIN EXPERIENCE
The nurse should note the client’s nonverbal reactions and responses to pain. The COLDSPA memory guide will help in gathering data about the client’s pain in an organized manner.
Character: Describe the pain. How does it feel? Be specific. Is the pain constant, occasional, or recurring?
Onset: When did the pain start? How long have you had it?
Location: Where is the pain? Is it internal or external? Does it radiate? Where does it start and where does it radiate to? Is it always in the same place?
Duration: How long have you had the pain? How long does it last? Does it come back? How often?
Severity: How bad is the pain? (Use an appropriate rating scale to assist the client.)
Pattern: Does anything relieve the pain? What are you doing to relieve the pain? Does anything make it worse? Does anything specific seem to cause the pain?
Associated Factors or Related Occurrences: Are other symptoms associated with the pain (headache, visual difficulties, sensitivity to light, nausea)? Are any obvious cultural factors involved? Have you had this same type of pain in the past? Is anything particularly stressful occurring in your life at this time? Have you had any recent injury or illness that might contribute to or cause this pain? Has anyone in your family had a similar type of pain? Have you been injured or threatened by anyone in the past year? Are you interested in counseling?
Special Note
• Remember to check back with the client after giving medications or performing other interventions to determine results. Document all interventions and their results.
Pharmacologic Therapy
Analgesics are medications that relieve pain. Analgesia is usually most effective when given on a regular basis or at the very onset of pain. The preventive approach is recommended (e.g., give analgesics immediately after surgery or before a painful treatment). If medication is given before pain occurs, the pain is often easier to control. A needed analgesic that is withheld for too long may be ineffective when given. Some clients are allowed to administer their own analgesia through a patient-controlled analgesia (PCA) pump (Fig. 55-5).
Analgesics generally provide pain relief by altering the body’s sodium and potassium levels, thus slowing or halting pain transmission (Taylor, Lillis, LeMone, & Lynn, 2008). Three classes of analgesics are commonly used for pain relief. These are:
• Nonopioid nonsteroidal anti-inflammatory drugs (NSAIDs): Examples of NSAIDs include aspirin, ibuprofen (Motrin), and naproxen (Naprosyn, Aleve). These drugs are usually given to clients who are experiencing mild to moderate pain. Another nonopioid analgesic commonly used for mild pain is acetaminophen (Tylenol).
• Opioids/narcotic analgesics: The most commonly used example is morphine (and its derivatives). Opioids are usually used to manage pain in clients with moderate to severe pain.
FIGURE 55-5 · A patient-controlled analgesia (PCA) pump allows clients to administer their own analgesia. Many are smaller and easier to carry around if the client is ambulatory
• Adjuvant drugs: An adjuvant medication is one that is usually used for other purposes but may also help with pain. Common examples include anticonvulsants and antidepressants. These medications can help improve the client’s mood, thus assisting in muscle relaxation. When muscles are relaxed, pain improves and endorphin production often increases.
Ointments and liniments that contain local anesthetics may provide pain relief. Such medications may also draw blood into the painful area to increase temperature and improve circulation. Many other pharmacologic agents are used to manage pain. Many of these are discussed in Unit 9.
Nursing Alert Dependence on pain medications usually does not occur when the client needs relief from acute pain. However; these medications, especially opioids, should not be used on a long-term basis.
Surgical Intervention
Surgery may be necessary to alleviate certain types of chronic pain. For example, when a herniated disk is the cause of lower back pain, the disk may be removed. Physical causes, such as tumors causing pressure, or pinched nerves, can be treated with surgical intervention. In addition, the nerves transmitting the pain sensation may be cut (ablation surgery). However, with the advent of many less invasive techniques, this surgery is rarely used today.
Nursing Interventions
Empathie nursing care can help provide pain relief. There are a number of things the nurse can do to help relieve the client’s pain. These nursing interventions include providing diversion or music, changing the client’s position, bathing the client, giving a back rub, or massaging the client’s hands. The healthcare provider may order the application of heat or cold or other treatments. Keep in mind that these methods are often used to complement, not replace, pharmacologic interventions. Some clients, particularly those with a terminal illness, may experience long-term and severe intractable pain, which is difficult to manage.See the Nursing Process section at the end of this topic for further description of applying the nursing process to pain management.
NCLEX Alert Throughout the examination,you will demonstrate your knowledge as you relate the collection of data to the selection of nursing actions to control and manage clients’ pain. Suggestions for documentation of pain—level, description, action taken, and results—are provided to you in this topic
Comfort Measures
The nurse can independently perform a number of comfort measures aimed at helping the client deal with pain or at relieving pain. A clean bed, clean face and hands, restful music, warm room, or a semilighted room may promote relaxation, which in turn may help lessen pain. Positional changes can also help. The client is encouraged to eat a nutritious diet and to obtain adequate fluids. Offer fluids often, including nutritional supplements, if ordered. It is important to assist with elimination by monitoring voiding and bowel patterns and by offering ordered medications to prevent constipation and diarrhea.
Physical Measures
Physical measures can be used in addition to pharmacologic pain management interventions.
Physical Stimulus (Cutaneous Stimulation)
Gentle massage or pressure may relieve congestion or promote circulation and oxygenation, and thus help to relieve pain. This may be applied by gently massaging a painful area or more generally by giving a backrub.
Specific and accurately directed stimulation is applied by using the transcutaneous electrical nerve stimulation (TENS) unit (Fig. 55-6). TENS is a technique that allows the client to wear an electronic device and trigger an electrical stimulation when he or she feels pain. This gentle electrical shock blocks pain, allowing muscles to relax. The shock also stimulates the production of endorphins. Other, more invasive, methods are also used but are beyond the scope of this text.