Turning and Moving Clients
As a nurse, you will be required to turn and move clients on a daily basis. It is important to do so without endangering either the client or yourself.
Preventing Deformities
Any client who does not move the hands needs to have his or her hands supported in an open position to prevent contractures (permanently shortened muscles). A hand roll supports the wrists and keeps the fingers bent slightly and the thumb out (Fig. 48-6). This is the grasping position. The hand roll is made by rolling a washcloth or small towel or by using a commercially prepared hand roll. The roll is placed in the client’s hand. By doing this, the client will later be able to functionally use the hand. (Without this procedure, the muscles would pull the hand into a tight fist.)
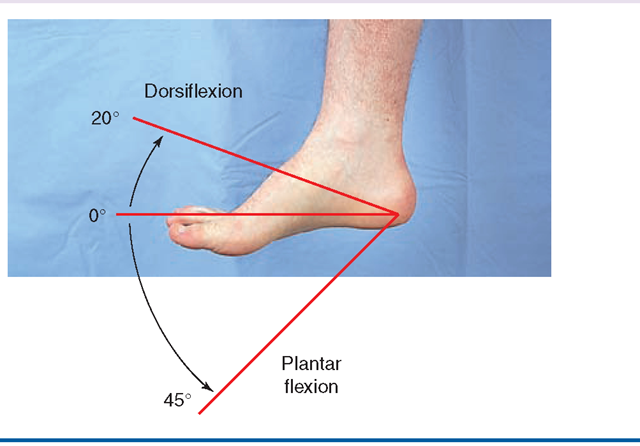
When the client is in bed, the knees are supported in a comfortable position. A slanting footboard (at about the same angle as if the person were standing) is comfortable for the feet and prevents footdrop (see Fig. 49-4). Footdrop is a contracture deformity in which the foot hangs in a plan-tarflexed position (see Fig. 49-3). This deformity prevents the heel from being placed on the ground, impeding walking. (The same sort of deformity can occur if a person wears very high heels all the time.)
The bed mattress may slip to the foot of the bed when the head of the bed is raised. Maintaining proper body alignment becomes difficult. To avoid mattress slippage, place a pillow or a rolled blanket in the space between the edge of the mattress and the foot of the bed.
NCLEX Alert Appropriate body mechanics and positioning are commonly composites of situations that include client care, client safety and prevention of the hazards of immobility.
Turning the Client to a Side-Lying Position
Proper body alignment is always important when turning a client to the side. When a person is to remain in the side-lying position for a while, he or she is turned in the same manner as if the position were temporary (for example, to receive a backrub). Then, the client is propped into the new position. In Practice: Nursing Procedure 48-1 gives the steps in turning the client to a side-lying position. Pillows may be placed as the client wishes, to add to his or her comfort.
Body Alignment With the Client on the Back (Supine Position)
Often the client prefers to lie on his or her back most of the time. This is called the supine position. (This client may return from a side-lying position to the back, if he or she is not properly supported on the side.) When the client prefers the supine or dorsal recumbent position, use pillows to support the head, neck, arms, and hands, and a footboard to support the feet. Placing the client in this position allows digestive and respiratory organs to function without being restricted. If the client’s trunk must lie more flatly than the upper part of the body, the person will need only one pillow to support the head and neck. A knee roll is placed under the knees, and a pad is placed under the ankles to prevent pressure on the heels. The footboard will be more nearly upright in this case.
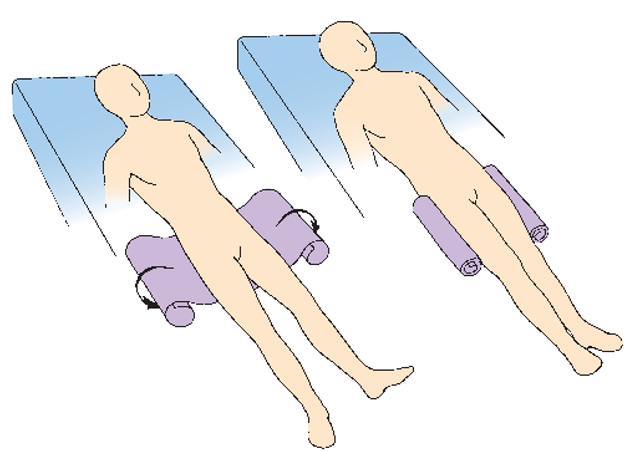
When the immobile client is to lie on the back for some time, trochanter rolls are placed on each side of the legs (Fig. 48-7). These rolls keep the legs and feet from rotating outward, causing later deformities. Trochanter rolls are made by rolling a bath blanket or by using rolls commercially prepared for this purpose.
Supporting the Client in a Sitting Position in Bed Fowler’s Position. A client may sit up for a short time to eat meals, work at the overbed table, or change position, per the primary healthcare provider’s order. The most commonly used position is called the Fowler’s position (see Table 481). (Note: the Fowler’s position is simply a variation of the supine position, in which the head of the bed is raised.) In semi-Fowler’s or low Fowler’s position, the head of the bed is raised about 30° to 45°. In high Fowler’s position, the head of the bed is raised to nearly vertical.
The Orthopneic Position. Some clients with cardiac or respiratory conditions need to sit upright continuously to make breathing easier. This condition is called orthopnea.
FIGURE 48-7 · Placement of trochanter rolls to prevent outward rotation of the legs and hips.
Putting clients in the orthopneic position will further facilitate breathing. To achieve the orthopneic position, place the overbed table across the bed or in front of a chair with one or two pillows on top of the table. Have the client lean forward across the table with his or her arms on or beside the pillows and rest his or her head on the pillows. Pillows can also be placed at the client’s back to further support the person (see Table 48-1). In the alternative orthopneic position, the client sits up straight with arms supported by pillows.
Prone Positions
The person may be positioned on the stomach (prone) for short periods, to provide variety (see Table 48-1.) The complete prone position, however, is uncomfortable for extended lengths of time because having the head turned to the side can strain the neck and cause headache.
The Semi-prone Position. The semi-prone position is a variation of the prone position or of the side-lying position. It is more comfortable than lying on the stomach and breathing is easier than in the full prone position. To place a client into a semi-prone position from a back-lying position, roll the person as in In Practice: Nursing Procedure 48-1. The major difference is that the bottom arm will be placed behind the client, rather than in front, and the client will be more on the stomach than on the side. The upper arm and leg are supported with pillows. Usually, pillows are not needed behind the person. The semi-prone position is similar to the Sims’ position but not as extreme. (See Table 48-1.)
Key Concept The client’s body alignment when lying down should be approximately the same as if the person were standing. If in doubt about moving any client, ask for assistance.
The Logroll Turn
The logroll turn is a method of turning the client that keeps the body in straight alignment (like a tree log). This method is used for clients who have spinal cord injuries or who have had back surgery. Because the goal is to turn the client’s body as one intact unit, this method is important in preventing further injuries to the back and spine. Two or three nurses are required to turn the client properly in this fashion; however, one nurse may perform this procedure in an emergency, such as if the client is vomiting.
The logroll turn may be used for bed linen changes, change of body position, or to give back care. First, the client is turned to the side using the logroll turn. This position is helpful in relieving pressure areas over bony prominences and generally adds to the client’s comfort. In clients who have an unstabilized cervical spine injury, one nurse is required to maintain the stability of the neck and to keep it in alignment. Determine the client’s ability to understand instructions and to be cooperative in the turn. In Practice: Nursing Procedure 48-2 explains the detailed steps of the logroll turn.
Key Concept A lifting sheet is often used to help move clients.This may also be called a transfer sheet, draw sheet, or turning sheet.
Nursing Alert Only specially trained clinical nurses should attempt to turn clients with an unstabilized cervical spine injury.
JOINT MOBILITY AND RANGE OF MOTION
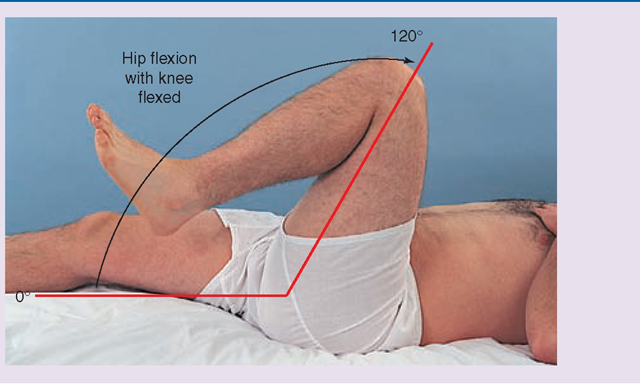
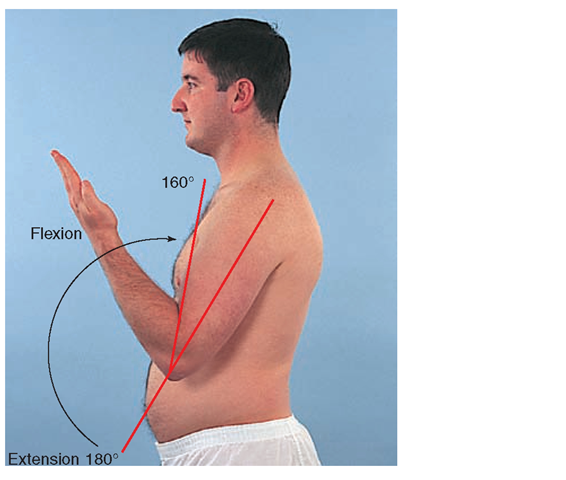
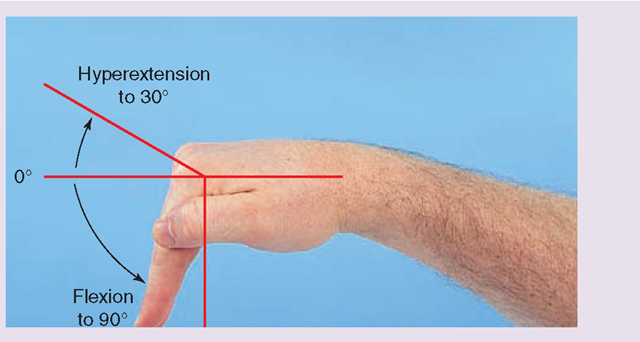
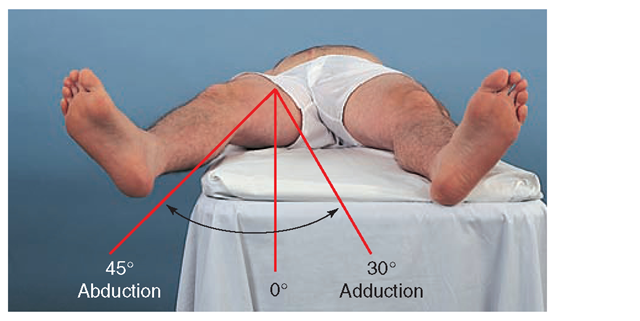
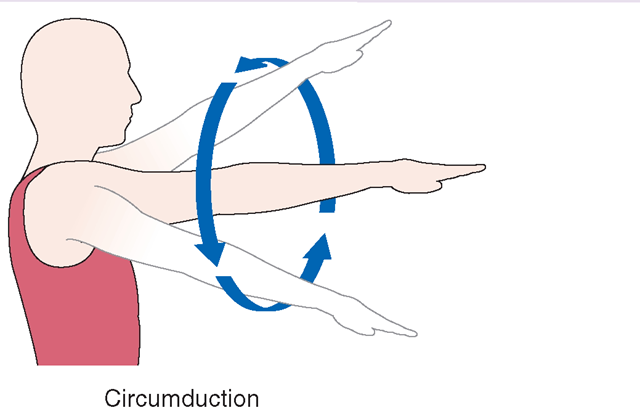
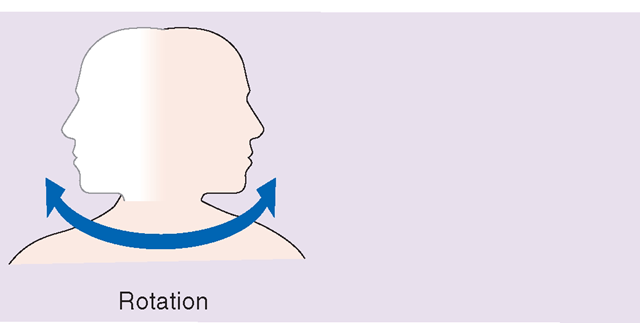
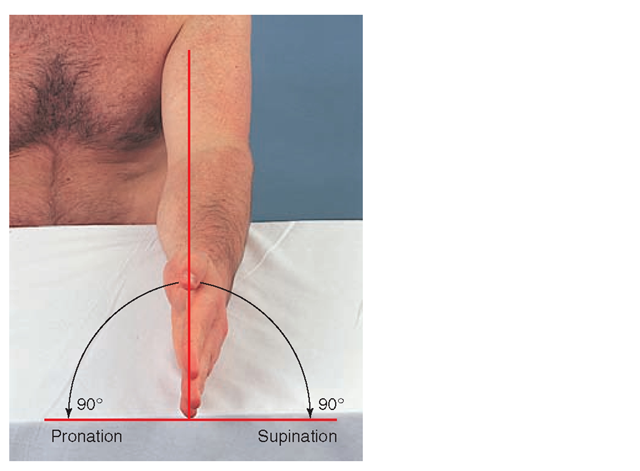
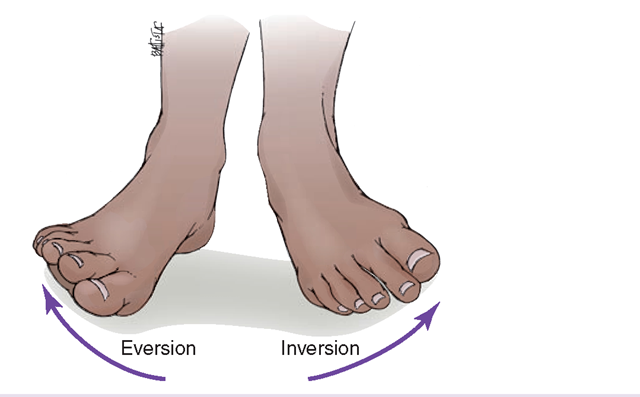
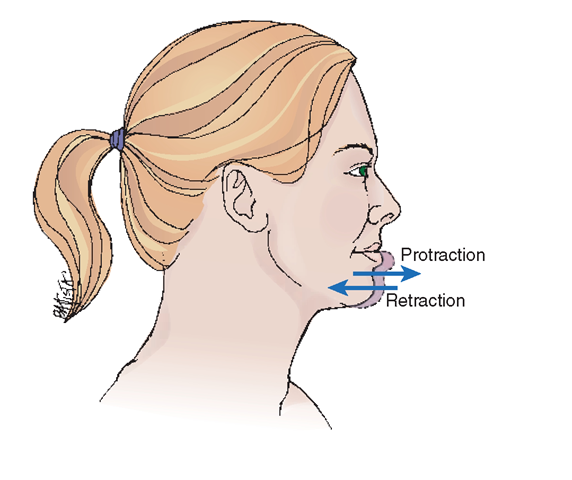
Every body joint has a specific but limited opening and closing motion that is called its range of motion (ROM).The limit of the joint’s range is between the points of resistance at which the joint will neither open nor close any further. Generally, all people have a similar ROM for their major joints. Factors such as body development, genetic inheritance, presence or absence of disease, and amount of exercise the person usually gets determine individual differences.
Table 48-2 will help you review the various motions the body can perform.Ligaments, muscles, and tendons that connect the bones control joint movement. Clients who have injuries to their tendons, muscles, or ligaments will have limited joint movement and often, pain on movement.
Every major body joint (i.e., neck, shoulder, elbow, wrist, finger, thumb, hip, knee, ankle, and toe) must move regularly several times each day to prevent stiffness and deformities. For healthy and active people, this exercise occurs normally in everyday life. For the ill or immobilized person, however, joint movement may be limited or impaired. To avoid joint abnormalities, the nurse must be sure that clients exercise all joints—several times daily—through ROM exercises.
Nursing and physical therapy share the responsibility of managing ROM exercise programs for clients. Regular exercises prevent joint deformities caused by prolonged muscle contractures. A contracture is the continuous contraction (shortening of the length) of the muscles that move the bones of the joint. Exercise also helps to prevent conditions such as hypostatic pneumonia, thrombophlebitis, footdrop, circulatory difficulties, skin breakdown, urinary disorders, fecal impactions, and depression. Attentive and frequent nursing care can minimize these problems for the immobile client.
Passive Range of Motion
If a client is unable to move, the nurse helps by performing passive range-of-motion (PROM) exercises. In PROM, the nurse or therapist moves the client’s joints and assists in assuming various positions. (If the client moves himself or herself, this is active range of motion.) In Practice: Nursing Procedure 48-3 gives information for providing PROM exercises. The physical therapist may draw up a special PROM plan for a specific client. The nurse helps to carry out this plan.
Continuous Passive Motion
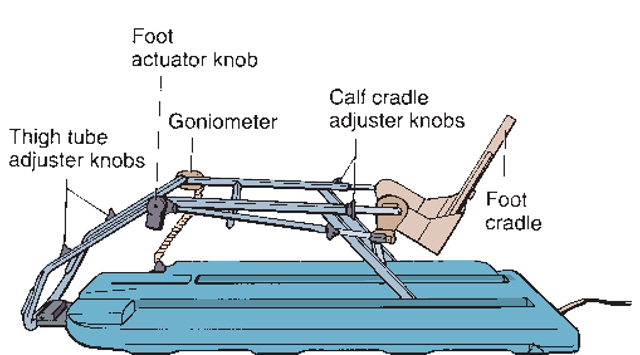
Mechanical devices which provide continuous motion to a specific joint, usually the knee or hip, are called continuous passive motion (CPM) machines. They are often used after surgery for joint replacement or arthroscopic repair of a joint. The CPM machine moves the client’s leg without effort on the part of the nurse or client. CPM exercises promote joint mobility and speed rehabilitation. It is important that the nurse carefully explain the purpose of the machine to the client to avoid anxiety. Some discomfort may also occur.
TABLE 48-2. Range of Motion in Body Movements
TABLE 48-2. Range of Motion in Body Movements Continued
TABLE 48-2. Range of Motion in Body Movements Continued
The CPM machine is electric, with a padded rack to hold the extremity (Fig. 48-8). The physical therapist or healthcare provider determines the machine’s parameters. The nurse may set the machine for the number of movements per minute (speed) it is to move and the degree of flexion of the joint, as ordered by the healthcare provider. The client’s leg is secured into the rack, with the knee joint far enough away from the end of the rack to allow flexing without rubbing the skin. Be sure the call light is placed within the client’s reach. The client is instructed to call if there is pain. It is often helpful to give a PRN (as needed) pain medication approximately 15 minutes before the CPM treatment begins, to relieve pain and allow greater joint movement during the treatment.
FIGURE 48-8 · The continuous passive motion (CPM) machine. The goniometer measures the angle of the bend in the knee joint and controls the parameters of flexion and extension of the knee. Padding is added to protect the limb.
In some cases, a client will return from surgery with the CPM machine already in place and moving. Many providers will order the CPM to be running around the clock; others order the machine on only at night. The degree of flexion and speed of the CPM are gradually increased, per the provider’s orders. This helps build the strength and mobility of the joint. (Be aware that some providers believe the CPM does not promote healing and may actually increase inflammation.)
Key Concept Do not force joint movement when doing PROM exercises. If the client complains of pain, stop and check with your supervisor
Active Range of Motion
The client doing individual self-directed exercises is performing active range of motion (AROM), although supervision may be necessary to ensure that the client moves all joints and muscles to the fullest extent possible.
Isometric (muscle-setting) exercises are those the client performs by tightening and releasing certain muscle groups. These exercises are helpful for strengthening the abdominal, gluteal, and quadriceps muscles, which are necessary for ambulation. Because these exercises only preserve muscle mass, they are not useful in preventing contractures. Therefore, isometrics are useful in preparing the client for crutch-walking or wheelchair use; maintaining muscle tone in a casted limb; or teaching bowel or bladder training. The routine that achieves the best results is a repetition of five sets of exercises, each lasting 5 seconds, with a 2-minute rest period between repetitions. (For example, tighten the abdominal muscles: count 1-1,000, 2-1,000, 3-1,000, 4-1,000, and 5-1,000. Rest for 2 minutes. Repeat until five sets have been completed.) The client’s thigh and leg muscles can be strengthened by contracting the quadriceps femoris, the large muscle on the anterior thigh; the client will feel as though he or she is pushing the popliteal space behind the knee downward into the mattress and pulling the foot forward.
Other exercises are done while sitting up in bed or in a wheelchair. The client lifts the hips by pushing the hands down into the mattress or the chair. For push-ups, the client lies face down with the hands placed flat on the mattress next to the shoulders, with the elbows bent. The client extends the elbows stiffly to raise the head and chest off the bed. Some daily activities can be turned into useful exercise (e.g., reaching for objects on the bedside table; pulling the overbed table forward and pushing it away; brushing the hair). Most clients confined to bed are given a trapeze, which hangs on a bar above the bed (see Fig. 49-6). The client uses it to pull up in bed, thus exercising the arms. Frequent use strengthens muscles, and the client often creates his or her own exercises when the importance of exercise is explained.
The physical therapist may introduce the exercises, but the activities are repeated several times a day, and nurses supervise them. Occupational therapy also provides muscle exercises, often for smaller muscle groups.