Learning Objectives
1. State at least three purposes for applying binders and bandages.
2. State the most common reasons for applying the roller bandage.
3. Explain how to judge the condition of the client’s extremity when it is wrapped in a bandage or has an antiembolism stocking applied.
4. Identify the most common use of the T-binder, addressing the differences when used for a male and a female client.
5. State the rationale for using Montgomery straps.
6. In the skills laboratory, demonstrate the ability to perform the following: applying roller bandages and antiembolism stockings, and changing a dressing using Montgomery straps.
|
IMPORTANT TERMINOLOGY |
|
|
antiembolism stockings |
Montgomery straps |
|
Kerlix |
peripheral neurovascular assessment |
|
maceration |
|
Acronyms |
|
|
ACE |
PNA |
|
CMS-ET |
SCD |
|
PCD |
TED |
When the client’s condition requires the application of bandages or binders, understanding the reasons for their use and performing correct, safe application techniques are important.
BANDAGES
Bandages and binders exist in a number of forms. They may be elasticized, such as the ACE wrap, or may be firmer.
Bandages and binders have many purposes and therapeutic benefits:
• Supporting a limb or joint
• Supporting a wound or incision
• Holding dressings in place
• Holding a pad to absorb drainage
• Holding a splint in place
• Holding a cold pack or warm pack in place
• Immobilization of a joint or limb
• Maintaining a limb in a specific position
• Providing compression, to promote venous return or prevent edema
• Providing compression, to prevent contractures, as in a burn
• To shape a stump before fitting a prosthesis
• Promoting venous return, as seen with venous insufficiency
Bandages and binders come in various widths and sizes. Some are rolled, to provide easy application. They may be clean or sterile. Table 53-1 provides some examples of various patterns that can be used when wrapping bandages.
Often, elasticized bandages are wrapped around a client’s limbs to provide muscle or joint support or to increase or support circulation. Gentle pressure against the tissues stimulates blood return to the heart and prevents blood from pooling in the extremity. Application that is too tight, however, can squeeze the blood vessels and nerves (constriction), resulting in tissue damage. It is vital to determine carefully and frequently the status of circulation and nerve function in the client’s fingers or toes to make sure that a bandage is not too tight.
The formal term for evaluating the status of an extremity encased in a bandage or a cast is peripheral neurovascular assessment (PNA). (See In Practice: Data Gathering in Nursing 53-1.) The final assessment is done by an RN, but the LPN/LVN assists in making and reporting observations. Some of the observations made in the distal part of the extremity are listed here. (The bandage or binder is between the distal portion of the extremity and the heart.)
• Skin color
• Finger or toe motion
• Sensation in fingers or toes
• Distal pulses
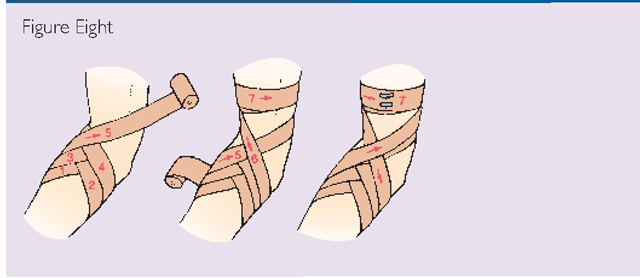
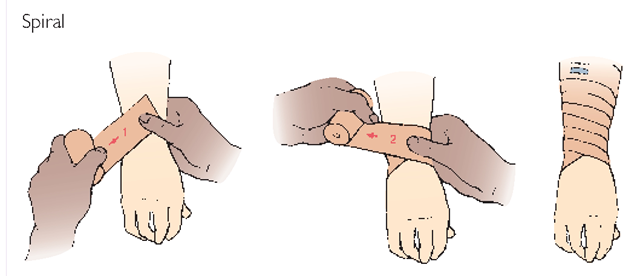
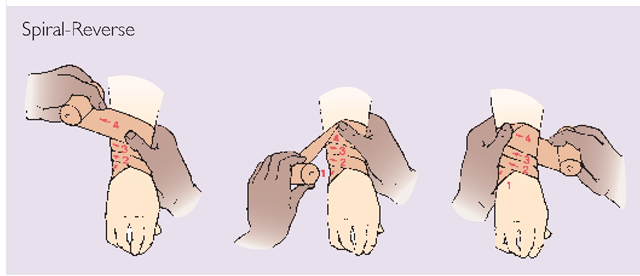
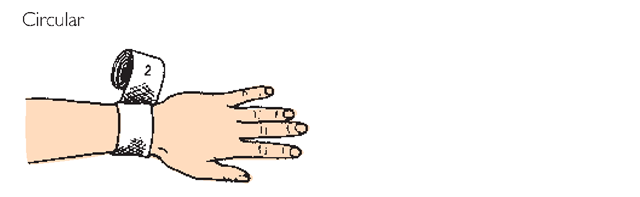
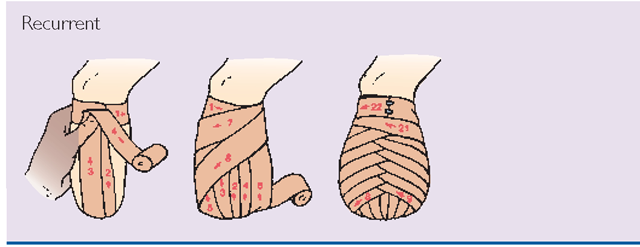
TABLE 53-1. Wrapping of Bandages
• Capillary refill
• Edema or swelling (see Fig. 47-10)
• Pain
• Severe pressure or tightness
• Skin temperature
When making these observations, note any abnormal findings and report them immediately. Often, a checklist is available on paper or in the computer to report frequent neurovascular assessments. Determine the protocol in your facility.
Wrapped bandages also can loosen easily, particularly if the client is mobile or restless. Loose bandages are not therapeutic. Just as you will check frequently to see if the bandage is too tight, you must also check to see if it is too loose.
IN PRACTICE :DATA GATHERING IN NURSING 53-1
THE CLIENT’S CIRCULATION WHEN USING BANDAGES (“CMS-ET”)
Color of Toes or Fingers
• The toes or fingers should be a color appropriate for the client’s normal skin tone. They should not be pale, white, dusky cyanotic, or mottled.
• Digits are checked by pressing them lightly Skin tone should return to normal immediately after the pressure is removed (capillary refill). If the area that was touched remains lighter the skin is blanched (indicating impaired circulation).
Motion or Mobility
• The client should be able to move the toes or fingers freely without pain.
Sensitivity or Sensation
• The client should be able to feel your touch on his or her toes or fingers. This should be equal on both sides.
• The client’s subjective feelings—tingling, numbness, or itching; pain (report and follow up); and any tightness (extreme tightness is a significant complication) should be discussed to obtain additional information.
• The client’s complaints of severe or excessive pain are significant.
Edema and Swelling
• When you press the client’s hand or foot, an indentation should not remain. An imprint indicates pitting edema. Nonpitting edema is also possible.
Temperature
• The temperature of the client’s toes or fingers should be warm and the same as the rest of his or her body The temperature should be the same on both sides.
NOTE: This assessment should be repeated at least every 2 hours (or more often, if necessary) for the client who has a cast, bandage, or binder in place.
CMS-ET, color, motion, sensitivity edema, temperature
NCLEX Alert You should be aware of the purposes and therapeutic benefits of bandages/binders, and how they relate to nursing care. Examples you study in this topic include the support of a limb/joint or a wound/incision, and holding a splint or warm/cold pack in place. Consider this as you select nursing actions in the NCLEX exam scenarios.
Roller Bandages
A commonly used bandage is an elastic roller bandage called the all cotton elastic (ACE) bandage (Fig. 53-1). (ACE is a brand name.) Although usually wrapped around a limb to give support, the ACE bandage may also be used to hold a dressing on an extremity or on the body’s trunk. In first aid, an ACE bandage may be wrapped around a body part to exert pressure over a bleeding point.
Kerlix
In other cases, a type of gauze with the brand name Kerlix is used to hold dressings in place or to apply pressure. Kerlix is a stretchy gauze in a long roll. The steps for applying an ACE- or Kerlix-type bandage are described in In Practice: Nursing Care Guidelines 53-1.
FIGURE 53-1 · Wrapping the all cotton elastic (ACE) roller bandage on the client’s arm. (A) Wrap the bandage around the client’s limb twice, below the joint, to anchor it. (B) Use alternating ascending and descending turns to form a figure eight. (C) Overlap each turn of the bandage by one-half to two-thirds the width of the strip. Fasten the end securely.
Stretch-Net Bandages
Another type of bandage, called Tube Gauze, is frequently used. It consists of a net or mesh-type material, which is very stretchy. These bandages come in assorted sizes,ranging from finger size to a size large enough to go around a person’s body. They are often used to hold a wound dressing in place and are frequently used in first aid and in burn care. This bandage is convenient and comfortable for the client. Tape is not always required to hold this bandage in place. This type of dressing is used frequently in the healthcare practitioner’s office or in the school or industrial setting, to dress a small wound or to hold a small dressing in place. In Practice: Nursing Care Guidelines 53 2 describes the steps used to apply this dressing.
IN PRACTICE :NURSING CARE GUIDELINES 53-1
APPLYING A ROLLER BANDAGE
• Wear gloves if the client has any non-intact skin or a rash. Rationale: It is important to protect yourself and others from the spread of infection.
• If the client does not have a dressing in place, it may not be necessary to wear gloves. Check with your team leader if you are unsure.
• Check your agency’s policy regarding orders for dressings and dressing changes. The primary healthcare provider’s order will indicate the specific part to wrap and how often. Rationale: The dressings will often be changed at the same time the bandage is rewrapped. It is important to follow the provider’s instructions because this is part of the treatment of the wound or the client disorder.
• In many cases, a roller bandage will be applied to give support to a body part (see Fig 53-1). In this case, a wound may or may not be present. Rationale: The basic wrapping of the roller bandage is the same, whether or not a wound dressing exists.
• Use the correct bandage size. The width of the bandage used is determined by the part to be wrapped. Generally a bandage wider than 7.5 cm (3 in) is difficult to keep in place on an arm or leg. Wider bandages may be used on the chest or abdomen. More than one roller bandage may be used, if necessary Simply overlap ends. Rationale: If a bandage is too narrow, it will pinch and bind. If a bandage is too wide, it will fold over. In either case, the effectiveness of the bandage will be compromised.
• Explain to the client what you plan to do. Rationale: Ensure the client’s cooperation.
• Elevate the extremity to be wrapped to just above the level of the client’s body if the client is recumbent. If the client is sitting, elevate to above the client’s heart level. Support the limb while wrapping. Rationale: Elevation helps to prevent congestion of the blood and lymph in the area to be wrapped.
• If the client has been sitting or walking and you are going to wrap a foot or leg, have the client lie down for at least 15 minutes before wrapping the bandage. Rationale: This time allows blood that may have pooled in the legs to be returned to the circulation. Otherwise, edema could interfere with the effectiveness of the bandage or cause damage to the limb.
• Roll the bandage before beginning to wrap. Rationale: This will help ensure that even pressure is applied and will add to the convenience when applying the bandage.
• Begin wrapping the bandage at the client’s toes or fingers and move toward the hip or shoulder Rationale: Wrapping upward enhances venous circulation.
• Wrap the bandage firmly but not too tightly Stretch the bandage very slightly while wrapping. Rationale: These precautions will help prevent the bandage from being wrapped too tightly and cutting off circulation.
• Overlap each layer about half the width of the previous strip. Do not allow any gaps between strips. Rationale: Overlapping ensures more even pressure.
• Keep the bandage free of wrinkles and folds. Rationale: If the bandage is wrinkled, this can quickly cause skin irritation and breakdown.
• Anchor the top with hypoallergenic tape or the attached Velcro strips. Rationale: Pins or clips may scratch the client.
• Check the circulation of the client’s toes or fingers after the bandage is in place. (See description of this procedure in Data Gathering in Nursing 53-1.) Rationale: A bandage that is too tight can cut off circulation and cause tissue damage. If it is too loose, it will not provide support.
• Dispose of any soiled dressings and your gloves in the prescribed manner. Wash or sanitize your hands. Rationale: Used dressings are grossly contaminated.
• Check the client’s peripheral neurovascular status at least every 2 hours. Rewrap the bandage, if necessary. Rationale: A bandage that is too tight can cause damage very quickly. One that is too loose will not accomplish its purpose.
• Document the procedure, noting the client’s reactions. Rationale: Documentation provides communication and ensures continuity of care.
• Release the bandage at least once every 4 hours, unless ordered otherwise. At this time, help the client exercise the leg or arm and give skin care. Rationale: Releasing the bandage allows for skin inspection under the area that is bandaged; exercise and skin care increase circulation and help to prevent deformities and discomfort.
The larger sizes of stretch-net dressings cover an arm or leg and are applied in a manner similar to the procedure outlined for dressing a finger. They are simply stretched and placed over the extremity. The body-size stretch-net is stretched out and moved over the head and arms, to get it in place over the torso.
Nursing Alert When applying a large stretch-net bandage to the torso, be sure to tell the client beforehand that the netting will be moved over the head in order to place it around the body This will help to alleviate apprehension about the process.