PREPARATIONS
Injectable medications are packaged in many ways. Some are supplied as powders that must be reconstituted with a diluent. When mixed with a diluent, these medications are often fairly unstable and may deteriorate rapidly. They must be used within the time specified by the manufacturer. Common diluents include sterile water and sterile normal saline. The manufacturer’s instructions will specify the diluent and the amount to be used. In other cases, both the diluent and the powder are supplied by the manufacturer. Follow the specific instructions for mixing any of these solutions.
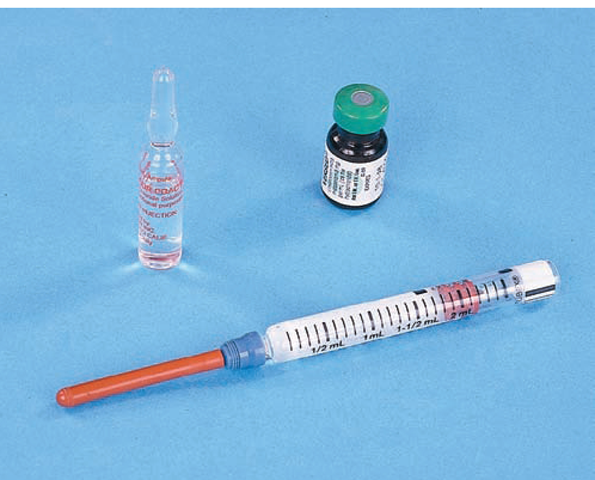
Many parenteral medications are premixed by the manufacturer. Medications for injection may be supplied in a single-dose ampule, single-dose or multidose vial, or prefilled syringe (Fig. 64-6). An ampule is a glass container that holds a premeasured, single medication dose.
Key Concept Discard any unused portion of an ampule’s contents, because no way exists to prevent contamination of an open ampule.
A vial is a glass container equipped with a self-sealing rubber stopper. It may contain a single premeasured medication dose, or may be a multidose vial. When drawing up any injection, use strict aseptic technique, to prevent contamination. Label all multidose vials with the time, date, and initials detailing first use. (Some medications require refrigeration before and/or after being opened.) In Practice: Nursing Procedure 64-1 describes how to draw up medication from an ampule and from a vial.
A prefilled syringe, for example Tubex or Carpuject, provides a single medication dose prepared by a manufacturer or pharmacy. If the entire amount of medication is not needed, discard the excess amount into the designated receptacle before administration. This is done by pushing the plunger until the correct quantity is obtained. Remember, if the medication is a controlled substance, another licensed nurse must witness this procedure and document it in the designated manner. In many cases, prefilled syringes do not have safety needle covers. Therefore, other measures must be taken to prevent accidental needle sticks (see Fig. 64-4B).
FIGURE 64-6 · Examples of an ampule, vial, and prefilled medication cartridge.
Key Concept Remember: Medications and their packaging cannot be disposed of in the community sewer system. Packages from oral, rectal, eye, ear, transdermal medications, and so on are placed in the hazardous waste container All vials, ampules, needles, syringes, and prefilled syringes are to be disposed of in the sharps container
INTRADERMAL INJECTIONS
Intradermal injections, often used for diagnostic testing (“skin tests”), are shallow injections given just beneath the epidermis. The inner aspect of the forearm is the common injection site. If a number of substances are to be tested, the back may be used. Tuberculin syringes, which identify hundredths of a milliliter and can hold a total of 1 mL, are commonly used. Because the tuberculin syringe has a very small diameter, it can be graduated in hundredths and tenths of a milliliter for accurate measurement of very small amounts of medication (In Practice: Nursing Procedure 64-2 and Fig. 84-1).
Key Concept If administering an intradermal injection, instruct the client not to scratch or pinch the site. Rationale: This could irritate the area and alter the results of the test. This could also cause the injected material to be absorbed systemically.
SUBCUTANEOUS (SC, SubQ) INJECTIONS
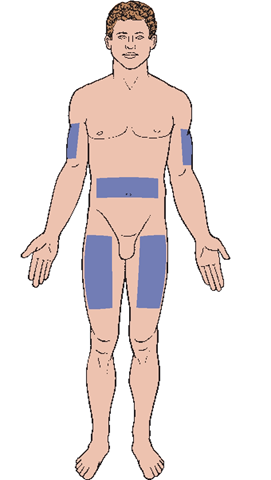
Subcutaneous injections are administered into subcutaneous or adipose (fatty) tissues located below the dermis (Fig. 64-7; see also Fig. 64-5). This method is used for small amounts of medication that require slow, systemic absorption. Generally, the duration of SC medications is longer than that of other parenteral medications. Many medications cannot be given by the subcutaneous route. If the volume of medication is greater than 1 mL, the subcutaneous route is usually not recommended or two sites must be used.
Subcutaneous medications must be soluble and of sufficient strength to be effective, yet safe for surrounding tissues. Common SC medications are insulin and heparin. Allergy injections and some pain medications may be administered SC as well. Subcutaneous injections are given in areas where bones and blood vessels are not near the skin’s surface. One common site is the outer aspect of the upper arm, above the halfway mark between the elbow and the shoulder.
FIGURE 64-7 · Subcutaneous injection sites. Less commonly, sites on the back are used.
There are a number of commonalities between the administration of SC and IM injections. The major difference is the choice of the site, the needle used, and the angle at which the needle is inserted. In Practice: Nursing Procedure 64-3 explains the steps in administering a subcutaneous or intramuscular injection, and In Practice: Nursing Care Guidelines 64-1 offers specific considerations for subcutaneous injections.
Key Concept Always rotate injection sites for clients who receive injections on a regular basis.
INTRAMUSCULAR (IM) INJECTIONS
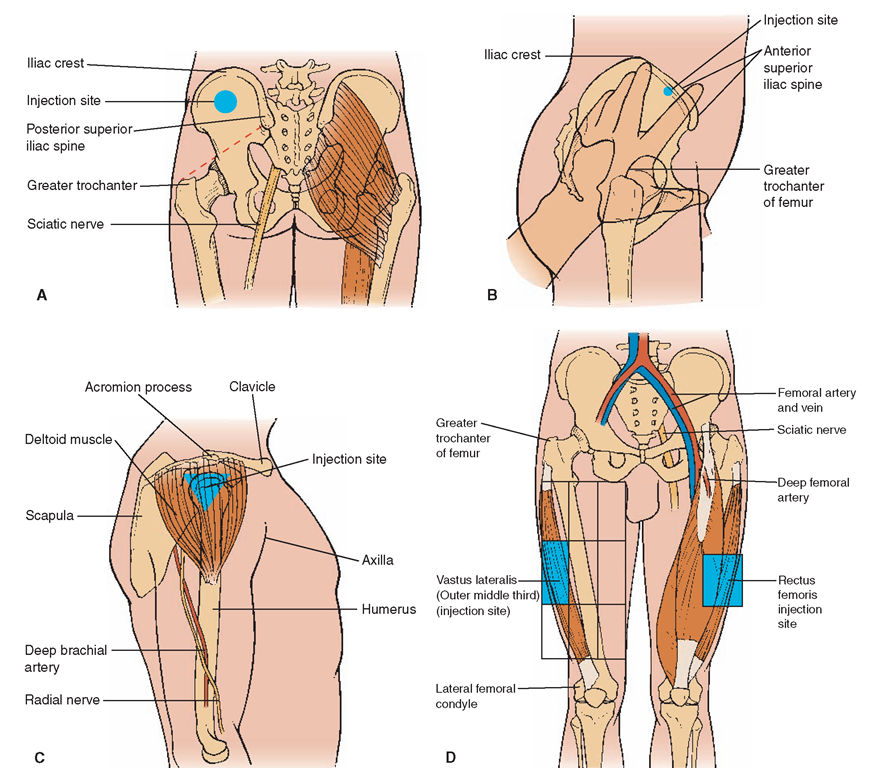
Intramuscular injections are given in muscles situated below the dermal and subcutaneous skin layers. Such medications must be injected deep into muscles. The body absorbs IM injections much more rapidly than SC injections, because of the greater amount of blood supply to muscle tissue. It is important for the nurse to be thoroughly familiar with IM injection sites and the technique for administering these injections. The most common areas for IM administration are the following (Fig. 64-8):
• Dorsogluteal (back of hip)
• Ventrogluteal (side of hip)
• Deltoid (upper arm)
• Vastus lateralis (side of thigh)
• Rectus femoris (anterior thigh), used only when other sites are not available
IN PRACTICE: NURSING CARE GUIDELINES 64-1
GIVING A SUBCUTANEOUS INJECTION
• The most common method of giving a subcutaneous (SC) injection is to bunch the skin at the subcutaneous site. Rationale: Usually, bunching the skin will ensure that the injection is made into the subcutaneous tissue and not the muscle beneath. Spreading the skin would not allow sufficient subcutaneous tissue to prevent intramuscular injection.
• Assess the client for body mass of subcutaneous tissue and choose the appropriate needle and angle of injection. The angle of injection varies with the amount of available tissue (Fig. 64-7). Most subcutaneous injections are given at a 90-degree angle. However; a thin client may need to be injected at an angle of a lesser degree (as small as 45 degrees). Rationale: It is important to choose an injection angle that will ensure the medication is delivered into the subcutaneous tissue and not the muscle.
Injecting the medication.
• The amount of the client’s adipose tissue also determines the length of needle to use (generally between % and 1 inch). Rationale: It is important to have a needle that is short enough to just reach the subcutaneous tissue and not extend into muscle.
• Take care not to inject the medication too closely to the skin’s surface. Rationale: Doing so will allow for faster absorption and onset of action of the medication and may cause local irritation. (This might actually be an intradermal injection if it is very shallow.)
• Injection at the correct angle is important. Rationale: The usual rule is 45 degrees for a /8-inch needle or 90 degrees for a /2-inch needle. Check the agency’s policy.
• Indicate that the medication was administered subcutaneously If the client is to receive repeated injections, identify the exact site used. Rationale: Documentation provides coordination of care. Site rotation prevents injury to subcutaneous tissue.
• Check the client’s response to the medication within an appropriate period. Rationale: Drugs administered parenterally have a rapid onset.
• Dispose of syringe and needle in the sharps container.
Intramuscular injection is the best technique when medications given less deeply irritate the client’s tissues or when large amounts of medication are necessary. These injections are given in much the same way as subcutaneous injections. However, a longer needle with a larger bore is used, most often a IV2- to 2-inch, 20- to 22-G needle, depending on the type of medication. Use an angle of 90 degrees for the injection (see Fig. 64-5; see also In Practice: Nursing Procedure 64-3). In addition to requiring a longer and larger-gauge needle, IM injections are more difficult and dangerous than SC injections. The needle must be injected deeper into the client’s body, penetrating the epidermal, dermal, subcutaneous, and muscle tissues. If the medication is thick, injecting into the muscle may be more difficult (In Practice: Nursing Procedure 64-4).
FIGURE 64-8 · Intramuscular injection sites. (A) Dorsogluteal (posterior view): lateral, slightly superior to midpoint of line drawn from trochanter to posterior superior iliac spine. (B) Ventrogluteal (side view): palm placed on greater trochanter and index finger toward anterior superior iliac spine; middle finger spread posteriorly away from index finger as far as possible; injection site is in middle of triangle. (C) Deltoid (side view): lower edge of acromion process palpated; at midpoint, in line with axilla on lateral aspect of upper arm, triangle is formed. (Deltoid site not used for children younger than 4 years.) (D) Vastus lateralis: divide thigh into thirds, horizontally and vertically. Give injection in outer middle third. (Vastus lateralis site used in infants and toddlers as well as adults.) The rectus femoris site is on the anterior aspect of the thigh, approximately one-third of the way between knee and hip. This site is uncomfortable and not commonly used.
Nursing Alert When administering IM and SC injections, insert and remove the needle quickly (unlike the intradermal injection).
Dorsogluteal Site
The dorsogluteal area is a common IM injection site (see Fig. 64-8A). To use the dorsogluteal site, assist the client to a side-lying or prone position. If the client is on the side, instruct him or her to bend the knees. If on the stomach,instruct the client to point the toes inward. Rationale: This positioning aids in relaxation of the gluteal muscles, making the injection more comfortable.
Key Concept Do not administer an intramuscular injection with the client standing. Explain to the client who is reluctant to lie down that this will be the safest and most comfortable position. Rationale: Clear identification of the area is difficult, and the muscles will be tenser while standing. In addition, the client may experience a vasovagal reaction and faint, sustaining injury as he or she falls.
Nursing Alert It is very important to select the dorsogluteal site carefully. Rationale: This site is very close to the sciatic nerve. Hitting this nerve can cause permanent damage. Do not use this site for infants and children younger than 3 years. Rationale: Their muscles in this area are not yet developed and are not of sufficient mass.
Ventrogluteal Site
The preferred site for injection in the hip area is the ventrogluteal site (see Fig. 64-8B). This site can be used if the client is in the side-lying, prone, or supine position. The ventrogluteal site is safer and less painful for IM injections than the dorsogluteal site, through which the sciatic nerve runs. The fat layer is thinner in the ventrogluteal area, and the gluteal muscle is thicker, even in very thin clients. One disadvantage of the ventrogluteal site is that the client may never have received an IM injection in this area, which may cause anxiety. Another disadvantage is that the client can see what the nurse is doing, which may also increase anxiety. The client will be most comfortable in a side-lying position.
Deltoid Site
Although the deltoid muscle may be used for IM injections, it is large enough only for small amounts of medication. In most cases, 1 mL is the maximum amount of medication that can safely be given in this site. A risk of brachial artery and radial nerve damage exists with this site. Use this route in children only if they are older than 4 and only if the medication to be administered is not irritating to the tissues, the volume is very small, and the medication will be absorbed quickly. This site is not used for infants and toddlers. The deltoid muscle is located on the lateral aspect of the upper arm, 1 to 2 inches below the acromion process (see Fig. 64-8C). Identify the injection site by placing the index and middle fingers over the acromion process. The injection site is 11⁄2 to 2 inches below the middle finger. Hepatitis B vaccine and tetanus toxoid are examples of medications often given in the deltoid muscle.
Vastus Lateralis Site
The vastus lateralis is a thick muscle located on the anterior, lateral area of the thigh. This muscle may be used for IM injections in infants and children younger than 3 years because it is the largest muscle mass in this age group. Little risk of injury exists with this site because no large nerves or arteries surround the area. Locate this site by placing the palm of one hand over the greater trochanter and the palm of the other hand over the knee; identify the injection site anteriorly and laterally, halfway between these two points (see Fig. 64-8D).
Rectus Femoris Site
The rectus femoris muscle lies medially to the vastus lateralis.Identify the injection site in the same manner as that for the vastus lateralis (see Fig. 64-8D). This site is often used for infants and toddlers. Many adult clients find the rectus femoris site uncomfortable; it is often used in adults only when other sites are contraindicated. Rationale: Disadvantages of this site are that the sciatic nerve and numerous blood vessels run very close to it. Should contact with the sciatic nerve be made while administering the injection, nerve damage—resulting in permanent damage or paralysis—may occur. Table 64-1 presents further guidelines for site selection.
Nursing Alert IM injections must be given into healthy muscle tissue for proper absorption to occur. If a client requires frequent IM injections, rotate the sites and note on the client’s medical administration record (MAR) or a “site rotation map,” which site was used each time.
Rotating insulin injection sites is particularly important because insulin can atrophy tissue (lipodystrophy) with repeated injection in the same site.