Positron Emission Tomography
Positron emission tomography (PET) scanning involves injecting a solution containing molecules labeled with an unstable radionuclide into the blood circulation. The excess protons in the unstable radionuclide are converted into neutrons by radioactive decay. During this conversion, a positron (a positively charged electron) is emitted. The positron collides with an electron, releasing two photons that are sensed by detectors placed around the head. Usually blood flow in the brain is monitored by injecting oxygen 15 (15O)-labeled water, and glucose utilization is assessed by injecting fluorine-18-labeled 2-de-oxyglucose. When a particular brain region is activated by a given task (e.g., visual stimulation), neuronal activity, blood flow, and glucose utilization are increased in that region. A common radionuclide used for localization of a seizure focus in patients with epilepsy is 18F-deoxyglu-cose. This radiolabeled substance displaces glucose. As the unstable isotope decays, a positron is generated that collides with an electron. This collision destroys both particles, and two gamma rays are emitted, which are then detected using special detectors. The areas of positron-electron collisions, representing the areas of high metabolic activity, can be imaged in this manner. It should be noted that PET scans taken in situations in which the patient is hyperactive or shivering can give false-positive readings. Therefore, hyperactivity and shivering are controlled before the PET scanning procedure is carried out on the patient. This procedure is also used for detecting brain neoplasms because malignant cells have a relatively high glucose uptake.
Single-Photon Emission Computed Tomography
Single-photon emission computed tomography (SPECT) is less expensive and less complex than a PET scan. Gamma camera technology is used to determine regional cerebral blood flow after the injection of a specific radio-nuclide, such as hexamethyl-propyleneamineoxime. SPECT is useful as an adjunct to diagnosis in many neurologic conditions in which there may be defects or alterations in blood flow to specific regions of the brain such as a stroke.
Angiography (Arteriography)
Angiography usually involves introduction of a specially designed catheter into a femoral artery. The catheter is then advanced under fluoroscopic guidance until it reaches the aortic arch. The tip of the catheter is then steered towards the origin of the vessel under investigation (e.g., the internal carotid or vertebral artery). A radiopaque contrast material (e.g., an iodinated dye) is then injected via the catheter, and x-ray pictures are taken in rapid sequence as the contrast material flows through the artery (arterial phase), capillaries (capillary phase), and veins (venous phase). Photographic techniques are then used to visualize the blood vessels. Injection of the contrast material is contraindicated in patients who are allergic to the contrast-enhancing agents. Usually the contrast of the x-ray image prepared before the injection of the contrast material is reversed by making a positive image in which bones appear dark. The reverse-contrast image is superimposed on the x-ray image prepared after the injection of the contrast material. A print is then made of the two images together. More commonly, the x-ray images are processed digitally for clear visualization of blood vessels.
Angiography is used to identify structural abnormalities of vessels (e.g., stenosis [narrowing], occlusion, malformations, and aneurysms), displacement of the normal position of the cranial vessels, and changes in flow patterns (e.g., occlusion of a major vessel by a thrombus may promote collateral flow in a smaller branch).
Angiography is an invasive procedure and may cause stroke in some patients. Moreover, bleeding may occur sometimes at the arterial puncture site. Occasionally, occlusion of the femoral artery may develop at the puncture site, which may cause ischemia in the leg. Therefore, the arterial puncture site is carefully examined and observed for at least 24 hours after the procedure is completed. As mentioned earlier, in view of the invasive nature of conventional angiography, usually noninvasive procedures, such as MRA or CT scanning, are used first for visualization of intracranial blood vessels. However, blood vessels are not imaged clearly in ordinary CT scans because the x-ray density of blood and CNS is similar. Therefore, a contrast material is usually injected intravenously before CT scanning to allow clear visualization of blood vessels. Computer processing of CT scans allows three-dimensional reconstruction of arteries and veins.
Vascular Syndromes
The areas supplied by the most commonly affected arteries and the deficits after their occlusion are described in the following sections.
Cerebral Vascular Syndromes
The cerebral cortex is supplied by the following arteries.
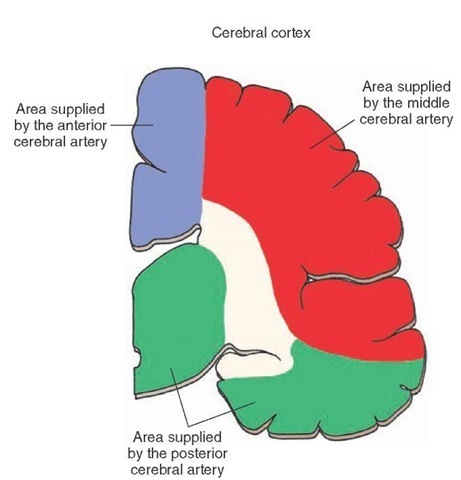
The anterior cerebral artery: This artery and its branches supply blood to the medial and dorsal aspect of the frontal and parietal lobes of the cerebral hemisphere, including the postcentral gyrus (which is concerned with the processing of sensory information from the contralat-eral leg) and precentral gyrus (from which motor control of the contralateral leg originates). The regions of the cerebral cortex supplied by the anterior cerebral artery are shown in Figure 27-7 (see also Fig. 4-2).
FIGURE 27-7 The coronal section through cortex showing the territories supplied by the anterior cerebral (blue), middle cerebral (red), and posterior cerebral (green) arteries.
The middle cerebral artery: This artery and its branches supply blood to the precentral gyrus (primary motor area), premotor region, the somesthetic and auditory areas, and the integrative association areas of the parietal lobe. The cerebral cortical areas supplied by the middle cerebral artery are shown in Figure 27-7 (see also Fig. 4-3).
The posterior cerebral artery: This artery supplies most of the midbrain and thalamus as well as the subtha-lamic nucleus (Fig. 27-7; see also Fig. 4-4). After this artery passes around the midbrain, three major branches arising from it (i.e., anterior and posterior temporal and parieto-occipital branches) supply the temporal and inferior occipital lobes of the cortex (Fig. 4-4). A branch of the posterior cerebral artery, called the calcarine artery (Fig. 4-4), supplies the primary visual cortex.
The following syndromes are caused by the interruption of the blood flow in the above-mentioned arteries.
Anterior Cerebral Artery Syndrome
Anterior cerebral artery syndrome is caused by interruption of blood flow in the trunk of one of the anterior cerebral arteries, which damages the precentral gyrus and results in contralateral paralysis (contralateral hemiplegia), mainly of the leg. Occlusion of both anterior cerebral arteries produces bilateral paralysis, which is pronounced in the lower limbs. Ischemic damage to the postcentral gyrus results in impaired sensation, mainly to the leg.
Middle Cerebral Artery Syndrome
Middle cerebral artery syndrome is caused by occlusion of the main trunk of this artery, which results in contralateral hemiplegia predominantly in the upper extremities and face because the upper limb region is represented in a l ateral position of the precentral gyrus.If the left hemisphere is involved, aphasia (disturbances in speech) may occur because the speech centers are located laterally in this hemisphere.
Posterior Cerebral Artery Syndrome
Posterior cerebral artery syndrome is caused by interruption of the calcarine branch of the posterior cerebral artery, which supplies both the upper and lower banks of the visual cortex, which results in hemianopsia (see Figs. 4-4 and 16-10). CT scans taken 6 and 48 hours after the onset of a right homonymous hemianopsia, due to the embolization of the left posterior cerebral artery, are shown in Figure 27-2, A and B, respectively. A subtle loss of gray-white contrast and marked hypodensity of gray and white matter in the infarcted left visual cortex are visible after 6 and 48 hours of the onset of hemianopsia, respectively. Other symptoms are described below under "Weber’s Syndrome."
Midbrain Vascular Syndromes
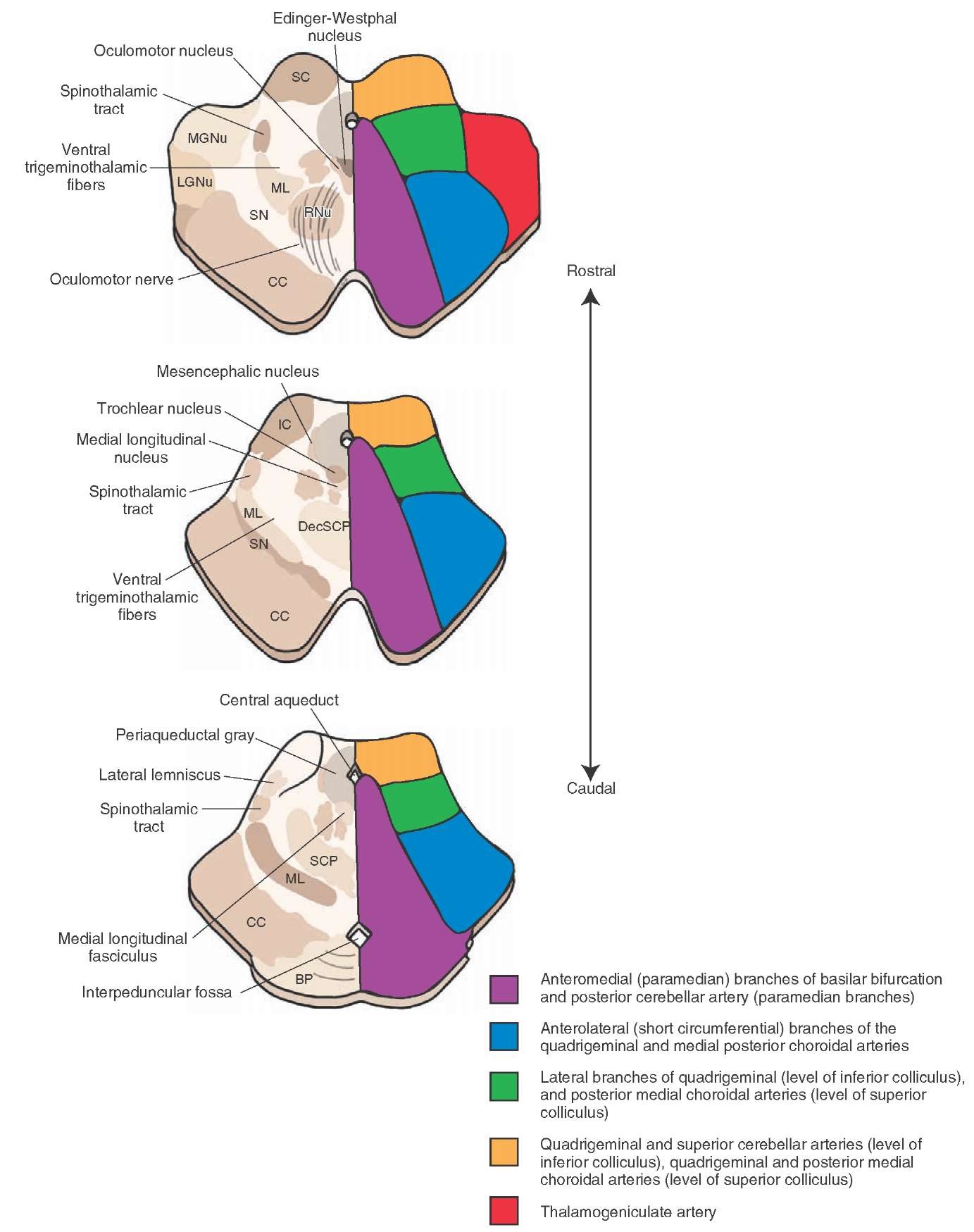
Arterial supply of different regions in the midbrain is schematically shown in Figure 27-8. The posterior cerebral arteries arise at the terminal bifurcation of the basilar artery (See Fig. 4-1). Occlusion of branches of the posterior cerebral arteries that supply the midbrain results in the following midbrain vascular syndromes.
FIGURE 27-8 Arterial supply of the midbrain (schematic representation). Important structures are shown on the left and the pattern of arterial blood supply is shown on the right side of each diagram. BP = basilar pons; CC = crus cerebri; DecSCP = decussation of the superior cerebellar peduncle; IC = inferior colliculus; LGNu = Lateral geniculate nucleus; MGNu = Medial geniculate nucleus; ML = medial lemniscus; RNu = Red nucleus; SC = superior colliculus; SN = substantia nigra.
Weber’s Syndrome
Weber’s syndrome is also called medial midbrain syndrome and results from occlusion of paramedian branches of the posterior cerebral artery causing unilateral damage to the ventral region of the midbrain. It is characterized by ipsilateral paresis of adduction and vertical gaze, pupillary dilation (due to damage to the oculomotor nerve), and paresis of the contral-ateral face, arm, and leg (due to damage to the corticospinal and corticobulbar tracts.
Claude’s Syndrome
Unilateral damage to the tegmental region of the midbrain causes Claude’s syndrome. It is characterized by ipsilateral oculomotor paresis (due to damage to the oculomotor nucleus) and contralateral ataxia and tremor (due to damage to the superior cerebellar peduncle).
Parinaud’s Syndrome
Parinaud’s syndrome is also called gaze palsy syndrome, sylvian aqueduct syndrome and midbrain syndrome. Dorsal midbrain lesions cause this syndrome, which is characterized by impaired upward vertical gaze and loss of the pupillary light reflex (due to damage to the pretectal area.
Benedikt’s Syndrome
Benedikt’s syndrome is caused by combined lesions of the ventral and tegmental midbrain. It is characterized by oculomotor paresis (due to damage to the rootlets of the oculomotor nerve), ataxia, and weakness (due to damage to the region of the red nucleus and superior cer-ebellar peduncle.
The superior cerebellar artery arises just caudal to the bifurcation of the basilar artery (see Fig. 4-1). This artery supplies the rostral pons, caudal midbrain, and the superior surface of the cerebellum (Fig. 27-8). Occlusion of this artery results in the following midbrain syndrome.
Superior Cerebellar Artery Syndrome
Symptoms of superior cerebellar artery syndrome include: (1) analgesia and thermoanesthesia on the ipsilateral side of the face due to damage to the nucleus and spinal tract of the trigeminal nerve; (2) ipsilateral Horner’s syndrome, which is characterized by a triad of symptoms, including constriction of the ipsilateral pupil, drooping of the upper eye lid, and sinking in of the eyeball (in this syndrome, there is a disruption of the descending sympathetic pathways that supply the eye, resulting in unopposed parasympathetic effects on the eye); (3) contralateral loss of sensations of pain and temperature due to damage to the spinothalamic tract; and (4) ipsilateral limb and gait ataxia due to damage to the superior cerebellar peduncle and adjoining cerebellar efferents, respectively.
Pontine Vascular Syndromes
The arterial supply of different regions of the pons is shown in Figure 27-9. The arteries supplying the pons include paramedian and long circumferential branches of the basilar artery and branches of anterior inferior and superior cerebellar arteries (see Fig. 4-1). The pontine paramedian arteries arise from the basilar artery and supply the medial portion of the caudal and rostral pons. The short circumferential arteries supply a wedge-shaped area in the ventrolateral pons. The long circumferential arteries supply most of the tegmentum of the rostral and caudal pons and lateral portions of the mid-brain tegmentum. The anterior inferior cerebellar artery (AICA) supplies the ventral surface of the cerebellum and lateral portions of the caudal pons. Occlusion of different arteries supplying the pons elicits the following syndromes.