Descending Motor Systems From The Brainstem
There are six descending fiber pathways from the brain-stem to the spinal cord that are of importance: the medial and lateral reticulospinal tracts, the medial and lateral ves-tibulospinal tracts, the rubrospinal tract, and the tectos-pinal tract. The reticulospinal and vestibulospinal tracts innervate neurons of the ventral horn that are associated with the axial musculature, whereas rubrospinal (similar to corticospinal) fibers supply mainly the neurons that innervate the distal flexor musculature.
Reticulospinal Tracts
There are two reticulospinal tracts; one arises from the medulla (the lateral reticulospinal tract), and the other arises from the pons (medial reticulospinal tract) (see Fig. 9-15). The medial reticulospinal tract arises from large cells located in the medial part of the reticular formation (called the nucleus reticularis pontis oralis and nucleus reticularis pontis caudalis) and descends to all levels of the spinal cord where it synapses either directly upon both alpha and gamma motor neurons or indirectly through interneurons. The primary motor function is to facilitate voluntary or cortically induced movements and to increase muscle tone because of its actions on gamma motor neurons. The lateral reticulospinal tract arises from cells called the nucleus reticularis gigantocellularis and other large (magnocellular) neurons located in the medial two thirds of the medulla. Axons of these cells descend to all levels of the spinal cord. The actions of this pathway are opposite to those of the medial reticulospinal tract. Activation of this pathway inhibits voluntary movements and cortically induced movements and reduces muscle tone by further inhibiting muscle spindle activity through its effects on gamma motor neurons.
Vestibulospinal Tracts
There are two vestibulospinal tracts. One arises from the medial vestibular nucleus, and the other arises from the lateral vestibular nucleus (see Fig. 9-14), and both convey impulses to the spinal cord from the labyrinth. The medial vestibulospinal tract arises from the medial vestibular nucleus and projects as the descending component of the medial longitudinal fasciculus to reach cervical levels of the spinal cord bilaterally. The importance of these fibers is that they activate lower motor neurons associated with the spinal accessory nerve. In this manner, activation of the medial vestibulospinal tract can cause rotation and lifting of the head as well as rotation of the shoulder blade around its axis. Such movements are important in producing an appropriate orientation of the individual in response to forces that cause changes in posture and balance. The lateral vestibulospinal tract arises from the lateral vestibu-lar nucleus and projects to all levels of the spinal cord. Stimulation of this pathway powerfully facilitates alpha and gamma motor neurons that innervate extensor motor neurons. Similar to the medial vestibulospinal tract, the lateral vestibulospinal tract also plays an important role in the maintenance of posture by exciting neurons that innervate extensor (i.e., antigravity) muscles, mainly of the lower limbs. The lateral vestibulospinal tract is modulated by activation of the vestibular apparatus or cerebellum, which provides it with its major afferent supply.
Rubrospinal Tract
The rubrospinal tract arises from the red nucleus. As soon as the axons emerge from the red nucleus, they cross over to the contralateral side in the ventral tegmental decussa-tion and descend to the spinal cord (see Fig. 9-13). In less advanced animals, such as the cat, the fibers have been shown to descend to both cervical and lumbar levels. However, in higher forms, the primary projection to the spinal cord is directed to cervical levels. Thus, in humans, the primary action of the rubrospinal tract is to facilitate motor neurons that innervate flexor muscles. As noted earlier, the red nucleus receives major inputs from the primary and premotor cortices, and the entire pathway from the cortex to the spinal cord is somatotopically organized. In this manner, this system may be referred to as a cortico-rubro-rubrospinal pathway. This pathway may thus be thought of as a functionally parallel system to that of the corticospinal tract. The reasons for this conclusion are that: (1) both systems originate from the same general regions of cortex, (2) both systems are somatotopically organized, and (3) both systems act primarily on the flexor motor system. In particular, by innervating flexor muscles of the upper extremity, both corticospinal and rubrospinal neurons excite muscles that act against gravity (in humans) and that are involved in the fine control of movement.
It should also be noted that, in humans, where the overall size of the rubrospinal tract is diminished, there is an increase in the size of the descending projections of the red nucleus to the cerebellum via the inferior olivary nucleus (i.e., rubro-olivary fibers), suggesting the presence of a more potent influence of the red nucleus on cerebellar function in primates.
Tectospinal Tract
The tectospinal tract arises from the superior colliculus of the midbrain and soon crosses over to the contralateral side in the dorsal tegmental decussation. The fibers descend to cervical levels of the spinal cord where they terminate (see Fig. 9-13). Although little is known about the functions of this tract, it is believed that it serves to produce postural changes in response to visual stimuli that reach the superior colliculus.
The Upper Motor Neuron Syndrome
This syndrome is the result of disruption of central motor pathways that arise from the cerebral cortex. The lesion may occur in the cortex, internal capsule, crus cerebri, lower medulla, or even lateral funiculus of the spinal cord. Typically, however, the most common sites of damage include the internal capsule and cerebral cortex. It should be pointed out that the upper motor neuron syndrome likely reflects damage not only to corticospinal neurons, but also to other descending fibers from the cortex to the brainstem, which synapse upon descending pathways to the spinal cord. Examples of such connections include cortical projections to the reticular formation (i.e., to reticulospinal neurons) and the red nucleus (i.e., rubrospinal neurons). In fact, these connections help to account for some of the clinical signs characteristic of the upper motor neuron syndrome. Thus, it may be concluded that, while all corticospinal neurons are upper motor neurons, not all upper motor neurons are cor-ticospinal neurons.
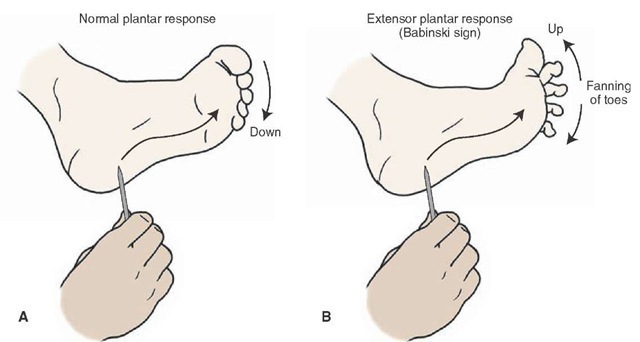
The most classic signs of upper motor neuron syndrome include: (1) paralysis or weakness (paresis) of movement of the affected muscles; (2) a marked increase in muscle tone (hypertonia) coupled with spasticity (i.e., resistance to movement in a single direction); (3) the presence of abnormal reflexes, such as the Babinski sign (i.e., extension and fanning out of the big toe; also referred to as an extensor plantar response), after stroking along the sole of the foot with a sharp object (Fig. 19-9); and (4) the diminution of some reflexes such as the abdominal reflexes. However, immediately after damage (usually from a stroke) to the cerebral cortex or internal capsule, a flaccid paralysis of the contralateral limb appears with hypotonia and loss of myotatic reflexes. Nevertheless, the condition reverses after a period of time, and the hypotonia is replaced by hypertonia. The myotatic reflexes reappear and are highly pronounced (i.e., hyperreflexia), with continued loss of function of the distal musculature.
FIGURE 19-9 Illustration of a Babinski test. The sole of the foot is stroked with a sharp object from front to back. This kind of stimulation typically produces flexion of the foot (A). However, a patient who has an upper motor neuron paralysis will show extension of the large toe coupled with a fanning out of the other toes (B).
There are several aspects to upper motor neuron syndrome. The paralysis of movement of the distal musculature can easily enough be accounted for in terms of our understanding of the anatomical relationships between the upper and lower motor neurons. Specifically, the sequencing of discharge patterns of different groups of ventral horn cells at a given time for a purposeful movement to occur requires command signals from corticospinal fibers. The loss of such input to the ventral horn of the spinal cord would obviously prevent those neurons from discharging in a meaningful sequence. Hence, such a loss would result in paralysis of movement.
The second feature of this disorder is spasticity and hyper-tonia, which is still poorly understood. Several hypotheses have been advanced to attempt to account for this phenomenon. One logical possibility is that corticospinal fibers make contact with both interneurons that excite motor horn cells as well as several types of inhibitory interneu-rons. One type of inhibitory interneuron is a Renshaw cell. When stimulated, this neuron produces recurrent inhibition of motor neurons innervating a specific muscle group. A second type might include an inhibitory interneu-ron that receives inputs from a 1b sensory fiber and which makes synapse with a homonymous motor neuron. A third type of inhibitory interneuron is one which receives input from a 1a sensory afferent fiber and which makes synaptic contact with a motor neuron that supplies the antagonistic muscle. The loss of input to these inhibitory interneurons could result in increased levels of excitability of neurons that innervate antagonists, such as extensor groups of the lower limbs and flexors of the upper limbs. The difficulty with this hypothesis is that "pure" pyramidal tract lesions of restricted regions of area 4 or at the level of the lower brainstem, which only destroy corticospinal tract fibers, do not necessarily produce spasticity. In fact, when such experimental lesions were carried out in monkeys, the resulting effect was described as a hypotonia.
An alternative interpretation for the presence of spas-ticity is that lesions of the internal capsule or cerebral cortex destroy not only corticospinal fibers, but also corti-cobulbar fibers. One such group of fibers of significance is the corticoreticular fibers that innervate neurons that give rise to the reticulospinal tracts. It is known that the medullary reticulospinal fibers powerfully inhibit spinal reflexes and, in particular, the actions of the gamma motor system. In contrast, the pontine reticulospinal system is facilitatory to spinal reflexes and the gamma motor system. This hypothesis proposes that the medullary reticu-lospinal neurons require cortical inputs to discharge, while those reticulospinal neurons located in the pons receive other kinds of afferent fibers and have less of a requirement for cortical inputs in order for them to discharge. Therefore, after damage to the cerebral cortex or internal capsule, there is a loss of inhibitory input to the spinal cord from the medullary reticular formation, whereas the excitatory regions of the pontine reticular formation continue to affect spinal motor neurons. Such a condition would result in an imbalance between excitatory and inhibitory influences upon spinal motor neurons from the reticular formation, in which case, the excitatory inputs remain largely intact. Since the reticular formation acts to a great extent on the gamma motor system, the resulting changes would cause spasticity.
Clinical Case
History
Jane, a 75-year-old secretary who still works for an academic physician, has a history of hypertension but was doing relatively well until she received an important phone call that relayed news regarding a poor score on a National Institutes of Health grant application submitted by her boss. Her boss grabbed the telephone from her after noting that she suddenly developed weakness in her right arm, leg,and face and that she was slurring her speech on the telephone. She needed to be helped by some of the ancillary staff to the emergency room (ER) because she continually fell to the right.
Examination
The physician who saw her in the ER noted that, when asked to smile, her mouth elevated only on the left side. Other than slurred speech, there were no problems with speech syntax or the construction of sentences. The right side of Jane’s mouth drooped, and water dribbled from her mouth when she attempted to drink. Her right eye drooped, and did not close completely. When asked to raise her eyebrows, her eyebrows raised symmetrically. Her right arm and leg were weak, and when the doctor scratched the lateral plantar surface of her foot, the right great toe dorsiflexed, and the remainder of her toes flared. When the same procedure was performed on the left side, the toes curled downward.
Explanation
Jane has an example of a left-sided cerebral vascular accident. It is unlikely that this stroke involves the cerebral cortex because of the lack of cortical signs, such as aphasia or speech dysfunction.The equal involvement of the arm,leg,and face suggest that this occurred in a location where the pathways mediating these functions travel closely together, such as the internal capsule or the crus cerebri. Additionally, sensory signs were found, implicating a smaller region of dysfunction. A magnetic resonance imaging scan was obtained in the ER, which revealed a new internal capsule infarct that extended from the posterior limb into the genu. Note that the corticospinal fibers are contained in the posterior limb, and corticobulbar fibers are present in the genu. Thus, both of these fiber systems were damaged, which accounted for the deficits observed in this patient.
SUMMARY TABLE
Descending Motor Pathways in the Brain
|
Pathway |
Origin |
Distribution |
Function |
Effects of Lesion |
|
Corticospinal tract |
Area 4 (30%); area 6 (30%); areas 3,1,2(40%) |
All levels of spinal cord but mainly to cervical and lumbar levels |
Primary motor cortex: Planning of response; provides muscle contraction of individual muscles Primary somatosensory cortex: Provides sensory input to dorsal horn and dorsal column nuclei that filters out irrelevant stimuli from these nuclei that normally pass to somatosensory cortex Supplementary and premotor areas: Receive major input from posterior parietal cortex; coordinate voluntary movements; can activate groups of muscles, elicit postural adjustments, and control opening and closing of hands and body orientation |
Paralysis or weakness of movement, mainly of distal musculature; marked increase in muscle tone (hypertonia), spasticity, and presence of abnormal reflexes (Babinski, extensor plantar reflex); lesions of supplementary and premotor cortices can result in various forms of apraxia |
|
Corticobulbar tract |
Lateral aspects of the primary motor and somatosensory cortices |
Bilateral to most cranial nerves except contralateral to lower part of CN VII, CN XI, and CN XII |
Voluntary control over cranial nerve functions, especially motor and autonomic functions of cranial nerves |
Generally, weakness in muscles innervated by cranial nerves(pseudobulbar palsy), except for CN VII and CN XII where effects are more pronounced (i.e., jaw and tongue deviate to opposite side of lesion) |
|
Reticulospinal Tracts |
||||
|
Lateral reticulospinal tract |
Large-celled region of medulla |
Fibers from each tract descends to all levels of spinal cord,synapsing upon alpha and gamma motor neurons and interneurons |
Inhibits voluntary movements and reduces muscle tone |
Selective lesions limited to the reticulospinal tracts in humans have not been reported, but lesions, especially of the lateral reticulospinal tract, are believed to contribute to hypertonia and spasticity |
|
Medial reticulospinal tract |
Large-celled regions of pons |
Facilitates voluntary or cortically induced movements; increases muscle tone |
||
|
Pathway |
Origin |
Distribution |
Function |
Effects of Lesion |
|
|
Vestibulospinal Tracts |
|||
|
Lateral vestibulospinal tract |
Lateral vestibular nucleus |
Projects to all levels of spinal cord |
Facilitates alpha and gamma motor neurons of extensors and facilitates extensor reflexes |
Selective lesions limited to the vestibulospinal tracts in humans have not been reported, but are likely not to produce paralysis of muscles |
|
Medial vestibulospinal tract |
Medial vestibular nucleus |
Projects to cervical levels, bilaterally |
Activates lower motor neurons associated with spinal accessory nerve, assisting in the lifting and rotation of the head and shoulder blade |
|
|
Rubrospinal tract |
Red nucleus |
Pathway decussates near level of origin and descends mainly to cervical levels of spinal cord and indirectly to cerebellum |
Facilitates alpha motor neurons of flexor motor neurons and flexor reflexes |
Selective lesions limited to the red nucleus or rubrospinal tract have not been reported; lesions of the region of the red nucleus result in tremor and movement disorders, but such effects may be more closely associated with damage to fibers of passage associated with cerebellar and basal ganglia systems |