Cuneocerebellar Tract
The course of this tract is shown in Figure 9-8B. It should be recalled that the nucleus dorsalis of Clarke is not present in the spinal segments rostral to C8. Therefore, afferent fibers entering the spinal cord rostral to this level ascend ipsilaterally in the fasciculus cuneatus and project to neurons located in the accessory cuneate nucleus of the lower medulla. Neurons located in this nucleus then give rise to the cuneocerebellar tract, which is functionally related to the upper limb, conveying nonconscious proprioception. (Recall that the dorsal spinocerebellar tract is functionally related to the lower limb.) The fibers in this tract then terminate in the cerebellar cortex.
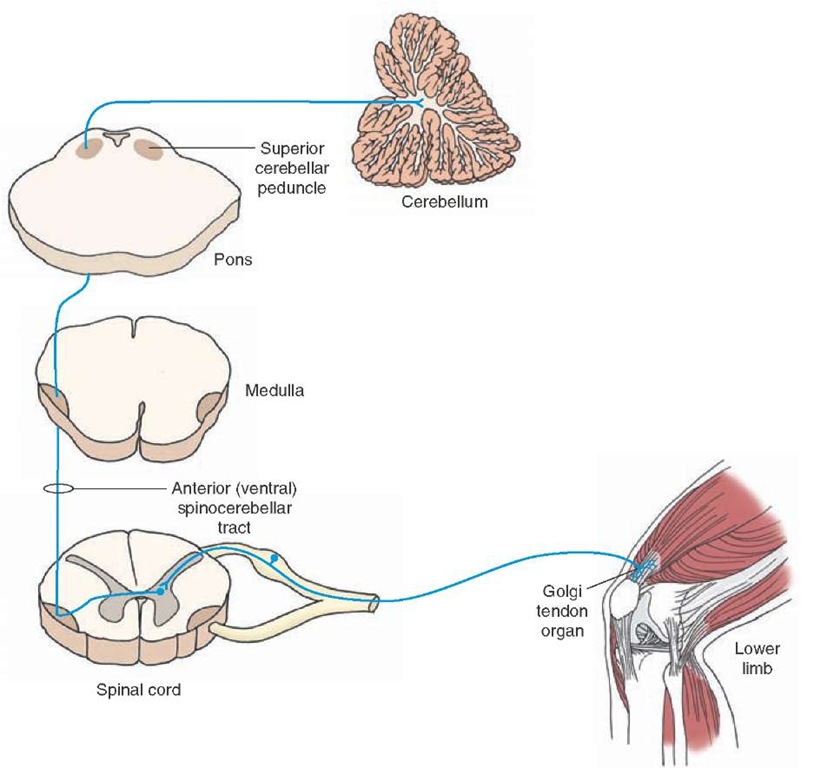
Ventral (Anterior) Spinocerebellar Tract
The course of this tract is shown in Figure 9-9. The first-order neurons in this system are located in the dorsal root ganglion; their peripheral processes innervate the Golgi tendon organs that are located at the junction of the muscle and tendon of the ipsilateral lower limbs. The central processes of the first-order neurons project to the second-order neurons located in the lateral part of the base and neck of the dorsal horn. The axons of the second-order neurons cross in the spinal cord and ascend through the medulla to the pons. The fibers then join the superior cerebellar peduncle (brachium conjunctivum) in the pons, cross again to the other side, and terminate in the vermal region of the anterior lobe of the cerebellum. Thus, the ventral (anterior) spinocerebellar tract crosses first in the spinal cord and then crosses again when it joins the superior cerebellar peduncle and crosses to terminate in the cerebellum. This tract conveys information about whole limb movements and postural adjustments to the cerebellum. Damage to this tract results in loss of noncon-scious proprioception and coordination in the lower limb.
FIGURE 9-9 The ventral (anterior) spinocere-bellar tract. Note that the tract first crosses in the spinal cord and then crosses a second time in the superior cerebellar peduncle and terminates in the cerebellum.
Rostral Spinocerebellar Tract
The course of this tract is similar to the ventral spinocer-ebellar tract except that the afferents are from the Golgi tendon organs located in the upper limb, the tract is uncrossed, and it enters the cerebellum via the inferior cerebellar peduncle. Damage to this tract results in loss of nonconscious proprioception and coordination in the upper limb.
Spinothalamic Tract
Conventionally, it was believed that the lateral spinotha-lamic tract transmits pain and temperature sensations, whereas the anterior spinothalamic tract transmits the sensation of nondiscriminative touch to the primary sensory cortex. This concept has recently been revised. Currently, it is believed that pain and temperature sensations are transmitted primarily via the spinothalamic tract, which ascends in the ventrolateral quadrant of the spinal cord located contralateral to the side where the afferents carrying these sensations enter the spinal cord. Pain sensation is complex. It includes the perception of noxious stimuli (discriminative component), emotional and autonomic responses to such stimulation, and an increased level of attention (arousal-emotional component). Multiple pathways mediate the discriminative and arousal-emotional components of pain sensation. Because these pathways ascend in the ventrolateral quadrant of the spinal cord, they are collectively known as the anterolateral system of ascending tracts.
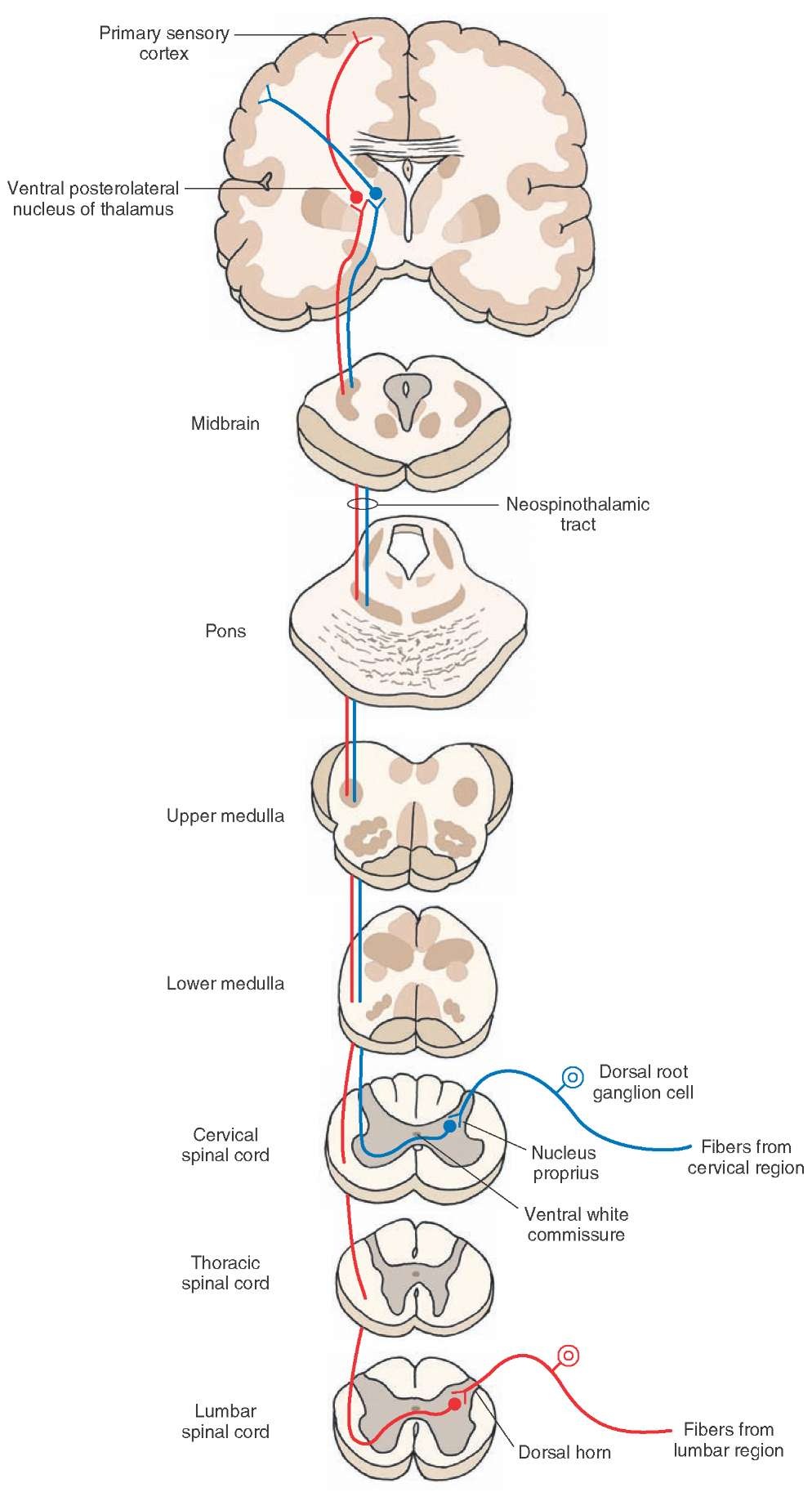
The spinothalamic tract consists of the following components: (1) The direct pathway, consisting of the neospi-nothalamic tract, mediates pain, temperature, and simple tactile sensations; whereas indirect pathways, consisting primarily of paleospinothalamic, spinoreticular, and spi-nomesencephalic tracts, mediate the affective and arousal components of these sensations. These pathways are described below. Direct Pathway
Neospinothalamic Tract. The course of this tract is shown in Figure 9-10. The neurons that give rise to this tract arise mainly from the nucleus proprius (proper sensory nucleus) that is located in laminae III and IV of the dorsal horn. The axons of these neurons cross obliquely via the ventral (anterior) white commissure to enter the contral-ateral white matter where they ascend in the lateral funic-ulus. This tract has a somatotopic organization throughout its course, including in the spinal cord. Fibers arising from the lowest part of the body (the sacral and lumbar levels of spinal cord) ascend dorsolaterally, whereas those arising from the upper extremities and neck (the cervical cord) ascend ventromedially. The ascending axons synapse on third-order neurons located primarily in the ventral poste-rolateral nucleus of thalamus that, in turn, project to the primary sensory cortex in the postcentral gyrus.
FIGURE 9-10 Direct spinothalamic pathway: the neospinothalamic tract. The peripheral processes of these dorsal root ganglion cells end as receptors sensing pain, temperature, and simple tactile sensations. The central processes of these dorsal root ganglion cells synapse with the neurons of the nucleus proprius. The axons of these second-order neurons cross via the anterior white commissure, enter the contralateral white matter, ascend in the lateral funiculus, and synapse on third-order neurons located in the ventral posterolateral nucleus of the thalamus. The axons of third-order neurons project to the primary sensory cortex.
Deficits After Damage to the Direct Neospinothalamic Pathway. Sectioning of the direct neospinothalamic pathway at the cervical level on one side results in complete loss of pain (anesthesia), temperature (thermoanesthesia), and simple tactile sensations on the contralateral side of the body (upper and lower limbs and trunk). The loss of pain sensation is experienced about one to two levels below the lesion because the first-order afferent fibers contained in the zone of Lissauer ascend or descend one to two levels before making synaptic contact with second-order neospinothalamic neurons. If a lesion is present at the lumbar level, then there would be a loss of pain, temperature, and simple tactile sensations in the contralateral lower limb and trunk.
Loss of pain, temperature, and tactile sensations can also occur at a specific segment after damage to the area around the central spinal canal. This occurs in a condition called syringomyelia, in which there is an expansion of the central canal of the spinal cord. In addition, the glial cells proliferate around the central canal. In this case, the crossing fibers from the neospinothalamic tract on each side are affected but only in or about the segment in which the lesion is present. Accordingly, such a disorder results in bilateral loss of pain, temperature, and simple tactile sensations at the affected segment.
As noted earlier, the neospinothalamic tract is somato-topically organized in such a manner that sacral and lumbar fibers lie dorsolateral to the thoracic and cervical fibers. Accordingly, an expanding lesion or tumor located in the gray matter within the spinal cord is likely to affect the thoracic and cervical fibers first, whereas the sacral and lumbar fibers would be affected later, if at all. This clinical phenomenon, in which damage to the spinothalamic tracts leaves intact the pain, temperature, and simple tactile sensations in sacral dermatomes, is referred to as sacral sparing.
Damage to the dorsal columns as well as to the neospi-nothalamic tracts on one side elicits the following symptoms. On the ipsilateral side below the level of the lesion, there is a loss of conscious proprioception, but the sensations of pain, temperature, and simple touch are preserved. On the contralateral side below the level of the lesion, just the reverse is true; that is, there is a loss of pain, temperature, and simple tactile sensations, while conscious prop-rioception is preserved.
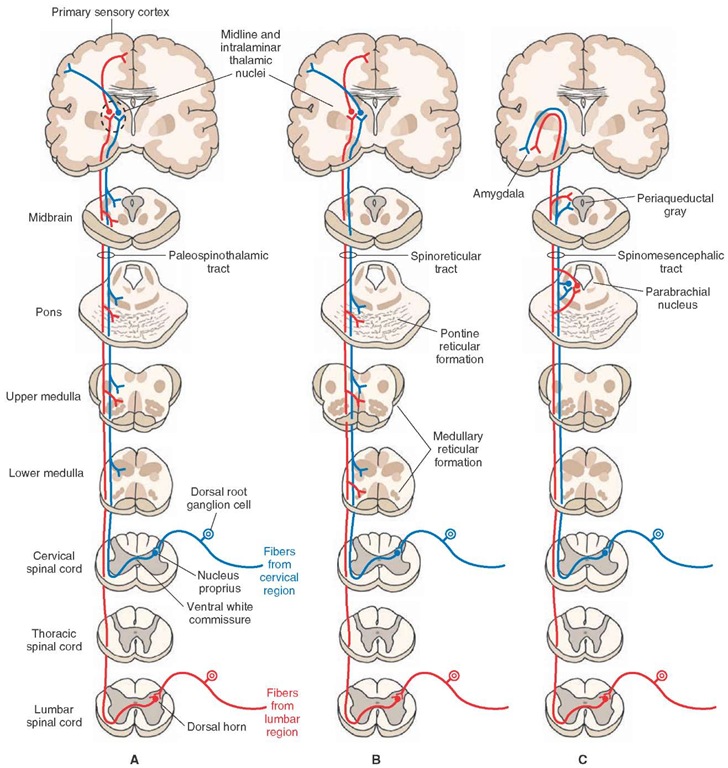
Indirect Pathways. These pathways are involved in the autonomic, endocrine, motor, and arousal components of pain, temperature, and simple tactile sensations. Indirect pathways are also involved in activation of pain-inhibiting mechanisms.The axons of these neurons ascend in the spinal cord bilaterally, show poor somato-topic organization, and make multiple synapses in the reticular formation, hypothalamus, and limbic system. The pathways described in the following sections are included in this system.
Paleospinothalamic Tract. The neurons of this pathway are located in the dorsal horn and intermediate gray matter.
The axons of these neurons ascend contralaterally as well as ipsilaterally in the ventrolateral quadrant of the spinal cord (ipsilateral projection is not shown in Fig. 9-11A). The axons ascending in the spinal cord make several synapses in the reticular formation of the brainstem (medulla, pons, and midbrain) and finally project to the midline and intralaminar thalamic nuclei.These nuclei, in turn, project in a diffuse manner to the cerebral cortex, especially to limbic regions such as the cingulate gyrus.
Spinoreticular Tract. The neurons of this pathway are also located in the dorsal horn and intermediate gray matter. One group of these axons terminates in the medullary reticular formation and another ascends to the pontine reticular formation.The projections from the spinal cord to the brain-stem are both crossed and uncrossed (uncrossed projection is not shown in Fig. 9-11B). Although details regarding the projections of ascending spinoreticular fibers have not been delineated, it is believed that these fibers transmit sensory information to the reticular formation, which, in turn, activates the cerebral cortex through secondary and tertiary projections via the midline and intralaminar tha-lamic nuclei.The thalamocorti-cal projections, in turn, are highly diffuse and influence wide areas of the cerebral cortex.
Spinomesencephalic Tract. The neurons of this pathway are also located in the dorsal horn and intermediate gray matter. The axons of these neurons ascend to the midbrain where they terminate in periaqueductal gray (PAG), a region surrounding the cerebral aqueduct (Fig. 9-11C). This pathway presumably activates PAG neurons, which send descending indirect projections to the spinal cord to inhibit pain sensation at this level.As is the case with spinoreticular fibers, details regarding the distribution of spinomesencephalic fibers have not been clearly established. It is believed that sensory information associated with this tract is transmitted to the amygdala via parabrachial nuclei.
Long Descending Tracts
These tracts mediate motor functions including voluntary and involuntary movement, regulation of muscle tone, modulation of spinal segmental reflexes, and regulation of visceral functions. The corticospinal tract arises from the cerebral cortex, and the tectospinal and rubro-spinal tracts arise from the midbrain. The remaining tracts arise from different nuclear groups within the lower brainstem. These tracts include the lateral and medial vestibulospinal and reticulospinal tracts that arise from the pons and medulla. In addition, other descending pathways that arise from medullary nuclei modulate auto-nomic functions. It should be noted that the corticospi-nal and rubrospinal pathways are mainly concerned with control over the flexor motor system and fine movements of the limbs, whereas the vestibulospinal and reticulospi-nal systems principally regulate antigravity muscles, posture, and balance.
FIGURE 9-11 Indirect spinothalamic pathways. These pathways mediate the affective and arousal components of pain, temperature, and simple tactile sensations. (A) The ascending axons in the paleothalamic tract synapse in the brainstem reticular formation and neurons in midline and intralaminar thalamic nuclei, which then project diffusely to the cerebral cortex including the cingulate gyrus. (B) In the spinoreticular tract, one group of ascending axons projects to the medullary reticular formation, and the other group projects to the pontine reticular formation. The neurons in the reticular formation then project to neurons located in the midline and intralaminar thalamic nuclei. These thalamic neurons then project to the cerebral cortex. (C) In the spinomesencephalic tract, ascending axons terminate on the periaqueductal gray neurons that, in turn, project to neurons in the amygdala via the parabrachial nuclei.