Pathological Activity Within Limbic Circuits
Because epilepsy is a major disorder associated with the limbic system and, in particular, with temporal lobe structures, we include the following discussions of epilepsy and the application of the electroencephalogram (EEG).
Measurement of Brain Activity: The Electroencephalogram
The EEG is recorded at the scalp and sometimes from the surface of the brain during epilepsy surgery. It measures potential differences between two active electrodes on the scalp or between a scalp electrode and an inactive electrode, which is usually placed behind the ear. The EEG measures the summation of excitatory postsynaptic potentials (EPSPs) and inhibitory postsynaptic potentials from the scalp. Because these signals are low in amplitude, a differential amplifier is used to make the waves more visible. Gold or platinum electrodes are placed on the scalp after thorough cleaning with an abrasive agent. The pins from the wire attached to the electrodes are plugged into a jack-box that is attached by cable to the amplifier.
There are many characteristic waveforms seen on both normal and abnormal EEGs. For instance, when a normal subject lies quietly, an alpha rhythm is found in the occipital leads. This disappears with eye opening. If this rhythm is slow or absent, then there may be a neurologic problem. States of alertness are characterized by waves of lower amplitude and higher frequency (see Fig. 23-10). Similarly, epileptiform spikes are sharp waves followed by a slow wave, and the presence of these entities is abnormal. If the patient has had seizures or questionable seizures in the past, then the presence of epileptiform spikes will assist in making the diagnosis. Additionally, certain patterns, such as a 3-per-second spike and wave when the patient has had a history of staring spells, will assist in making the diagnosis of an absence seizure. Likewise, waves of 4 to 7 Hz recorded over the temporal lobes or within the hippocam-pal formation, called a theta rhythm, reflect a dysfunction of hippocampal tissue in humans. In lower forms of animals, theta rhythms may appear normal when recorded from hippocampal tissue, especially during conditions reflecting altered motivational states, such as when an animal is approaching a goal. Delta rhythms are defined as very slow, 1-Hz to 3-Hz, synchronous waves that occur under conditions of severe trauma to the brain (e.g., brain tumors). They also occur normally for short periods during sleep. EEG is also useful in other disorders, such as coma.
Epilepsy
Seizures can be defined as paroxysmal events in which there is a significant change in the EEG that correlates with a change in behavior and/or consciousness. Seizures may also include generalized convulsions, sensory experiences (either prior to or during the seizure), and a variety of motor activities. Seizures are usually stereotyped for each patient, and some patients with severe epilepsy may have multiple seizure types.
Epilepsy can be defined as a condition in which seizures are recurrent. Seizures may develop as a result of the spreading of EPSPs, which discharge synchronously from either abnormal neurons or metabolic problems that lower seizure potential. Seizure disorders may be idiopathic, but they also may occur as a result of a mass lesion, such as brain tumors and vascular malformations, infections, drugs and drug withdrawal, and metabolic problems. The time of the occurrence of the seizure is called the ictal period; the time following the seizure is called the postictal period; and the time between seizures is called the interictal period.
Seizures can be classified into two basic types: (1) partial or focal, meaning that the seizure arises from specific regions of the brain and is limited to one hemisphere, or (2) generalized, meaning seizures arise diffusely throughout the brain, causing a loss of consciousness. The EEG also classifies seizure types. The EEG helps to define whether seizures arise from one or more specific areas or whether they develop diffusely.
Partial seizures can be classified as either simple partial or complex partial seizures. Simple partial seizures do not cause a change in consciousness, but the patient experiences various sensory and motor symptoms, usually not lasting more than 1 to 2 minutes. Motor signs described in simple partial seizures include focal motor clonic activity and a focal Jacksonian March, in which seizure activity begins locally over the cortex, causing either sensory or motor activity directly corresponding to the homuncu-lus of either the sensory or motor cortex. The patient experiences a "march" of sensory or motor activity from muscle to muscle in the same order as the homunculus. Other types of simple partial seizures include those that generate sensory phenomena such as somatosensory, visual, olfactory, gustatory, and vestibular sensations. These seizures may also contain autonomic symptoms including a rising epigastric sensation, pallor, sweating, and pupillary dilation. Psychic symptoms may also be found in simple partial seizures, but when these are present, the patient will also progress to a complex partial seizure with impairment of consciousness. Examples of psychic phenomena include dysphasia, which is a speech difficulty that is a less severe form of aphasia. The patient may also experience deja vu, fear, anger, macropsia (i.e., things appearing larger than they are), or micropsia (i.e., things appearing smaller than they are). Often, simple partial seizures are called an "aura," meaning that they provide a warning of the spread of the seizure, causing a complex partial seizure.
The most common type of seizure is the complex partial seizure (sometimes called psychomotor seizures). These seizures are characterized by an impairment or loss of consciousness. They may begin with an aura (simple partial seizure), but this is not necessary for the diagnosis of this seizure type. During the seizure, the patient may stare and not respond to commands. The patient may exhibit automatisms, which are automatic, stereotypic, and nonpurposeful behaviors such as chewing, lip smacking, or grabbing objects. Complex partial seizures may spread from a single focus to the entire cortex, resulting in secondary generalization. The patient initially has complex partial seizures that evolve into generalized tonic-clonic seizures as a result of the diffuse spread of the seizure. Postictal periods of sleepiness are common in this seizure type.
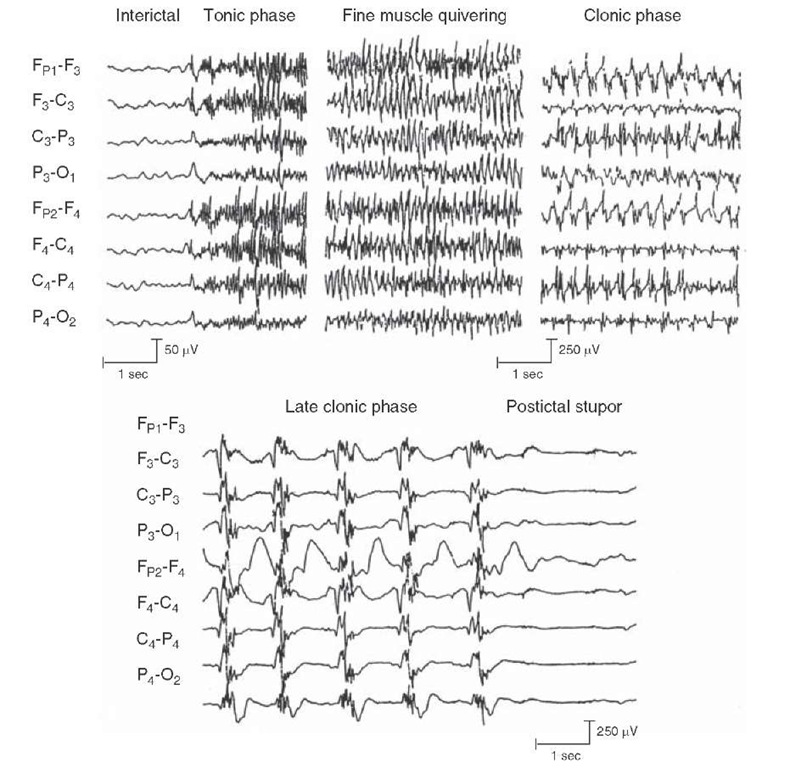
Generalized seizures arise diffusely from the cerebral cortex. All generalized seizures reveal epileptic activity diffusely. One common type of generalized seizure is the generalized tonic-clonic seizure (Fig. 25-8). These seizures, often called "convulsions," involve a tonic phase or stiffening, followed by a clonic phase in which the extremities contract the agonistic and antagonistic muscles. The clonic phase begins with rapid movements, which then slow until they stop, and the patient remains unconscious. Often at the beginning of these seizures, the patient will attempt to force air through a tonic airway, causing an "epileptic cry." Most of these seizures are not dangerous and last only 1 to 2 minutes. Prolonged seizure activity or the generation of two or more of these seizures in a row without regaining consciousness is called status epilepti-cus. This condition is a neurologic emergency with a high morbidity and mortality.
Other types of generalized seizures include absence, myoclonic, and atonic seizures. Absence seizures are very brief (approximately 3-10 seconds long), and the patient is unresponsive, commonly described as "daydreaming" (Fig. 25-9). When the patient is tested during the seizure, all behavioral functions cease but begin again after the seizure, indicating that there is no effective postictal period. The classic finding on the EEG is a 3-per-second spike and wave complex. Myoclonic seizures are very brief and characterized by a rapid muscle jerk accompanied by polyspike and wave complexes, which are also brief. Atonic seizures, which are found mainly in children with neurologic disorders, consist of a very brief complete loss of muscle tone. These seizures are further characterized by a brief burst of polyspike and slow-wave complexes.
FIGURE 25-8 Electroencephalogram records showing a generalized tonic-clonic seizure. The various segments illustrate the interictal phase (prior to the seizure); the tonic phase (where the body is stiff) with repetitive spiking; a clonic phase (where body is jerking), which shows spike and waves; and a postictal phase (where no seizure activity is present).
FIGURE 25-9 Absence seizure. Electroencephalogram records illustrating an absence seizure consisting of a 3-Hz spike and wave pattern, at which time the patient was unresponsive.
One of the unique features of temporal lobe neurons, which include those cells that lie in the pyriform cortex, hippocampal formation, and parts of the amygdala, is their low threshold for seizure discharges. In particular, one region of the hippocampus, called Sommer’s sector, consists of CA1 neurons that are highly susceptible to anoxia at birth and that are also damaged in patients who have epilepsy with a primary focus in the hippocampus. Seizure discharges associated with hippocampal epilepsy are commonly characterized by high-frequency, high-amplitude synchronous discharges of large groups of cells that become self-sustaining. Typically, partial seizures are limited to the region of the hippocampus that has no behavioral concomitant. The patient sits quietly and appears unaware of his surroundings during the time of the seizure (i.e., ictal period). The patient may appear confused and experience auditory, olfactory, vertiginous, or even gustatory hallucinations. Such seizures are often identified by EEG recordings. As indicated earlier in this topic, such emotional responses as aggressive behavior may be associated with seizures of the temporal lobe, occurring in the postictal or interictal periods. Such responses occur frequently when attempting to look toward the patient or give the patient directions. Seizures may evolve from multiple sources. Typically, they result from anoxia at birth or from head injuries or tumors in adults. Such damage may involve vascularization, glial formation, or fibrosis, which serve as irritative foci for seizure development.
Seizures are mainly treated with anticonvulsant medications. However, patients with seizures that are intractable to multiple medications may be candidates for other options, such as the surgical removal of the epileptic focus (if there is one clear focus); vagus nerve stimulation, which has been used successfully for the treatment of seizures when drug therapy is unsuccessful; and in young children suffering from an inborn error of metabolism (phenylketonuria), a restricted protein diet, which gives rise to ketones.
Clinical Case
History
Chuck is a 58-year-old chairman of a neurology department, who has always performed well professionally and never had any significant health problems. In the past year or two, both his colleagues and family have noticed that his behavior has changed. Although he was mildly impulsive and prone to rage attacks at home in the past, recently, Chuck has begun to have more violent, inappropriate rage attacks at work, as well. When a nurse was slow in passing him a reflex hammer while examining a patient in his office, he threw it at her. When he believed that a colleague did not produce a result quickly enough, he accused her of not trying hard enough, threw a floppy disc at her, and ordered her out of the hospital. Additionally, he was pursuing women inappropriately,even at work, despite having a relatively stable marriage. One of his colleagues found him taking liberties with his secretary, despite obvious protests on her part. He propositioned women in front of his wife, who became so upset that she demanded that he either see a psychiatrist or she would divorce him. However, 2 days prior to his appointment. Chuck had an episode characterized by a "funny smell" and then stared motionless for approximately 2 minutes. While he was staring into space, his secretary observed him chewing and smacking his lips. When she asked him if he was all right, he did not answer. When he began to speak again, he simply said that he was tired and went to lie down. At this point, his secretary became concerned, and she called a fellow neurologist, who examined him the same day.
Examination
On examination, there were no obvious abnormalities, with the exception of a visual field deficit in the right upper quadrant of each eye. Smell and hearing were intact.AII motorfunctionsand languagefunctionwerealsonormal.The neurologist ordered a magnetic resonance imaging (MRI) scan and an electroencephalogram (EEG).The MRI of Chuck’s head revealed a left side anterior temporal mass, which, upon further investigation, was identified as a glioma. The tumor was growing slowly as evidenced by the lack of significant swelling surrounding the tumor.
Explanation
The staring episode is called a complex partial seizure or paroxysmal storm of initially localized activity, which appears on an EEG to be rhythmic, excitatory activity. Clinically, these seizures are manifested as stereotypic staring spells, sometimes involving various automatic behaviors. Because stimulation of certain regions of the limbic system, including the corticomedial amygdaloid nuclei, can induce anger and rage, a tumor in this region can produce behavioral changes of this sort. Hypersexuality and indiscriminate sexual behavior can also be found with lesions of this region, even unilaterally. Bilateral lesions of the amygdala commonly cause hypersexuality as part of the Kluver-Bucy syndrome. The superior quadrantanopsia or "pie-in-the-sky" visual field defect occurs as a result of interruption of fibers from the upper visual field as they travel through the temporal lobe. It may go unnoticed initially because the patient is easily able to compensate for small visual field defects.
SUMMARY TABLE
The Limbic System: Afferent and Efferent Connections, Functions and Dysfunctions
|
Structure |
Afferent Connections |
Efferent Connections |
Functions |
Dysfunctions |
|
Hippocampal formation |
Cingulate gyrus, septal area,entorhinal and pyriform cortices, brainstem monoamine neurons |
Medial hypothalamus and mammillary bodies, anterior nucleus of thalamus,septal area |
Short-term memory processes, modulation of hypothalamic processes, in particular, emotional and endocrine functions |
Temporal lobe epilepsy, short-term memory disorders; aggressive and rage behavior, possible endocrine dysfunctions |
|
Septal area |
Hippocampal formation, hypothalamus, brainstem monoamine neurons |
Hippocampal formation, medial hypothalamus, including mammillary bodies |
Modulates aggression and rage and other functions of the hypothalamus; also serves as a relay of hippocampal formation to hypothalamus |
Emotional disorders, including rage and aggression, and related functions of hypothalamus |
|
Amygdala |
Substantia innominata, temporal neocortex, medial geniculate nucleus, solitary nucleus, prefrontal cortex, brainstem monoamine neurons, pyriform and olfactory cortices |
Medial and lateral hypothalamus, midbrain periaqueductal gray, prefrontal cortex, medio dorsal thalamic nucleus |
Fear, regulation of aggression and rage, functions associated with hypothalamus, including feeding, endocrine and autonomic processes |
Emotional disorders, e.g., aggression, rage, and loss of fear; disruption of other functions associated with hypothalamus, e.g., endocrine functions and eating disorders; temporal lobe epilepsy |
|
Prefrontal cortex |
All parts of cerebral cortex, mediodorsal thalamic nucleus, brainstem monoamine neurons |
Mediodorsal thalamic nucleus, hypothalamus, midbrain periaqueductal gray |
Cognitive, autonomic, and emotional processes, including the control over aggression and rage |
Loss of control over emotional processes, autonomic functions, flat personality, memory and intellectual deficits |
|
Basal forebrain: nucleus accumbens, substantia innominata |
Brainstem monoamine neurons, in particular dopamine neurons from ventral tegmental area, some inputs from basal ganglia, some inputs from amygdala, from nucleus accumbens to substantia innominata |
From nucleus accumbens to ventral tegmental area and to substantia innominata; from substantia innominata to hypothalamus, and to wide areas of cerebral cortex and limbic structures |
Nucleus accumbens mediates mood states; basal nucleus of Meynert of substantia innominata is cholinergic and is believed to mediate memory functions of cerebral cortex |
Dysfunctions of nucleus accumbens may be associated with addictive behavior; damage to basal nucleus of Meynert is associated with Alzheimer’s disease |