Functions of the Parasympathetic Nervous System
Activation of the parasympathetic division of the auto-nomic nervous system results in conservation and restoration of body energy. For example, a decrease in heart rate brought about by the activation of the parasympathetic nervous system will also decrease the demand for energy, whereas the increased activity of the gastrointestinal system will promote restoration of body energy. The effects of parasympathetic activation are localized and last for a short time. Important differences between the sympathetic and parasympathetic nervous system are shown in Table 22-1.
Enteric Division
The enteric division consists of neurons in the wall of the gut that regulate gastrointestinal motility and secretion. The enteric system consists of two layers of neurons that are present in the smooth muscle of the gut: the myenteric (Auerbach’s) and submucosal (Meissner’s) plexuses. The neurons of the myenteric (Auerbach’s) plexus control gastrointestinal motility, whereas the neurons of the submu-cosal (Meissner’s) plexus control water and ion movement across the intestinal epithelium. Excitatory transmitters of motor neurons and interneurons in the smooth muscle of the GIT are probably acetylcholine and substance P. Inhibitory transmitters are not yet known. The enteric nervous system is intrinsically active.
The enteric system is also controlled by sympathetic and parasympathetic innervation (extrinsic innervation). The sympathetic innervation is derived from branches of thoracic, lumbar, and sacral sympathetic chains. Most of the sympathetic fibers of the extrinsic innervation are postganglionic. The parasympathetic innervation is derived from the vagus and pelvic nerves. Most of the par-asympathetic fibers of the extrinsic innervation are pre-ganglionic. The extrinsic system can override the intrinsic system when the sympathetic or parasympathetic nervous system is activated.
TABLE 22-1 A Comparison Between the Sympathetic and Parasympathetic Divisions of the Autonomic Nervous System
|
Parasympathetic |
Sympathetic |
|
|
Preganglionic neurons: location |
Nucleus of oculomotor nerve (pupil)"; superior salivatory nucleus of facial nerve (lacrimal, sublingual, and submandibular salivary glands); inferior salivatory nucleus of glossopharyngeal nerve (parotid salivary glands); dorsal motor nucleus of vagus (GIT, kidney); nucleus ambiguus (heart); IML of the sacral spinal cord at S2-S4 level (colon, rectum, urinary bladder, sex organs); |
Intermediolateral cell column of the spinal cord (T1-L2). |
|
Preganglionic neurons: outflow |
CN III, VII, IX, X; pelvic nerves |
Ventral roots at T1-L2 |
|
Preganglionic fibers; transmitter at their terminals (within ganglia) |
Myelinated; the preganglionic fibers are relatively long because the ganglia receiving them are located within the target organ or close to it; acetylcholine |
Myelinated; the preganglionic fibers are relatively short because the ganglia receiving them are located at some distance from the target organ; acetylcholine |
|
Ganglia |
Ganglia located close to the organs (ciliary, otic); ganglia located within the organs (heart, bronchial tree, GIT) |
Paravertebral ganglia in sympathetic chain (25 pairs); prevertebral ganglia (celiac, renal, superior, and inferior mesenteric) |
|
Postganglionic fibers Transmitter at the terminals of postganglionic fibers |
Short, nonmyelinated Acetylcholine |
Long, nonmyelinated Norepinephrine (acetylcholine in sweat glands). |
|
Ratio of preganglionic to postganglionic neurons and extent of action |
Single preganglionic fiber may connect with only one or two postganglionic neurons; this arrangement favors localized actions |
Single preganglionic fiber may connect with numerous postganglionic neurons; this arrangement results in widespread responses |
CN = cranial nerve; T = thoracic spinal segment; L = lumbar spinal segment; GIT = gastrointestinal tract; IML = intermediolateral cell column. ‘ Target organ is shown in parentheses.
AUTONoMIC INNERVAtION of SOmE SElECTED ORgANS
Many organs receive dual innervation (i.e., from the sympathetic as well as the parasympathetic divisions of the autonomic nervous system). As a rule, in most of the organs with dual innervation, activation of the parasympa-thetic and sympathetic divisions has antagonistic actions. Exceptions to this rule are the salivary glands, where activation of either system results in increased secretion of saliva: Sympathetic stimulation produces viscous saliva, whereas parasympathetic stimulation produces watery saliva. The autonomic innervation of some selected organs is discussed in the following sections.
Upper Eyelid
The upper eyelid is raised by the levator palpebrae superior muscle. The bulk of levator palpebrae superioris is a skeletal muscle that is innervated by the caudal-central nucleus of the oculomotor nuclear complex. A small portion of this muscle, the tarsal muscle, consists of smooth muscle fibers that receive innervation from sympathetic postganglionic fibers arising from the superior cervical ganglion (Fig. 22-3A). The orbital muscle of Muller is also nonstri-ated and maintains the eyeball in a forward position in the orbit. This muscle is also innervated by sympathetic post-ganglionic fibers arising from the superior cervical ganglion. Sympathetic preganglionic fibers synapsing on the postganglionic neurons in the superior cervical ganglion arise from the IML at the T1—T4 level. Interruption of the sympathetic innervation to the tarsal muscle results in pseudoptosis (partial drooping of the upper eyelid), and damage to the orbital muscle of Muller results in enoph-thalmos (sinking of the eyeball in the orbit). These symptoms are characteristic of Horner’s syndrome (described later in this topic). It should be noted that damage to the oculomotor nerve also causes paresis of the levator palpebrae superioris muscle, which results in ptosis (drooping of the upper eyelid).
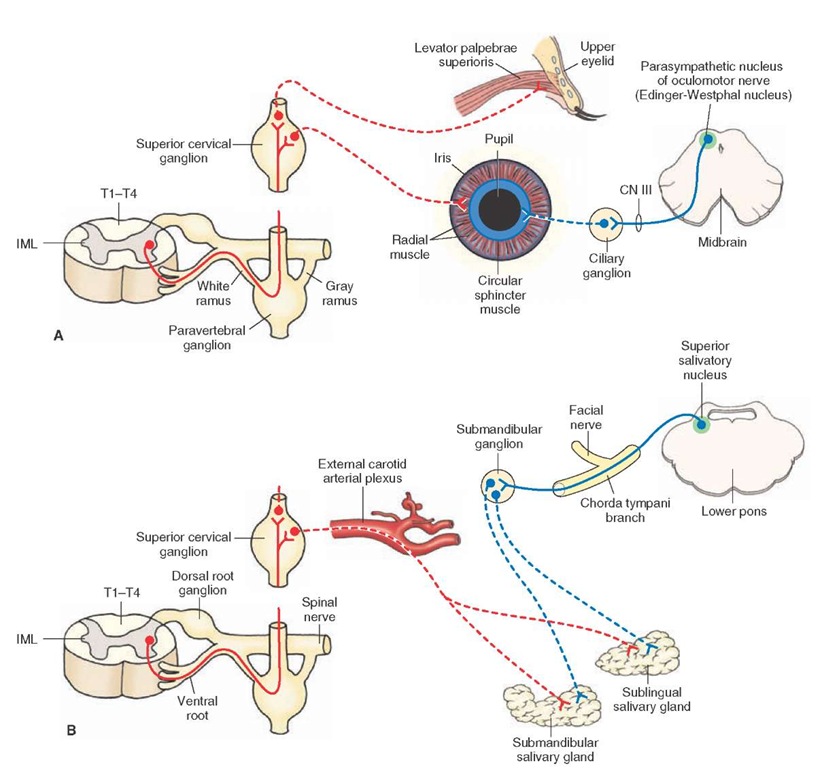
FIGURE 22-3 Autonomic innervation of the eye. (A) The upper eyelid and iris. (B) Sublingual and submandibular glands. Red = sympathetic nervous system; Blue = parasympathetic nervous system. Solid lines = preganglionic fibers, dotted lines = postganglionic fibers. T = thoracic spinal segment; IML = intermediolateral cell column; CN = cranial nerve.
Sympathetic Innervation
The axons of sympathetic preganglionic neurons, which are located in the IML at the T1 level, synapse on neurons in the superior cervical ganglia. The postganglionic sympathetic fibers arising from the latter innervate the radial smooth muscle fibers of the iris (Fig. 22-3A). Activation of the sympathetic nervous system results in contraction of the radial muscles of the iris, which causes mydriasis (pupillary dilation).
Parasympathetic Innervation
The axons of the parasympathetic preganglionic neurons located in the Edinger-Westphal nucleus (parasympa-thetic nucleus of the oculomotor nerve) leave the brain-stem through the oculomotor nerve (CN III) and synapse on the parasympathetic postganglionic neurons in the ciliary ganglion that is located in the orbit. The postgangli-onic fibers from the ciliary ganglion enter the eyeball and innervate the circular (sphincter) smooth muscle fibers of the iris (Fig. 22-3A) and the circumferential muscles of the ciliary body. When the parasympathetic innervation to the eye is activated, the circular muscles of the pupil and the circumferential muscles of the ciliary body contract. Contraction of circular muscles of the iris causes miosis (constriction of the pupil). Contraction of circumferential muscles of the ciliary body results in the relaxation of the suspensory ligaments of the lens. The lens becomes more convex, thus allowing for greater refraction of the light rays, which is more suitable for near vision. These two responses (i.e., constriction of the pupil and making the lens more convex) are included in the accommodation reflex.
Sublingual and Submandibular Salivary Glands
Sympathetic Innervation
The preganglionic neurons that provide sympathetic innervation to these glands are located in the T1—T4 level of the IML. The preganglionic fibers synapse on postgan-glionic neurons in the superior cervical ganglion. The postganglionic fibers pass through the external carotid arterial plexus and innervate these glands (Fig. 22-3B). Activation of the sympathetic innervation to the sublingual and submandibular glands produces viscous salivary secretions.
Parasympathetic Innervation
The parasympathetic preganglionic fibers arising from the neurons located in the superior salivatory nucleus leave the lower pons through the facial nerve (CN VII). These fibers exit through the chorda tympani branch of the facial nerve and synapse on postganglionic neurons in the submandibular ganglion. The postganglionic para-sympathetic fibers from the submandibular ganglion innervate sublingual and submandibular salivary glands (Fig. 22-3B). Activation of these parasympathetic fibers (secretomotor fibers) results in the secretion of watery saliva.
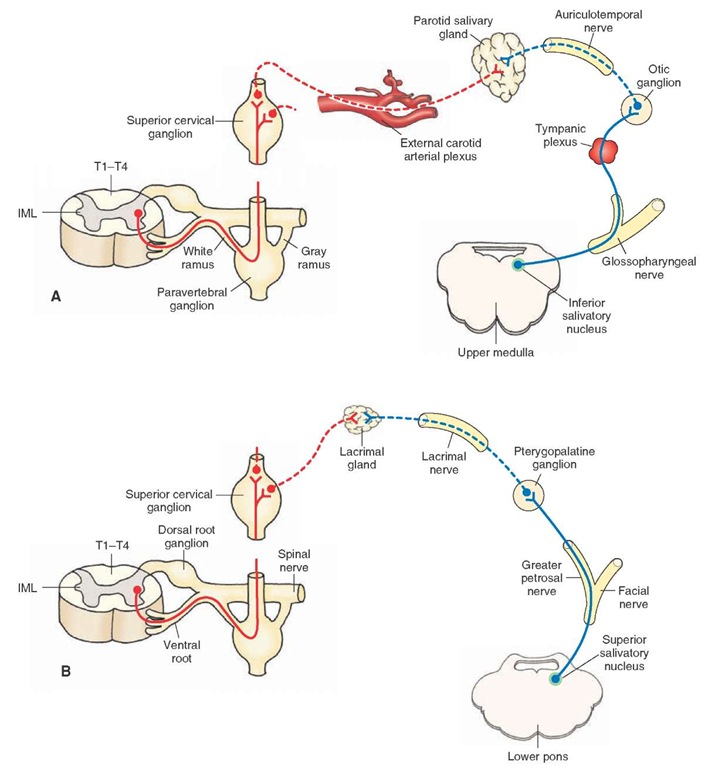
Parotid Salivary Glands
Sympathetic Innervation
The preganglionic neurons that provide sympathetic innervation to the parotid salivary glands are located in the T1-T4 level of the IML. The preganglionic fibers synapse on postganglionic neurons in the superior cervical ganglion. The postganglionic fibers pass through the external carotid arterial plexus and innervate the parotid salivary gland (Fig. 22-4A). Activation of the sympathetic innervation to these glands produces viscous salivary secretions.
Parasympathetic Innervation
The axons of the neurons located in the inferior saliva-tory nucleus, which is located in the upper medulla, exit through the glossopharyngeal nerve (CN IX). The para-sympathetic preganglionic fibers pass through the tympanic plexus and synapse on postganglionic neurons located in the otic ganglion. The parasympathetic post-ganglionic fibers from the otic ganglion pass through the auriculotemporal nerve and innervate the parotid salivary gland (Fig. 22-4A). Activation of these fibers results in secretion of watery saliva from the parotid gland into the oral cavity.
Lacrimal Glands
Sympathetic Innervation
The sympathetic fibers innervating the lacrimal gland follow the same course that was described for the sympathetic innervation of the sublingual and submandibular glands (Fig. 22-4B). The effects of activation of the sympathetic nervous system on secretion of the lacrimal glands are not clearly established.
Parasympathetic Innervation
The parasympathetic preganglionic fibers arising from the superior salivatory nucleus (located in the lower pons) exit through the greater petrosal branch of the facial nerve and synapse on the postganglionic neurons in the ptery-gopalatine ganglion. The postganglionic fibers from these neurons reach the lacrimal gland through the lacrimal nerve (Fig. 22-4B). Activation of these postganglionic par-asympathetic fibers results in secretion of tears.
Heart
Sympathetic Innervation
The sympathetic preganglionic neurons innervating the heart are located in the T1—T4 spinal segments. The sympathetic preganglionic fibers enter the sympathetic chain via the ventral roots and synapse on postganglionic neurons located in the thoracic ganglia (1-4) and inferior, middle, and superior cervical ganglia. Sometimes, the last two cervical and first two thoracic ganglia are fused to form the star-shaped stellate ganglion. Sympathetic postgangli-onic innervation to the heart arises from thoracic ganglia (1-4) and inferior, middle, and superior cervical ganglia. Sympathetic postganglionic fibers innervating the heart also arise from the stellate ganglion when it is present.
FIGURE 22-4 Autonomic innervation of (A) the parotid salivary gland and (B) the lacrimal gland (see text for details). Red = sympathetic nervous system; Blue = parasympathetic nervous system. Solid lines = preganglionic fibers, dotted lines = postganglionic fibers. T = thoracic spinal segment; IML = inter-mediolateral cell column.
The sympathetic postganglionic fibers arising from these ganglia innervate all regions of the heart (sinoatrial node, atria, atrioventricular node, and ventricles [Fig. 22-5]). Activation of the sympathetic nervous system results in an increase in heart rate by increasing the pacemaker activity of the sinoatrial node cells. Impulse conduction at the atrioventricular node and the contractile force of atrial and ventricular muscle fibers are increased.
Parasympathetic Innervation
Animal experiments have shown that preganglionic neurons providing parasympathetic innervation to the heart are predominantly located in the region surrounding the compact zone of the nucleus ambiguus (Fig. 22-5). A component of the parasympathetic innervation to the heart arises also from the dorsal motor nucleus of vagus. These two nuclei are located in the medulla. The pregan-glionic fibers from parasympathetic preganglionic neurons located in the nucleus ambiguus and dorsal motor nucleus of vagus exit the ventrolateral medulla through the vagus and synapse on the postganglionic neurons located in the heart. The postganglionic parasympathetic fibers innervate the sinoatrial node, atria, and atrioventricular node. The ventricles of the heart receive relatively little post-ganglionic parasympathetic innervation. Activation of the parasympathetic division of the autonomic nervous system results in a decrease in heart rate by decreasing the pacemaker activity of the sinoatrial node cells. The impulse conduction through the atrioventricular node and the contractile force of the ventricular muscle are decreased.
Lungs
Sympathetic Innervation
The sympathetic preganglionic neurons innervating the lungs are located in the IML at the T1—T4 spinal level. The sympathetic preganglionic fibers from these neurons synapse on T1—T4 ganglia in the sympathetic chain. Post-ganglionic fibers from these neurons innervate the smooth muscle of the bronchial tree (Fig. 22-5). Activation of the sympathetic nervous system results in bronchodilation.