Neurochemical Factors and Drug Treatments
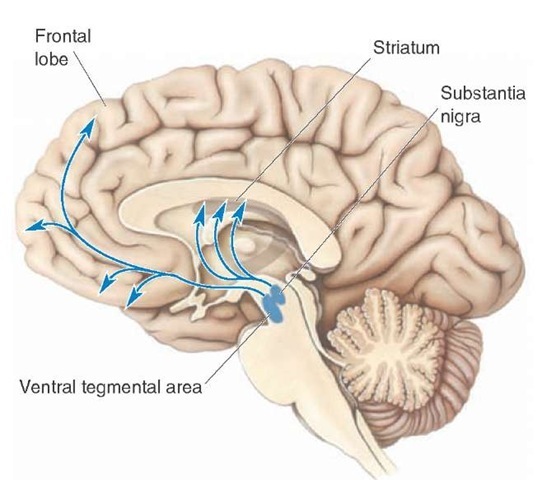
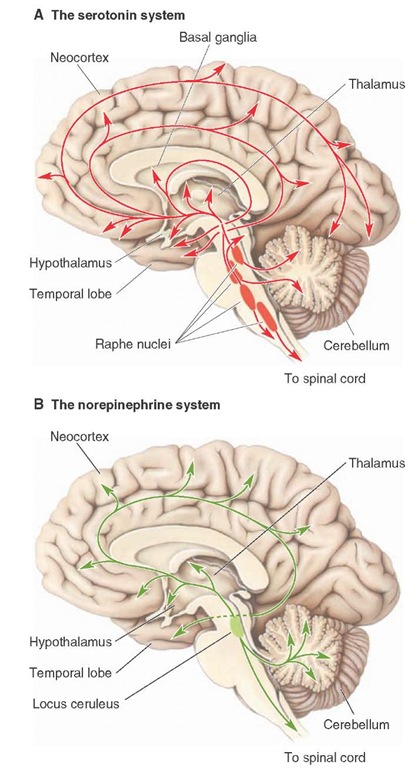
Based, in part, on the known ubiquitous projections of the monoamine neurons to the forebrain (Figs. 28-1 and 28-2), most studies have focused on the role of biogenic amines in the etiology of depression and other mood disorders. In fact, one of the longest running theories of depression has been the catecholamine hypothesis, which states that a deficiency in catecho-lamines causes depression and that mania results from an excess of catecholamines, especially at key synaptic regions of the brain. While this theory is generally not followed in its original form, it has generated considerable research. Later studies expanded on this hypothesis to include serotonin as well.
FIGURE 28-1 Dopaminergic pathways and depression. Schematic diagram indicating the distribution of the major dopaminergic pathways.
FIGURE 28-2 Serotonergic and noradrenergic pathways in depression. Schematic diagrams illustrating the distribution of the: (A) serotonergic pathways that arise from the raphe nuclei, and (B) noradrenergic pathways that arise from the nucleus locus ceruleus and other regions of the brainstem reticular formation. Both of these monoaminergic systems project to all parts of the central nervous system, but in particular, to the forebrain.
Dopamine
The arguments in support of the view that dopamine is involved in depressive disorders comes from several sources. First is the finding that reserpine, which causes depletion of stores of monoamines and which was originally used to treat schizophrenia and hypertension, produced depressive-like symptoms. However, neuroleptics, which are used to treat psychotic disorders and which are known to block dopamine receptors, do not appear to cause depression. Second, Parkinsonism, which involves depletion of dopamine, is sometimes associated with depression (although there may be other factors involved). Third, drugs that increase concentrations of dopamine, such as tyrosine and amphetamine, tend to reduce the symptoms of depression as well as induce hypomania, which was observed after administration of the metabolic precursor of dopamine, levodopa (L-DOPA). Likewise, dopamine antagonists have been effective in treating hypomania (as it relates to bipolar disorder).
Norepinephrine
With respect to norepinephrine, several of the arguments presented earlier for dopamine involvement would also implicate norepinephrine in depressive disorders because a number of the drugs that were used affected both dopamine and norepinephrine and others affected all of the monoam-ines. In addition, drugs, such as venlafaxine hydrochloride ([Effexor] a potent serotonin-norepinephrine reuptake inhibitor [SNRI]), have been shown to have antidepres-sant activity. Research studies have also shown a correlation between down-regulation of P-adrenergic receptors and antidepressant responses.
Serotonin
In recent years, considerable attention has been given to the role of serotonin in depressive disorders. Similar to dopamine and norepinephrine, serotonin has a ubiquitous distribution to wide areas of the forebrain, including regions normally associated with mood disorders. The most striking findings identifying serotonin as a key neurotransmitter involved in depression were the improved conditions of patients following administration of specific serotonin reuptake inhibitors for the treatment of this disorder. Examples of these drugs include fluoxetine (Prozac) and sertraline (Zoloft). There are several other classes of antidepressant drugs that affect serotonin concentrations or serotonin receptors. One class includes monoamine oxidase inhibitors, such as iproniazid, which maintain or increase serotonin (and other monoamine) levels and which have been shown to be effective anti-depressant drugs. Likewise, tricyclic compounds, such as amitriptyline, which also increase monoamine concentrations, help to diminish depressive states.
Other studies support a serotonin hypothesis of depression. These studies resulted in the observations that: (1) serotonin depletion has been correlated with the onset of depression; (2) in certain patients, low CSF levels of 5-hy-droxy-indoleacetic acid (5-HIAA) have been associated with suicide; and (3) there are changes in 5-HT1A and 5-HT2A receptors in the prefrontal cortex of suicide victims.
The Role of Lithium for Treatment of Bipolar Disorder
For approximately three decades, lithium has been used for the treatment of bipolar disorder.It reduces the intensity, recurrence, and length of the manic phase and has been reported to have positive effects on the depressive phase as well. However, a specific mechanism by which lithium produces its positive effects has yet to be elucidated. Nevertheless, research studies have revealed that lithium generates a variety of effects on neural tissue. Several of these include: (1) changes in G-protein expression, adenylyl cyclase, and monoamine receptors; (2) effects on release and uptake of catecholamines; and (3) effects on brain phosphoinositide systems. It has been suggested that these changes might form the basis of the positive effects obtained from lithium for treatment and prevention of mania and depression.
Neuroendocrine Function and Sleep
Patients with depressive disorders also experience neu-roendocrine and sleep dysfunctions, which, in turn, can have serious effects on their physical as well as mental health.
Concerning neuroendocrine function, significant changes in thyroid, reproductive, and adrenal hormonal activities have often been reported. Release of the anterior pituitary hormone, thyrotropin, and thyrotropin-releasing hormone in the hypothalamus are often reduced. For this reason, thyroid hormone treatment in patients with unipolar or bipolar disorder has been found to be helpful.
With respect to reproductive hormones, there is a decrease in the basal levels of follicle-stimulating hormone, luteinizing hormone, and testosterone (in males). Therefore, the adrenal androgen, dehydroepiandrosterone, might be helpful in treating depression in older men. It is possible that estrogen treatment may be effective for women suffering from premenstrual, menopausal, or post-partum depression.
An established finding has been the correlation between the time of occurrence of a major depression and hypersecretion of cortisol (which is released from the adrenal cortex by the pituitary hormone, adrenocortico-tropic hormone, which, in turn, is controlled by the par-aventricular nucleus of the hypothalamus). Postmortem examination of depressed patients have revealed higher levels of the corticotropin-releasing hormone (CRH) in the hypothalamus as well as elevated levels of cortisol in the urine and blood. These observations suggest that administration of inhibitors of CRH might reduce the symptoms of depression.
Sleep dysfunctions are also common in depressive disorders. Examples of sleep abnormalities include a shortened latency to rapid eye movement (REM) sleep,extended length of REM sleep, early morning awakening, delayed onset of sleep, and poor sleep efficiency.
Anxiety Disorders and Drug Treatments
Anxiety, a normal response to a real or perceived dangerous situation that is present in our lives daily, is generally a practical, useful, and adaptive reaction for an individual. However, when anxiety reactions occur in response to environmental or perceived stimuli that, objectively, should not evoke such reactions or when anxiety reactions are elevated to levels that disrupt behavior, anxiety is said to be maladaptive and, thus, constitutes a form of behavioral disorder. In fact, of all the psychiatric illnesses, anxiety reactions are the most common, and, additionally, they are symptoms in many other psychiatric disorders.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) lists different categories of anxiety disorders. Major categories of anxiety include panic attack, obsessive-compulsive disorder, posttraumatic stress disorder, and generalized anxiety disorder. A brief discussion of each of these disorders follows, together with their neurochemical correlates (where such information is available).
Panic Disorder
According to the DSM-IV classification, a panic attack is defined as a "discrete period of intense fear or discomfort." During an attack, which lasts for approximately 30 minutes or less, the patient typically exhibits symptoms such as shortness of breath, palpitations, sweating, trembling, and fear that he or she is going crazy or will die. Repeated episodes of panic attack are referred to as panic disorder. This disorder is sometimes accompanied by a condition called agoraphobia, which is a fear of leaving a familiar place. This kind of fear would require the patient to be escorted by a friend or family member into a crowded street or closed-in places such as a tunnel, elevator, or bridge.
From the results of various studies, there is some evidence suggesting that there may be a genetic component to this disorder. Such studies indicate that the risk of panic disorder is much higher if first-degree relatives have this disorder in contrast to first-degree relatives of patients with other psychiatric disorders. In addition, on the basis of twin studies, there is a higher concordance for panic disorder between monozygotic twins than dizygotic twins.
Panic attacks can be induced in some patients with this disorder by administering sodium lactate, a CCK agonist, or by inhaling carbon dioxide. Patients are also sensitive to caffeine and the a2-adrenergic receptor antagonist, yohimbine. In normal individuals, these substances are not effective in inducing panic attacks. The neurobiology of panic disorders remains poorly understood, and we have little knowledge of the specific brain regions that mediate this form of anxiety disorder.
Several approaches have been used in treating panic disorder. One approach has been the application of cognitive and other behavior therapies. This approach has met with success, and individuals receiving such therapy have had long-lasting remission of their symptoms. The other successful approach involves pharmacotherapy. Some reports suggest that the most effective approach has been to combine pharmacotherapy with cognitive or other behavior therapies. Concerning pharmacotherapy, the most effective drugs for the treatment of panic disorder are selective serotonin reuptake inhibitors (SSRIs). Although there have been wide, varying effects of these drugs, in general, agents such as paroxetine (Paxil), sertraline, and fluvoxamine (Luvox) have been used in recent years with considerable success.
Other classes of drugs have also been used with varying degrees of success. One class includes benzodiazepines, such as lorazepam (Ativan), which work rapidly against panic. Benzodiazepines are used as a first drug in the treatment of panic disorder; the drug is later replaced by a drug blocking serotonin reuptake. However, a problem with the long-term use of benzodiazepines is that they could lead to drug abuse, drug dependence, and cognitive impairment. Tricyclic anti-depressant drugs, such as clomipramine, and SSRIs, like paroxetine, have also been used successfully for the treatment of this disorder. Another class of drugs, the monoamine oxidase inhibitors (such as phenelzine [Nardil]), has also has been used but appears to require high doses to be effective.
Obsessive-Compulsive Disorder
The DSM-IV defines obsessive-compulsive disorder (OCD) as "recurring obsessions or compulsions that are sufficiently severe to be time consuming or cause impairment and distress." The obsession is a recurring sensation, thought, feeling, or idea that elevates anxiety levels; whereas the compulsion is a reaction that reduces anxiety levels (e.g., the need to wash ones’s hands after touching any object). Because these responses are so irrational and disproportionate to reality, OCD can be quite disabling and time consuming.
A number of brain imaging studies have been conducted to identify the possible brain regions associated with this disorder. Most, if not all, of the studies have identified the orbit-ofrontal cortex and adjoining regions of the dorsolateral and medial aspects of the prefrontal cortex as key areas (Fig. 28-3). Several other regions related to the orbitofrontal cortex, including the caudate nucleus (which receives many fibers from the prefrontal cortex), cingulate cortex, and parts of the dorsal thalamus, have also been linked with this disorder.
Neurochemical studies and clinical investigations have provided support for the view that serotonin plays some role in this disorder since serotonergic drugs have been more effective than other classes of drugs. In particular, the SSRI’s are effective in treating this disorder as is behavioral (conditioning) therapy. This would imply that dysregulation of the serotonin system in a "downward" direction contributes to the obsessive-compulsive disorder, and that psychotherapy may serve to readjust the levels of serotonin to normal values.
Posttraumatic Stress Disorder
The DSM-IV defines posttraumatic stress disorder (PTSD) as a group of symptoms that develop after an individual experiences an event that is potentially life-threatening. As a result of this traumatic experience,the individual displays fear and helplessness and tries not to be reminded of the event but relives it anyway. To be classified as PTSD, the patient’s symptoms must last for more than a month. The types of events that can produce this disorder are ones that would affect most people such as tornados, hurricanes, rape or other inappropriate sexual activity, war experience, assault, and very serious accidents. Although the patients re-experience the event in their thoughts and dreams, they do everything they can to prevent this from happening. As a result, the patient might display anxiety, depression, difficulties in cognitive functioning, hyperarousal, and reduced responsiveness.
FIGURE 28-3 Fluorodeoxyglucose positron emission tomography scans of representative patients in the horizontal plane at a mid level of the caudate nucleus before and after successful drug treatment of obsessive-compulsive disorder (OCD). Scans are processed to reflect the ratio of glucose metabolic rate registered by each pixel element, divided by that of the whole brain. OFC =orbital frontal cortex; L = left; R = right.
It has been suggested that a number of different neuro-transmitter systems might be associated with this disorder. However, drug studies have implicated, in particular, the noradrenergic system. For example, administration of cloni-dine or propranolol, which decreases noradrenergic transmission, is effective in reducing some of the symptoms of PTSD.