Central Auditory Pathways
The central auditory pathways are shown in Fig. 17-6. The central processes of bipolar neurons in the spiral ganglion form the cochlear nerve, which joins the vestibular nerve to form the vestibulocochlear nerve (cranial nerve VIII). The vestibulocochlear nerve passes through the internal auditory meatus, enters the posterior cranial fossa, and reaches the medullopontine angle of the brain-stem. Here the vestibulocochlear nerve splits into the vestibular and cochlear branches. Both branches enter the brainstem at the level of rostral medulla. The projections of the cochlear branch are described in the next section, and the projections of the vestibular branch are discussed later.
Cochlear Nuclei
The cochlear nerve contains central processes of bipolar neurons in the spiral ganglion. The spiral ganglion is located in the modiolus of the inner ear. The peripheral processes of the spiral ganglion bipolar neurons are connected to the hair cells in the organ of Corti. The axons in the cochlear nerve enter the medulla and project to dorsal and ventral cochlear nuclei located in the rostral medulla (Fig. 17-6). The axons of the cochlear nerve project to the cochlear nuclei in a tonotopic manner (i.e., the axons originating in the basal turns of the cochlea, mediating high-frequency sound, project to the deepest part of the nucleus, whereas the axons arising from the apical turns of the cochlea, mediating low-frequency sound, project to the superficial part of the nucleus). Some axons of the second-order neurons emerging from the dorsal cochlear nucleus located in the rostral medulla ascend to the pons and synapse on the ipsilateral superior olivary nucleus (not shown in Fig. 17-6). Other axons from the dorsal cochlear nucleus cross to the contralateral side in the tegmentum of the pons as dorsal acoustic stria and then ascend through the rostral pons and synapse on neurons in the inferior colliculus (located in caudal midbrain). Axons of both dorsal and ventral cochlear nuclei form the intermediate acoustic stria, which also cross to the contralateral side in the tegmentum of the pons, ascend through the rostral pons, and synapse on neurons in the inferior colliculus. Axons of the second-order neurons in the ventral cochlear nucleus form the ventral acoustic stria (trapezoid body), which cross to the contralateral side in the mid-pons and synapse in the superior olivary complex (i.e., the lateral and medial superior olivary nuclei and the nucleus of the trapezoid body). Some axons of the second-order neurons in the ventral cochlear nucleus synapse in the ipsilateral superior olivary complex in the mid-pons. The projections from the superior olivary nuclei are discussed in the next section.
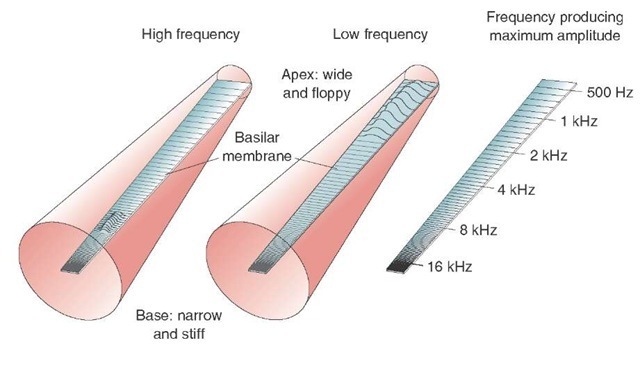
FIGURE 17-5 Topographical mapping of sound frequencies on the basilar membrane (tonot-opy). The cochlea is depicted as an uncoiled canal. The points responding to high frequencies of sound waves are located at the base of the basilar membrane, whereas those responding to low frequencies are located at the apex. Hz = Hertz.
FIGURE 17-6 Central auditory pathways. See text for details. CN = cranial nerve.
Superior Olivary Nuclei
The superior olivary nuclei on either side of the brain is tonotopically organized and receives bilateral auditory inputs from the cochlear nuclei. This nuclear complex can localize sound in acoustic space by discriminating the differences in the time of arrival of the sound or the differences in the intensity of sound to each ear.
Lateral Lemniscus and Associated Nuclei
Although the axons of the third-order neurons from the superior olivary complex and nucleus of the trapezoid body ascend bilaterally in the lateral lemniscus, a majority of these axons ascend in the contralateral lateral lem-niscus and project to the nucleus of the lateral lemniscus at the level of the pons-midbrain junction. The neurons in the nucleus of lateral lemniscus, in turn, project to the inferior colliculus (located in the caudal midbrain [Fig. 17-6]).
Inferior Colliculus
The dorsal portion of the inferior colliculus receives projections from neurons that are responding to low frequencies of sound, whereas the ventral portion receives projec tions from those neurons responding to high frequencies of sound. The auditory information is then processed and relayed by the inferior colliculus to the medial geniculate nucleus of the thalamus.
Medial Geniculate Nucleus
The medial geniculate nucleus of the thalamus is located in the caudal aspect of the thalamus and proximal to the midbrain. The axons of the inferior collicular neurons transmit auditory signals to the medial geniculate nucleus of the thalamus (Fig. 17-6). The medial geniculate nucleus, which is tonotopically arranged, relays precise information regarding the intensity, frequency, and binaural properties of the sound. The axons of these neurons, in turn, project to the primary auditory cortex.
Primary Auditory Cortex
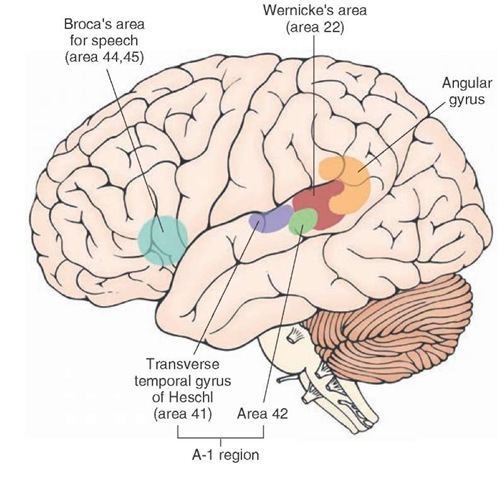
In humans, the primary auditory cortex is located in the transverse temporal gyri (of Heschl) of the medial aspect of the superior temporal gyrus (Fig. 17-7).Brodmann’s area 42 is the auditory association area. Together, Brodmann’s areas 41 and 42 are called the A-1 region and receive projections from the medial geniculate nucleus (geniculotemporal fibers or auditory radiations). The tonotopic organization in the auditory relay nuclei is maintained in the auditory cortex as well. One of the secondary auditory areas includes Wernicke’s area (Fig. 17-7), which is important for the interpretation of the spoken word.
Descending Pathways
The A-1 region in the cortex sends descending projections to the medial geniculate nucleus of the thalamus. The medial geniculate nucleus, in turn, sends projections to the inferior colliculus. Presumably, these descending projections provide neural feedback mechanisms within the central auditory pathways.
Other descending projections include olivocochlear efferent fibers. The axons of neurons located in the superior olivary nucleus form both the crossed and uncrossed olivocochlear bundle, travel in the cochlear nerve, and finally innervate the inner and outer hair cells of the cochlea. At the inner hair cells, uncrossed efferents make synaptic contacts with primary afferent fibers arising from bipolar neurons in the spiral (cochlear) ganglion, while crossed olivocochlear fibers enter the contralateral cochlear nerve and innervate the outer hair cells of the (contralateral) cochlea. The crossed, as well as uncrossed, olivocochlear efferent innervation regulates the function of hair cells by a mechanism not completely understood and modulates auditory sensitivity. The excitatory transmitters released by some of these efferents are believed to be acetylcholine, glutamate, and aspartate, whereas y-aminobutyric acid (GABA) is believed to be an inhibitory transmitter released by some efferent fibers.
FIGURE 17-7 Primary auditory cortex. This area is located in the transverse temporal gyri (Heschl) of the medial aspect of the superior temporal gyrus. It receives projections from the medial geniculate nucleus (geniculotemporal fibers or auditory radiations). The secondary auditory area (Wernicke’s area) is important for the interpretation of the spoken word. Other areas are shown for orientation purposes.
Clinical Disorders Associated With the Auditory System
Conduction Deafness
Otosclerosis is a condition in which the bony outgrowth of the stapes impedes its movement against the oval window. Thus, the ability for efficient conversion of airborne sound waves to pressure waves in the perilymph is lost. This type of conduction deafness is currently corrected by a microsurgical procedure called stapedectomy. The procedure involves removing the stapes and substituting it with a prosthetic device (usually a nonmagnetic metallic wire of appropriate thickness and length). Conduction deafness can also result from chronic infection of the middle ear accompanied by fluid accumulation in the middle ear (otitis media); reduced movement of middle ear ossicles has been implicated in this condition.
Sensorineural Deafness
Pathological lesions in the cochlea, cochlear nerve, or central auditory pathways can result in sensorineural deafness. Lesions of the cochlea, cochlear nerve, or cochlear nuclei elicit deafness in the ipsilateral ear. Lesions present in higher auditory nuclei may attenuate hearing; however, because of the multiple synapses and crossing and recross-ing within the auditory pathways, complete deafness does not occur.
Hearing Tests
Two simple hearing tests, Weber’s test and Rinne’s test, are often used in an office setting. In Weber’s test, the base of a vibrating tuning fork is placed at the top of the head in the midline. If the person’s deafness is due to conduction disturbance in the right ear, the sound from a vibrating tuning fork will be heard louder in the same (right) ear. If the person’s deafness is due to sensorineural loss in the right ear, the sound will be louder in the left ear. Rinne’s test compares hearing by air conduction versus bone conduction. A vibrating tuning fork is held in the air near the affected ear, and then the base of the tuning fork is placed on the skull (usually at the mastoid process). If the sound perceived by the patient is louder when the tuning fork is placed on the mastoid process, when compared to the sound of the tuning fork held in the air, the patient is diagnosed as suffering from conductive hearing loss. If the sound perceived by the patient is louder when the tuning fork is placed in the air near the affected ear, the patient is diagnosed as suffering from sensorineural hearing loss.
Conductive hearing loss can be effectively treated by surgery (see earlier section, "Conduction Deafness"). On the other hand, sensorineural hearing loss is difficult to treat. However, during the last decade, considerable progress has been made in treating this hearing loss with cochlear implants.
Tinnitus
Tinnitus is characterized by a "ringing" noise in the ears. Its pathophysiology is not clearly understood. It is believed that damage to the cochlear and vestibular end-organs is responsible for the ringing noise in the ears. Some drugs (e.g., salicylates) induce tinnitus in toxic doses.
Vestibular System
Anatomical Components
The vestibular system is essential for maintaining the position of the body in space, which, in turn, is important for coordination of motor responses, eye movements, and posture. It consists of the following anatomical components: saccule, utricle, and three semicircular canals (anterior or superior, posterior and lateral, or horizontal semicircular canals). The saccule and utricle (called oto-lith organs) detect linear acceleration, while the semicircular canals detect angular acceleration (Fig. 17-8).
Saccule
The saccule is an ovoid sac-like structure that is connected to the cochlea (through the canal reuniens) and to the utricle (through the utriculosaccular duct). One of the branches of the latter duct (the endolymphatic duct) travels through the petrous bone and forms the endolym-phatic (otic) sac in the cranium between the layers of the dura; the endolymphatic sac may be the site where endol-ymph is absorbed (Fig. 17-2). A small area containing hair cells and supporting cells is located within the saccule and constitutes the sensory organ of the saccule. This sensory organ is called the macula of the saccule. A similar area present in the utricle is called the macula of the utricle. There are two types of hair cells in the vestibular labyrinth (including those in the maculae of the saccule and utricle and ampullae of the semicircular canals). These include type I and type II hair cells (see "Vestibular Sensory Receptors"). Projecting from the hair cells are the cilia, which are embedded in a gelatinous matrix of the otolithic membrane containing otoliths (calcium carbonate crystals [Fig. 17-9]).
Utricle
The utricle is also an ovoid sac-like structure; the cavity inside is the largest in the vestibular labyrinth (Fig. 17-8). Its sensory organ, the macula of the utricle, is located in the anterolateral wall of the cavity, and the organization of its hair cells, cilia, and otolithic membrane is similar to that of the macula of the saccule. The macula of the sac-cule is almost at a right angle to the macula of the utricle. When the head is in an upright position, the macula of the utricle is in the horizontal plane, while the macula of the saccule is in the vertical sagittal plane.
FIGURE 17-8 The vestibular system. Note the location of the saccule, utricle, and three semicircular canals.
FIGURE 17-9 Otolithic membrane. Note that the cilia from the hair cells are embedded in a gelatinous matrix of the otolithic membrane containing otoliths that are composed of calcium carbonate crystals.
Semicircular Canals
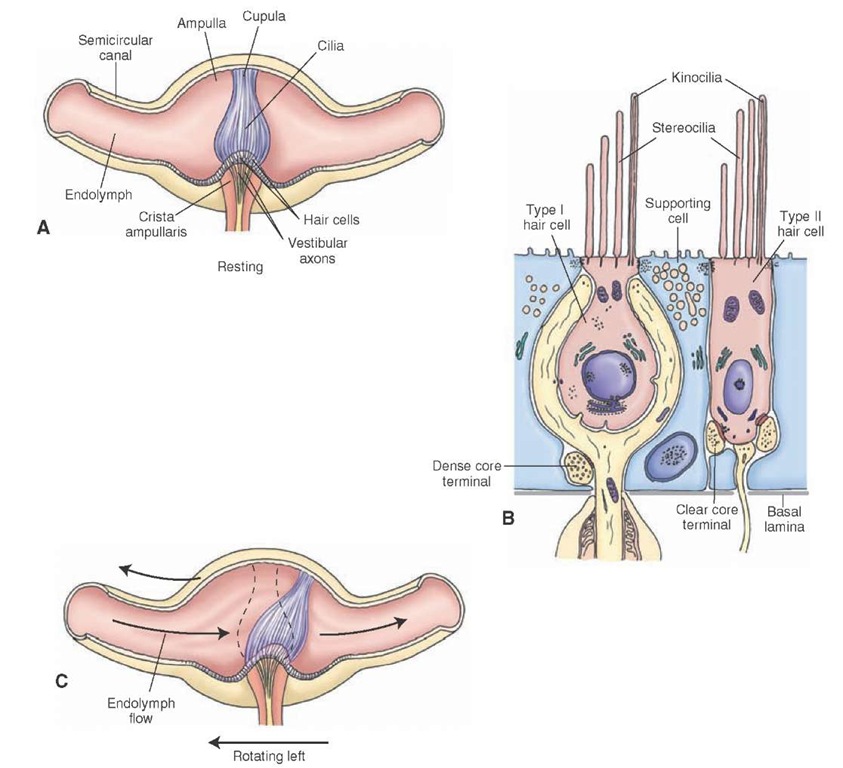
There are three semicircular canals (anterior or superior, posterior, and lateral or horizontal) that lie in different planes and are perpendicular to each other (Fig. 17-8). Each of these canals is continuous with the utricle at each end. One of these ends is dilated, and this dilation is called the ampulla. Inside the ampulla, a cone-shaped structure called the crista ampullaris, projects at a right angle to the long axis of the canal (Fig. 17-10A). The receptor cells (hair cells) and supporting cells are located in the crista ampullaris. A gelatinous mass (the cupula) extends from the surface of the hair cells to the roof of the ampulla. The cilia of the hair cells are embedded in the cupula (Fig. 17-10A).
Vestibular Sensory Receptors
The receptors in the vestibular system (maculae of saccule and utricle and ampullae of semicircular canals) are the hair cells. The hair cells of the vestibular system are of two types (type I and type II) (Fig. 17-10B). Recall that the two types of sensory receptors in the cochlea are called "inner hair cells" and "outer hair cells." In the vestibular system, the type I hair cells are goblet shaped, and the type II hair cells are cylindrical in shape. Stereocilia in large numbers project from the apical surfaces of all hair cells. A single kinocilium is present at the edge of the apical surface.
FIGURE 17-10 The ampulla. (A) Inside the ampulla is a crest (the crista ampullaris) on which hair and supporting cells of the crista are located. A gelatinous mass (the cupula) extends from the surface of the hair cells to the roof of the ampulla; cilia of the hair cells are embedded there. (B) Type I hair cells are goblet shaped, and type II hair cells are cylindrical. Note the stereocilia projecting from the apical surfaces of all hair cells and a single kinocilium at the edge of the apical surface. (C) Displacement of the cupula in the direction of the utricle results in excitation of the hair cell, whereas displacement of the cupula in the reverse direction results in inhibition of the hair cell.
The stereocilia are relatively shorter than the kinocilium, and their length increases as they approach the kinocilium. The hair cells are surrounded by supporting cells. Tight junctions are present between the hair cells and the supporting cells; this anatomic feature isolates the body of the hair cell from the endolymph, which surrounds the cilia. When the stereocilia are displaced toward the kinocilium, the hair cell is excited. When the stereocilia are displaced away from the kinocilium, the hair cell is inhibited. In the ampullae of the semicircular canals, when the head turns in the plane of one of the semicircular canals, the inertia of the endolymph generates a force across the cupula, moving it away from the direction of head movement, which results in a displacement of the hair cells within the crista (Fig. 17-10C). Displacement of the stereocilia present on the hair cells induces either depolarization or hyperpolari-zation of the hair cell; displacement of the cupula in the direction of the utricle results in excitation of the hair cell, whereas displacement of the cupula in the reverse direction results in inhibition of the hair cell. In the maculae of the utricle and saccule, linear acceleration or deceleration causes movement of the otolithic membrane and the cilia embedded in it. This displacement causes depolarization or hyperpolarization of the hair cell. The patterns of excitation and inhibition of hair cells are processed by the central pathways and interpreted by neurons in the cerebellar and cerebral cortices for the sense of balance (equilibrium).
The mechanical movement of the cilia results in the depolarization or hyperpolarization of a vestibular hair cell, involves the influx of ions (K+ and Ca2+), and is identical to the mechanism already described for the auditory system (see "Mechanism of Sound Conduction").