Other causes of post-operative airway obstruction
There have been several reports of airway obstruction following craniocervical fixation, which appear to have been the result of fixation in excessive flexion.
Rheumatoid arthritis patients are at particular risk of post-operative airway obstruction because of exacerbation of cricoarytenoid arthritis by intubation. he smallest possible diameter tube should be used. Emergency reintubation for airway obstruction due to acute sialadenitis after prolonged surgery has been reported.
Unilateral laryngeal nerve damage occurs after anterior cervical surgery, but this does not cause airway obstruction. It is often asymptomatic, although patients may have a lowing cough and a weak voice. One prospective study found an incidence of 11.3%, diagnosed by laryngoscopy.
Major blood loss
Serious blood loss is a feature of some spinal procedures, notably scoliosis correction and tumour surgery (Fig. 15.7). Pre-operative radiological embol-ization of tumours can reduce operative bleeding. Facilities and portals for rapid blood infusion should always be available. Close cooperation with haemato-logical colleagues is crucial so that blood products (red cells, platelets, fresh frozen plasma and factor concentrates) can be made available promptly. After four unit transfusion replacement with red cells, fresh frozen plasma and platelets should be in the ratio of 1:1:1.
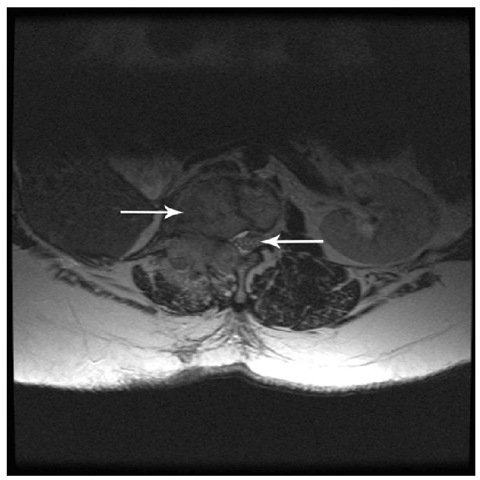
Fig. 15.7. MRI scan showing a tumour deposit invading the lumbar spine. The left arrow points to the tumour and the right to thecauda equina.
The most dramatic example of major blood loss associated with spinal surgery is damage to the aorta or inferior vena cava during lumbar discectomy. Surgeons are usually unaware that their rongeurs have perforated the great vessels because bleeding does not appear in the wound. Circulatory collapse is usually the first sign and mortality is very high. Damage to the iliac vessels can also occur, but the bleeding is usually less acute and the mortality rate correspondingly lower.
Monitoring the circulation is more difficult when the patient is prone. Central venous pressure monitoring is less accurate than in the supine position, but it nevertheless provides a useful trend to guide fluid management and the need for vasopressors. Cardiac output monitoring is increasingly practised, although oesophageal Doppler techniques are inconvenient when the patient is prone.
Aprotinin has been withdrawn, but tranexamic acid has been shown to reduce blood loss after spinal surgery. Induced hypotension does reduce blood loss and is controversial because of the risk of reduced spinal cord perfusion and concerns about its association with POVL. Hypotension may also cause an increased risk of post-operative cognitive impairment in elderly patients after spine surgery.
Minimizing the risk of perioperative spinal cord damage
Unsurprisingly, patients at greatest risk of periopera-tive SCI are those undergoing multilevel surgery with instrumentation as well as those with an established pre-operative myelopathy. It is important to realize that perioperative SCI is not conf ned to the cervical region but also occurs in the thoracic and lumbar (cauda equina) segments.
Airway management
The concept that airway management, and direct laryngoscopy in particular, is a cause of SCI has been described as a ‘legend of anaesthesia’. here are many reports of SCI below the cervical level and the author of course does not attempt to implicate airway management as causative. However, when an SCI occurs in the cervical region, attention nearly always focuses on airway management and therefore on the anaesthetist. his may simply be an example of confusion between subsequence and consequence, as airway management is inevitably followed by alternative causations, such as prolonged minor malposition or inadequate spinal cord perfusion pressure.
There is neither a case report that unequivocally implicates airway management in the genesis of SCI nor any evidence of outcome difference with one airway management technique over another. However, absence of evidence does not prove that the phenomenon does not exist. In two studies of the effect of airway management in cadavers rendered grossly unstable, basic life support techniques (head tilt, jaw thrust) produced more disturbance at the unstable cervical spine sites than direct laryngoscopy. If this is true in vivo, it might be an argument for ‘awake’ intubation in patients with unstable necks. However, the quantity of vertebral displacement or angulation that occurs in a truly unstable spine during ‘awake’ intubation is not known, and might in fact be greater than during intubation under general anaesthesia. Surveys of anaesthetists have indicated that ‘awake’ flexible fibre-optic intubation is perceived as a good option in patients with suspected cervical instability, but the procedure is by no means always straightforward and has resulted in laryngeal damage and even complete airway obstruction necessitating an emergency surgical airway. In this author’s view, it would not be in a patient’s interests for an anaesthetist inexperienced in ‘awake’ endoscopy to attempt an ‘awake’ intubation on the grounds of suspected or actual cervical instability.
Laryngoscopy
Whether or not videolaryngoscopy is clinically superior to direct laryngoscopy is unknown. One study found no significant difference in cervical spine movement between GlideScope* videolaryngoscopy and direct laryngoscopy, despite not using the tactic of only exposing the glottis sufficiently to allow the introduction of a gum-elastic bougie. Nevertheless, videolaryn-goscopy probably makes some intubations easier and it is of interest, irrespective of neurological considerations. Despite recent innovations, direct laryngoscopy with the Macintosh laryngoscope remains an accepted method of intubation for anaesthetists and emergency physicians.
Awake positioning
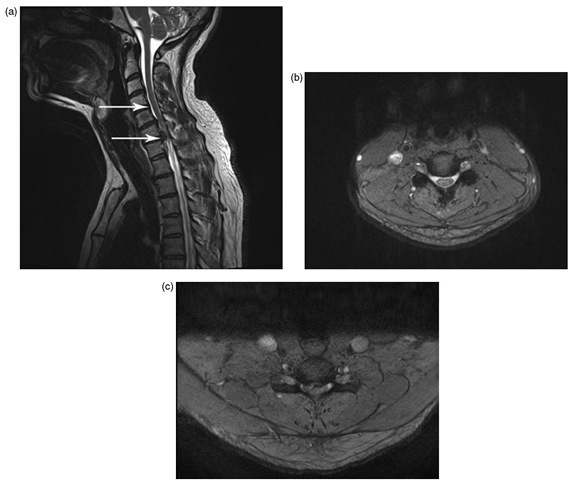
Prolonged abnormal spine positioning carries a small risk of neuraxial damage, even in patients with normal spines, and this risk is compounded in those with spinal disease. Te majority of reports of SCI during anaesthesia have involved patients with spinal canal stenosis (Fig. 15.8), not instability.
It is not possible to predict whether a particular position will be tolerable for the duration of surgery. Spinal cord monitoring techniques offer a potential guide to positional adequacy (see below), but ‘awake’ positioning has been suggested as an alternative. However, position-related SCI can still occur with awake positioning techniques because not even the patient can predict whether a position will still be tolerable some hours later. If awake positioning is undertaken, consideration must be given to where the dividing line between sedation and anaesthesia is to be drawn. In practice, this is not always clear cut and what is intended to be sedation can more closely resemble anaesthesia. Disinhibition and withdrawal of cooperation are possible, although unusual if the patient is properly prepared. In addition, some thought should be given to what action will be taken if a problem is suspected, as false positives have been described during awake positioning and the patient may not benefit from postponement of surgery.
Spinal cord monitoring
Sensory and motor evoked potentials have not been proved to improve outcome during spine surgery and both false-positive and false-negative results can occur. Sensory potentials have poorer sensitivity (52%) but higher specificity (100%) than motor potentials (100 and 96%, respectively) for cord damage. As evoked potentials are sensitive to hypotension, they also offer some guide to what level of blood pressure can be tolerated during surgery. For both sensory and motor evoked potentials, the best results are gained with pro-pofol infusion, although sensory recordings can be elicited in the presence of low doses of volatile agents. Motor potentials are abolished by volatile agents and muscle-relaxant drugs, so propofol and remifentanil infusions are the most convenient anaesthetic technique.
Blood pressure management
There is a tension between the possible improvement in operating conditions and reduction in blood loss obtainable with induced hypotension and reductions in spinal cord and optic nerve perfusion. Hypotension should be avoided if possible in all patients with known spinal cord compression. Unimpaired evoked potentials are reassuring in terms of the adequacy of spinal perfusion, although false negatives can occur. Infusions of vasoconstrictors such as metaraminol or phenylephrine are often necessary to maintain adequate blood pressure during prolonged spine surgery.
Fig. 15.8. T2-weighted MRI scans showing spinal stenosis. (a) Sagittal image with the upper arrow at a normal level and the lower arrow at an abnormal level. The abnormality could be disc or osteophyte. (b) Axial image showing a normal area where the cord is surrounded by cerebrospinal fluid (white) (upper arrow on the sagittal section). (c) Axial image showing an area of spinal stenosis causing cord compression (lower arrow on the sagittal section).
Post-operative spinal haematoma
Age >60 years, pre-operative non-steroidal use, Rh-positive blood type, procedures involving more than f ve spinal levels, a haemoglobin falling to less that 10 g dl-1, blood loss >1 l and, in the post-operative period, an international normalized ratio (INR) of >2 are independent associations with post-operative spinal haematoma.
Post-operative pain
Pain after spinal surgery can be severe and debilitating, and a multimodal approach to pain management is essential. Possible drugs include paracetamol, non-ster-oidal drugs, subanaesthetic doses of ketamine (0.5 mg kg-1 followed by 4 ^g kg-1 min-1), clonidine, dexametha-sone, gabapentin, pregabalin and opioids. here has been concern that the use of non-steroidal drugs may inhibit bony fusion after spinal surgery, but current evidence suggests that treatment for 48 h is safe.
Epidural analgesia can be very effective, although pre-operative catheter placement can be difficult if the anatomy is abnormal. Intraoperative placement by the surgeon sounds simple, but, in practice, misplacement and failure occur relatively frequently. Staff education is important to avoid confusion between the effects of epidural local anaesthetic on motor power and complications such as intraspinal haematoma and intracranial spread of anaesthetic because of subdural catheter placement (note that intracranial spread does not occur with epidural placement, as the dura is inserted onto the foramen magnum). Epidural clonidine infusion has been shown to be effective and may avoid the possibility of staff attributing myelopathic symptoms to local anaesthetic effects.
Post-operative visual loss
The overall incidence of POVL after spine surgery is low, but, when it occurs, it is devastating for the patient. A retrospective study of all spine surgery in the USA found an overall incidence of 0.09%, with spine surgery for scoliosis correction having the highest rate (0.28%). Nearly all cases occur after the prone position and, curiously, it is common for patients not to report POVL immediately, possibly because they presume that the loss is a temporary peri-anaesthetic phenomenon.
Ophthalmological diagnoses
There are several causes of POVL:
1. Ischaemic optic neuropathy (ION). his can be posterior when the optic nerve is damaged proximal to the eye, or anterior when the nerve is damaged as it enters the eye. Ischaemic optic neuropathy presents as painless, often bilateral, visual loss. he external appearances of both eyes are similar, although facial swelling is common after prolonged prone positioning. he retinal appearances can be normal in posterior ION, although the disc is swollen and there may be flame-shaped haemorrhages in anterior ION.
2. Central retinal artery occlusion (CRAO). his is usually unilateral and presents with signs of external pressure with a swollen, proptosed eye, sometimes with ophthalmoplegia. Surprisingly, pain is not mentioned in published reports. he characteristic retinal appearances are ‘cloudy swelling’ due to retinal oedema, retinal pallor and a cherry-red spot at the fovea caused by well- perfused sclera shining through the thinnest point of the retina.
3. Non-ION,non-CRAO visual loss.
4. Cortical blindness. his occurs due to damage to the visual cortex and is rare.
Causation
Central retinal artery occlusion is the rarest form of POVL and is often caused by external pressure on the eye. It can also be related to embolic obstruction in which case there are no external signs of pressure damage. he majority of reports of CRAO have involved the use of a horseshoe type of head rest, although it has been described with most types of head support apart from head-pin fixation.
The causation of ION and non-ION, non-CRAO visual loss remains uncertain, although these conditions might represent a form of compartment syndrome of the orbit. A striking finding of the American Society of Anesthesiologists’ analysis of POVL was that the mean period in the prone position was 9.8 ± 3.1 h in 94% of cases of ION. Orbital swelling and increased intraocular pressure is common after even short periods in the prone position, and it is not difficult to imagine how the optic nerve can be compressed by oedematous and engorged orbital contents. he risk of ION is increased with prone position, age > 65 years, male sex, diabetes, hypotension, anaemia and duration of surgery. Patients who develop non-ION, non- CRAO visual loss are more likely to be hypertensive, have peripheral vascular disease and to have had a blood transfusion.
Prevention
It has been suggested that avoiding pressure on the eye, applying 10° of reverse Trendelenburg tilt during prone surgery, maintaining arterial pressure near the patient’s baseline, avoiding large amounts of crystalloid infusion, keeping the haematocrit above 30 and staging surgery so that duration does not exceed 8 h might minimize the risk of POVL after spine surgery. An instructive account of a case of POVL can be found at http://www.rmf.harvard.edu/case-studies/ specialty-reference/anesthesia/blindness-following-spine-surgery.aspx.
Preventing pressure on the eye
The most certain method of preventing pressure on the eye is to use a skull pin fixation device. However, this requires a skilled operator, as inadequate fixation, perforation of the skull and perforation of an eye have all been reported. Devices that allow inspection of the eye, such as the Prone View, during surgery in the prone position are attractive (Fig. 15.9). A high index of suspicion, amounting to virtual obsession, is required throughout surgery. Te status of the eyes should be checked at regular intervals, although this is not always possible in practice and a safe frequency of checking is not agreed. A check should always be made if the position of the patient or table is changed.
Fig. 15.9. An example of a mirror system that allows inspection of the eyes and nose during surgery in the prone position.
Consent
The risk of POVL is not an issue that should be sprung on a patient on the day of surgery. In high-risk cases, a discussion must take place prior to admission to hospital.