Causation
Operations on the spine carry a risk of SCI, which increases with the complexity of the surgery and/ or if a myelopathy is present pre-operatively. Spinal cord injury can also occur during non-spinal operations, presumably due to a combination of relative malposition and hypotension, although many patients are subsequently found to have a pre-existing but undiagnosed spinal abnormality such as canal stenosis. Spinal cord injury has also been described in conscious individuals with normal spines who have adopted, or been forced to adopt, an abnormal posture.
Trauma is the major cause of non-operative SCI and, although vertebral fracture or dislocation is frequently present, SCI can occur when there is no radiographic abnormality (spinal cord injury without radiographic abnormality – SCIWORA).
Demographics and associations
Youth, male sex and alcohol or drug intoxication are important risk factors for SCI, but there is also an association with falls in the elderly. here is a strong association between severe head or facial injury and SCI and, unsurprisingly, between the finding of a focal neurological deficit and SCI.
Autonomic consequences
Impairment and imbalance between sympathetic and parasympathetic supply (autonomic dysreflexia) can result in cardiovascular instability. Hypotension and bradycardia are common (but not invariable) in the acute phase and are often described as ‘spinal shock. Postural hypotension and instability of blood pressure can be a persistent problem. Autonomic dysre-flexia can also cause dangerous hypertensive crises, often related to urological manipulation in patients with lesions above T6. Treatment is postural (sit the patient up), pharmacological (captopril or nifedipine) or anaesthetic (sevoflurane or isoflurane). Neuraxial block is an effective prophylactic measure during ‘at-risk’ procedures.
Prevention of secondary cord injury
Prevention of secondary SCI in the perioperative period is multifactorial.
Prevention of hypoxia
Hypoxia must be prevented. Possible aggravations of SCI by airway management manoeuvres are of secondary importance compared with the primacy of maintaining oxygen supply to a damaged cord. No method of intubation has been shown to be associated with improved outcome over another.
Spinal cord perfusion
Spinal cord perfusion must be maintained and a mean blood pressure of 85 mmHg has been recommended during the first week after SCI. Vasoconstrictor drugs may be needed to maintain perfusion pressure. Hypertension may be inappropriate because, in experimental models, cord swelling after trauma can be aggravated by severe hypertension. Fluid overload may also aggravate cord swelling and hypertonic (5%) saline has shown promising results in experimental reduction of cord swelling after trauma. Hyperglycaemia and hypo-glycaemia should be avoided.
Immobilization
After suspected spinal injury, immobilization is a standard. While the concept does seem a priori to be sensible, it is also certain that it brings hazards. Immobilization methods may force the patient into a position they would not voluntarily adopt and cause ischaemic pain and tissue damage over pressure points. Cervical collars can increase intracranial pressure and contribute to airway obstruction in patients with obtunded consciousness. A Cochrane analysis found no evidence of improved outcome, and one study found a worse outcome in patients who were immobilized after blunt cervical injury. Manual in-line stabilization (MILS) is recommended during airway management, but there is no evidence that it is associated with improved outcome. As with cricoid pressure, MILS should be adjusted or released if necessary to achieve adequate ventilation.
Detection of injury
Observational studies have found late neurological impairment in patients without an early diagnosis of spinal injury. However, it is also accepted that a proportion (about 5%) of patients with a spinal injury will suffer a neurological deterioration despite all care. his can occur hours to weeks after the initial injury and is then called subacute, post-traumatic ascending myelopathy. he reasons for this are uncertain, but vertebral artery damage is common. his uncomfortable fact should be borne in mind whenever a patient with a history of a spinal injury requires anaesthesia.
Clearing the cervical spine
Twenty-five to 50% of patients with a traumatic cervical spine injury have an associated head injury, so the need to confirm or exclude cervical injury in an unconscious patient is a common problem. here is local variation in practice but Table 15.3 summarizes the current recommendations in the UK. Some units dispense with plain films if the helical CT scan is satisfactory. MRI is required if there is focal neurological impairment, but the dangers inherent in transfer of a critically ill patient to an MRI scanner almost certainly exceed any benefit in patients with normal movement and a clear CT scan .
Table 15.3 Criteria for confirming cervical spine stability following cervical trauma
|
Conscious patient |
Unconscious patient |
|
Alert, no distracting injuries |
Plain radiographs are inadequate |
|
No midline pain |
The combination of plain films and CT scan is adequate to diagnose bony injury and ligamentous instability |
|
Normal movement |
|
|
No neurological deficit |
|
|
MR scans are not required for the exclusion of instability |
Pharmacological methods
High-dose methylprednisolone is controversial after SCI and is less used than previously. Many practitioners believe that convincing evidence of benefit that justifies an increased risk of infection, hyperglycaemia and psychosis is lacking.Magnesium is successful in experimental models but at doses that would not be tolerable in vivo.
Hypothermia
The debate about the possible benefit of ‘moderate’ (33°C) hypothermia after SCI continues. he advent of efficient intravascular cooling devices makes hypothermia an achievable goal, but whether any benefit exceeds the disadvantages of the intervention remains uncertain. As with traumatic brain injury, hyperther-mia should be avoided .
Pre-operative assessment
There are specific issues that should be considered during the pre-operative assessment of patients undergoing spinal surgery.
Urgency
Few spinal cases can be classified as emergencies, although there are notable exceptions such as acute myelopathies or cauda equina syndromes due to haematomas or disc protrusions, and airway obstruction due to tissue swelling/haematoma after cervical spinal surgery.
Haemostatic function
Drugs that affect platelet function should be stopped if possible prior to spinal surgery. Aspirin or clopidog-rel should be discontinued 7-10 days prior to surgery and non-steroidal anti-inflammatory drugs (NSAIDs) 48 h before. In emergency situations, it might be necessary to transfuse platelets. However, it is now clear that platelet inhibition is not always present in patients who are taking anti-platelet medication, and tests of platelet function that are entering clinical practice may distinguish those who need platelet supplementation from those who do not.
Assessment of symptoms and signs
It is wise to obtain the patient’s description of laterality and, for comparison with post-operative observations, to assess and document motor power in the limbs using the MRC scale. Paresis suggests that a myelopathy or cauda equina lesion is present and that there might be denervation changes at the neuromuscular junction. Under such circumstances, suxamethonium should only be used if absolutely necessary.
Blood pressure
The patient’s usual blood pressure should be ascertained and used to inform intraoperative-level blood pressure control. hose with suspect cord perfusion, such as patients with spinal stenosis, should not be allowed to be persistently hypotensive. here is recent evidence that elderly hypertensive patients may be at risk of a decline in neurocognitive function after spine surgery.
Post-operative ventilation
Some types of spinal surgery require overnight intubation or tracheostomy (see below) and patients with high-level myelopathy may require longer-term ventilatory support in the post-operative period.
Nutrition
Patients with a pre-operative swallowing difficulty or those who are likely to have prolonged difficulty swallowing post-operatively should be considered for a percutaneous endoscopic gastrostomy, as prolonged nasogastric intubation is associated with sinus infection. If a nasogastric tube is required in a patient who needs an awake intubation, it is sensible to pass it prior to intubation because it can be difficult and traumatic to intubate the stomach with a tracheal tube in place.
Airway assessment
The probability of serious airway difficulty is generally obvious from the end of the bed, but the following issues should also be considered when trying to predict difficult intubation:
• Conditions such as rheumatoid arthritis, ankylosing spondylitis, or iatrogenic problems such as halo-body or other cervical fixators, are well-known causes of difficulty and often necessitate special techniques such as awake intubation.
• Patients with disease of the craniocervical junction have a much higher prevalence of difficult laryngoscopy than those with disease below C3. It is generally difficult to identify restricted craniocervical movement by clinical examination of neck movement because of compensatory increased movement at lower cervical levels.
• Accurate prediction of airway difficulty in patients without ‘end-of-the-bed’ abnormality remains elusive. It is unlikely that a solution will be found, as the problem is essentially one of low prevalence. Unless a test can be devised that has nearly 100% specificity (negativity in health), even an extremely sensitive (positive in disease) test will result in an unacceptably high proportion of false-positive results if the prevalence is low.
• Tie Mallampati examination remains the most successful predictor of difficult direct laryngoscopy. Although its post-test probability is low (10-15%) when applied to a low-prevalence population (5%), this rises to around 50% in high-prevalence populations such as patients with rheumatoid arthritis. Te relative success of the Mallampati score in spinal patients probably reflects the consequence of restricted mouth opening due to craniocervical stiffness.
• A combination of the Mallampati score and a thyromental distance of <6 cm has a likelihood ratio of about 9, which, while not suitable for screening, does offer some predictive power (pre-test probability x likelihood ratio = post-test probability) .
• Poor separation of the posterior elements of the occiput, atlas and axis on lateral radiographs (the atlanto-occipital and atlanto-axial ‘gaps’ in Fig. 15.3) suggests poor craniocervical movement and is more predictive of difficult laryngoscopy than clinical tests .
• Although the advent of videolaryngoscopes means that it is nearly always possible to obtain a good view of the glottis, achieving intubation may still be difficult. It is not yet certain that alternatives to the combination of a Macintosh laryngoscope and a gum-elastic bougie represent a meaningful improvement over other, more complex, techniques .
Patient positioning
Careful patient positioning is crucial to maximize surgical access and prevent intraoperative nerve damage. Te fact that the spinal cord descends to about L1/2 and is intolerant of retraction means that surgery on cervical and thoracic lesions anterior to the cord is conducted in the supine or lateral position. However, posterior decompressive and stabilizing procedures at these levels are performed in the prone position. Te cauda equina is more tolerant of retraction, so that lumbar discs can be approached using the prone position . T e sitting position is rarely used during spine surgery, but the increasing prevalence of gross obesity may re-popularize this position.
Damage to the ulnar nerve at the elbow is a serious complication. Pain and disability can be long-lasting, with 50% of affected patients having symptoms at 3 months, and some a year later. Perioperative ulnar nerve monitoring has demonstrated that conduction becomes abnormal in up to 6% of cases. Ulnar nerve damage is more common in male patients and those with extremes of body habitus. No position has been identified as being either safe or dangerous in this respect.
Patients with anterior AAS require a system that allows the head to move posteriorly while the upper cervical spine (C2 and below) is supported. A large doughnut ring is ideal in the supine position.
Hazards of the prone position
There are well-recognized hazards of the prone position.
Damage to the eyes and face
It is usually impossible to inspect the eyes and nose if surgery is performed above the lumbar region in the prone position, even with mirror systems such as the Prone View. Pressure damage can occur rapidly and serious consideration should be given to using a Mayfield skull pin fixation system to the skull so that the eyes and nose are not compressed. he nose is particularly vulnerable to pressure-induced ischaemic damage.
Serious eye damage can result from injury to the cornea due to drying (exposure keratopathy) if the eye is not properly taped shut. he eyes must also be protected from blood and cleaning fluids. he problem of post-operative visual loss (POVL) is discussed in detail later in this topic.
Compression of the abdomen
Abdominal compression can result in both increased venous pressure and blood loss, and reduced ventila-tory compliance. Hepatic ischaemia due to prolonged abdominal compression has also been described and has been the subject of an investigation by the National Patient Safety Agency in the UK.
Cardiovascular problems
These are unusual unless the abdomen is compressed, when the effect varies with the type of positioning system used. Cardiac massage can be performed in the prone position but is less efficient.
Regional anaesthesia
Lumbar surgery, particularly microdiscectomy, can be performed with intrathecal anaesthesia, although the block may recede if the dura is breached. Caution should be observed in attempting to insert an epidural catheter in a patient with spinal stenosis or a history of spinal surgery. Neuraxial block is an attractive option for non-spine surgery in patients with cervical disease that may make airway management or positioning difficult, for example, in patients with rheumatoid arthritis requiring joint arthroplasty. It is also believed to be an effective preventative measure against autonomic dysreflexia in patients with high cord injuries.
Intraoperative airway management
As the majority of patients undergoing spine surgery will be placed in the prone position, tracheal intubation remains the standard technique of airway control although a supra-glottic airway (SGA) has been employed in some circumstances. Suxamethonium should be avoided during tracheal intubation if myel-opathy or myopathy might be present, because of the risk of hyperkalaemia. Reinforced, kink-resistant endotracheal tubes are popular but not essential. he tube f xation technique must be resistant to wetting with cleaning solutions in high spinal surgery, and waterproof material, such as Bioclusive transparent dressing, is usually satisfactory.
There is no conclusive evidence in relation to the optimal airway management technique in patients with possible cervical instability. Manual in-line stabilization has been recommended, but there is no evidence of improved outcome with any technique. Practitioners should therefore use whatever technique is most suitable in their hands.
Double-lumen tubes or bronchial blockers may be required for thoracic spinal surgery. As thoracic discs or vertebral body lesions cannot be approached from behind, a thoracotomy may be required, and surgical access is more straightforward if the lung is deflated.
Tracheostomy is prudent in many cases of high anterior surgery or if a maxillotomy or mandibular split is required, as post-operative swelling can last for some days .
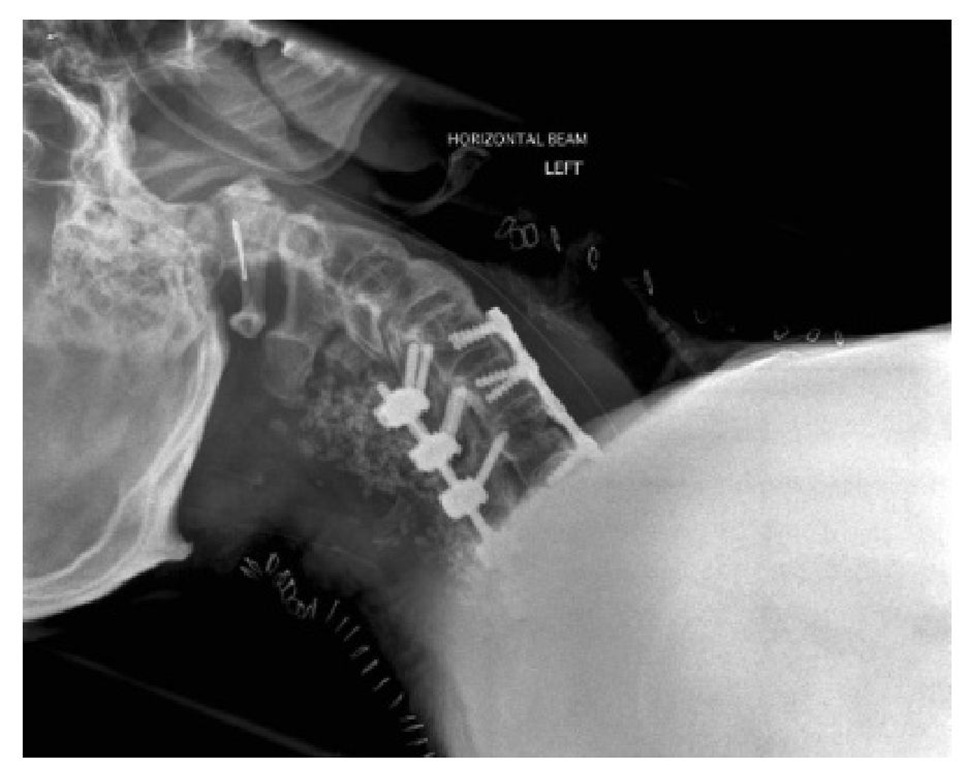
Post-operative airway obstruction
A post-operative haematoma capable of causing tra-cheal compression can occur after any anterior cervical operation and its treatment is immediate opening of the wound and evacuation of the haem atoma. However, airway obstruction due to tissue swelling is much more likely, particularly after lengthy surgery (>5 h) or surgery at high spinal levels. It is also more common if a patient who has had anterior surgery is then placed prone for a prolonged posterior intervention (Fig. 15.6). his is true even if the posterior procedure is performed some days or even weeks after the anterior approach. Extubation should be delayed until the following day if combined anterior and posterior surgery is performed and considered if anterior surgery lasts 5 h or longer. Any past procedure or intervention (such as surgery or radiotherapy) on the head or neck should raise suspicion that the lymphatic drainage of the laryngopharynx may not be normal and that airway swelling after prone positioning is more likely.
Under such circumstances, the cause of the airway obstruction is pharyngolaryngeal oedema, not tracheal compression, as peri- and supra-glottic tissue swelling occludes the airway. he symptoms usually occur within 6 h, but diagnosis can be delayed because stridor and desaturation are late signs. Wanting to sit up and complaining of difficulty in breathing are constant features. Te presence of a wound drain makes no difference to this complication.
Fig. 15.6. Radiograph of anterior and posterior fixation for cervical spine fracture. Post-operative airway obstruction due to soft tissue swelling is likely and extubation should be delayed.
Management
The immediate management of post-operative airway obstruction is opening of the wound, even though in most cases there is no haematoma. Tis is because relief of tissue pressure may critically improve airway patency. Tis fact is exemplified by a case report of airway obstruction due to extracapsular leaking of fluid during shoulder arthroscopy. In this case, initial rescue by direct laryngoscopy and intubation failed because of severe supra-glottic tissue swelling. However, a tracheostomy skin incision resulted in immediate improvement in the airway because of release of tissue pressure, and successful direct laryngoscopy and intubation .
The anaesthetist called upon to establish an airway in the presence of pharyngolaryngeal oedema is in an unenviable position. Folds of swollen pharyngeal tissue may make mask ventilation and direct laryn-goscopy difficult or impossible, and preparations for emergency surgical tracheostomy should always be made. Awake flexible fibre-optic intubation has been successful in the author’s experience but will not be suitable in the most acute cases. Because there is swelling of the pharyngeal soft tissues, airway collapse during inspiration often prevents a clear view of the cords, and the endoscopist must therefore advance the scope during expiration. Topical anaesthesia with lidocaine may be useful but, because it is an irritant, its use has been associated with complete airway obstruction. Te author has found that insertion of the endoscope into the trachea followed by a small dose of propofol (50-100 mg) allows the tube to be passed in these desperate patients.
Te use of a videolaryngoscope to facilitate intubation of three patients with severe airway obstruction due to supra-glottic swelling has been reported. Topical anaesthesia (6 ml lidocaine 4%) was administered via an atomizer and a remifentanil infusion run at 3 ng ml-1. Videolaryngoscopy and intubation were well tolerated. Inhalational induction of anaesthesia is often advanced as a safe technique in patients with airway obstruction, but the author has not known it to be successful in this situation. Te issue of whether muscle relaxant drugs should be used also remains controversial. However, in the author’s opinion, practitioners should use them whenever they feel that they will be helpful. Not using muscle relaxants is associated with difficult intubation, and there is a well-respected view that muscle relax-ants permit intubation in patients who are impossible to ventilate via a face mask when not paralysed. One group observed that, in patients with stridor due to laryngotracheal stenosis, positive-pressure ventilation via a laryngeal mask airway (LMA) after propofol and atracurium induction resulted in better gas flows than in the same patients during awake spontaneous breathing. Tere is no doubt that direct or videolaryngoscopy will sometimes be difficult, but, provided the glottic reflexes are obtunded, a gum-elastic bougie can be placed or a tube passed. Successful intubation after rapid sequence induction followed by ‘blind’ gum-elastic bougie placement has been described in four patients with grossly distorted pharyngeal anatomy.
If laryngoscopy is unsuccessful, an SGA should be considered. Fibre-optic-guided intubation can be performed subsequently via the SGA, which is removed after intubation. Tis technique uses an Aintree catheter for intubation, or placement of a gum-elastic bougie through the tracheal tube, removal of the tube and SGA, and then railroading of another tube over the gum-elastic bougie .