Introduction
The study of inflammation in the prion diseases is relatively new. Indeed, for a number of years the accepted dogma was that the prion diseases lacked an inflammatory response in the brain (1-3). This persists in spite of a number of studies showing that the pathological hallmarks of the prion diseases (PrPSc deposition, astrocytosis, vacuolation, and neuronal loss) are associated with the presence of activated microglia (4-7). At the heart of this discrepancy is a simple matter of what is meant by inflammation. The innate inflammatory response is the tissue’s response to injury or infection, and, as so succinctly put by Metchnikoff in the late ninetenth century, "The essential and primary element in typical inflammation consists in a reaction of the phagocytes against a harmful agent" (8). Given that the microglia are the brain’s resident macrophages (i.e., phagocytic cells), we believe that the presence of activated microglia in prion-affected brains represents an inflammatory response (9-11).
Another problem that arises is one of histological description. The histological characteristics of inflammation include perivascular cuffing of neutro-phils, in the case of an acute innate inflammatory response, or lymphocytes, plasma cells, and macrophages, in the case of chronic immune inflammation. An acute response in the periphery (e.g., skin) is characterized by the presence of neutrophils (by 6-12 h) and later monocytes/macrophages (12-24 h) at the site of injury, but the brain’s response is altogether different (12-14). Following either a pro-inflammatory (e.g., lipopolysaccharide, cytokines) or a neurotoxic (e.g., kainic acid) lesion to the brain parenchyma, in addition to the activation of the resident microglia, there are few neutrophils and a delay in monocyte response by 48-72 h. Therefore, the acute inflammatory response in the brain is different than that seen in the periphery, because there is no leucocyte cuffing around blood vessels in the injured brain parenchyma. It is, however, identical to a peripheral response, in as much as it functions to activate and deliver phagocytic cells to the site of injury.
Unlike the prion diseases, the association of central nervous system (CNS) inflammation in Alzheimer’s disease as characterized by the presence of activated microglia, is now well accepted (15,16). In light of the similarities between Alzheimer’s disease and the prion diseases (17), it would be surprising to find that CNS inflammation was not also a component of the prion diseases.
Evidence for an Inflammatory Response in the Prion Diseases
Conspicuous activation of microglia has been shown at the terminal stages of a number of experimental models of prion disease (4,18). The distribution of activated microglia correlated directly with the distribution of PrPSc amyloid plaque deposition and vacuolation. Activated microglia have also been seen in association with PrPSc amyloid plaques in the human prion diseases including Kuru, Creutzfeldt-Jakob disease (CJD), and Gerstmann-Straussler-Scheincke disease (3,5,6,19-21); however it is not clear what, if any, role the inflammatory response observed in the brain at advanced stages of both human and experimental prion disease, plays in the pathogenesis of this group of diseases. In order to address this question, we have carried out studies to characterize the inflammatory cells at earlier time points during the course of the disease, and to define the inflammatory pathways that are activated in these cells.
Experimental Model
We have studied in detail one strain of prion agent, the ME7 strain of scrapie, which is in many respects the archetype of murine prion agents. It has been studied for many years, and produces a well-defined but widespread pathology that includes neuronal loss, astrocyte activation, amyloid deposits of PrPSc, and microglial activation (4,22-25). We routinely use stereotaxic microinjection (1 ^L) of either prion-affected (ME7 strain of scrapie) or normal brain homogenate (NBH) into the dorsal hippocampus of C57BL/6J mice. In addition to minimizing the trauma that is probably associated with the injection of larger volumes of inoculum, focal microinjection has allowed exploitation of one of the well-documented properties of the prion agent to spread within the CNS along neuroanatomical connections (26,27). In this way we have been able to follow the progress of the disease as it spreads from its origin in the dorsal hippocampus, first to the contralateral hippocampus and also ros-trally into the septum and diagonal band of Broca, along well-described neuronal pathways (28).
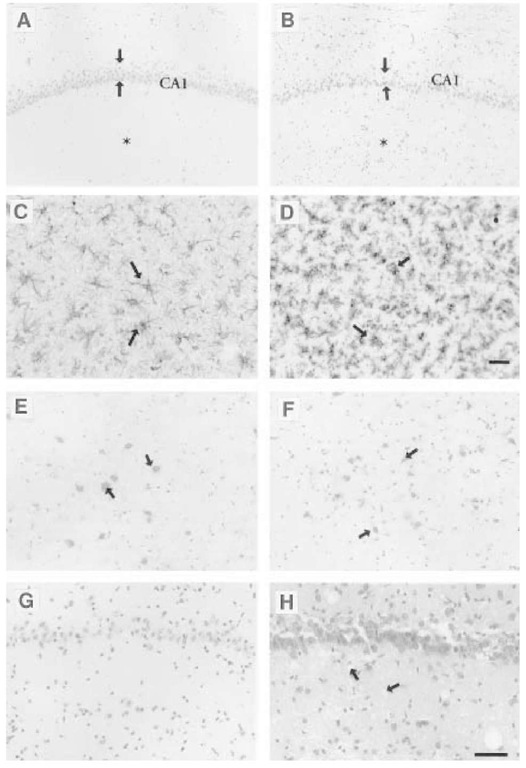
It has been possible to reproduce the previously reported clinical and pathological features of mouse scrapie (29), using focal microinjection. The mice display the typical clinical signs of disease, including hunched posture, pilo-erection, and reduction in mobility, at 23 wk after injection with ME7, and it is a further 2-3 wk before the mice become more profoundly ill (7). In addition, we have been able to confirm the presence of astrocytosis, neuronal loss, and PrPSc deposition and vacuolation at end-stage disease (Fig. 1). The vacuolation, visible as holes in the tissue with a diameter of 5-15 ^m, is, however, largely an artifact of tissue processing (30). Although this was first reported in the late 1960s (31), it has been overlooked more recently, which is surprising, because the pattern of vacuolation, or "lesion profile," has played an important role in defining the different prion strains, including variant (v)CJD (32).
The vacuolation is only a feature of fixed, paraffin-embedded brains, and is not seen on fresh-frozen cryostat sections. This artifact (30) may have implications for the understanding of prion disease pathogenesis. The vacuoles do not appear to contain lipid or carbohydrate storage material, and they do not appear to be lysosomal in origin. Because vacuolation is a feature of paraffin-embedded tissue, it is likely that the vacuoles arise as a consequence of tissue shrinkage, which occurs during paraffin processing, and this may relate to an alteration in the brain’s extracellular matrix. We thus looked for evidence of increased matrix metalloproteinase activity that might be involved in extracellular degradation. The 25-fold increase in stromelysin-1 mRNA expression, which is present at end-stage disease in this model, suggests that there is some modeling or degradation of the brain’s extracellular matrix and that this in turn could contribute to neuronal degeneration. There is evidence from the work of Chen and Strickland (33) that the interaction between components of the brain’s extracellular matrix and neurons is neuroprotective, and that disruption of this interaction by proteases directly contributes to the neuronal death in acute neurotoxic models.
We have also shown that there is an upregulation of a nonnuclear isoform of histone H1 in the brains of prion-affected mice with clinical signs of disease (34). This is seen both on Western blots, and on immunocytochemistry, in which upregulation of H1 is seen in neurons and within the neuropil and astro-cytes in areas of the brain affected by prion pathology. A similar picture is seen in Alzheimer’s disease brains. Histone H1, a lipopolysaccharide-binding protein, is a cell surface protein that is constitutively expressed on neurons. The role of this neuronal isoform is not established, but it has been suggested that it may act as an acute-phase protein (35), and that it may have antibacterial properties (36). Its role in the pathogenesis of prion disease requires further study. The absence of histone H1 upregulation in models of acute CNS inflammation (34) suggests that either the chronic neurodegenerative process and/or PrPSc accumulation is the trigger for histone H1 upregulation in prion disease.
The Inflammatory Response
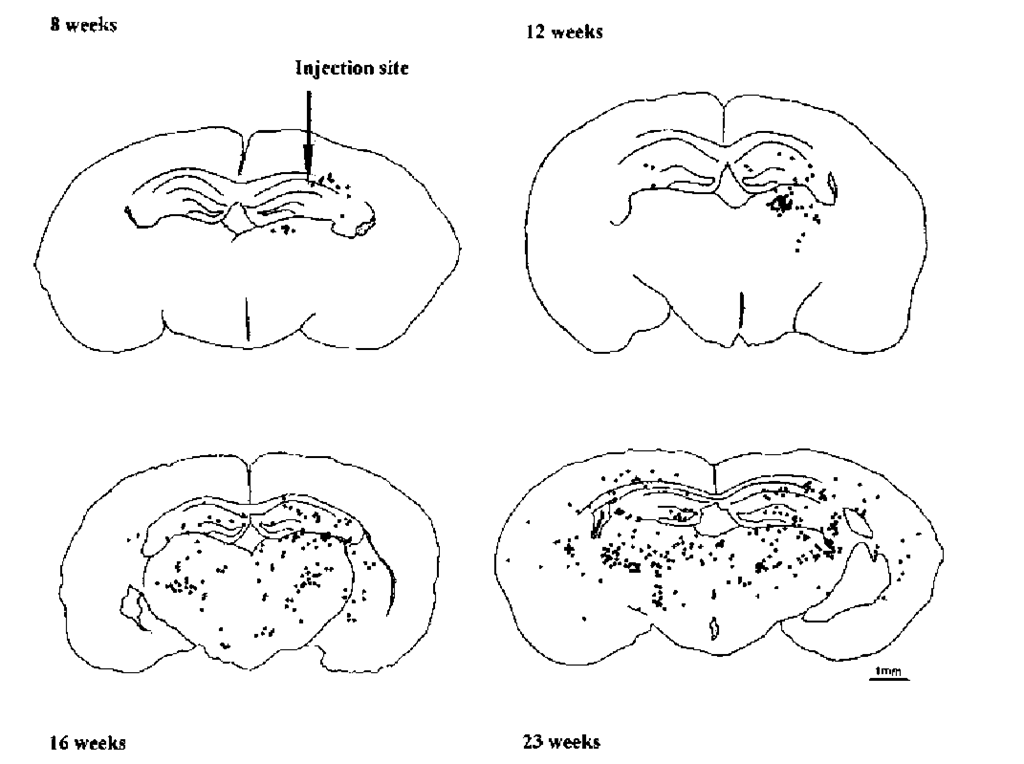
We have demonstrated the presence of activated microglia at end-stage disease, and, in addition, were the first to show the presence of cytotoxic (CD8+) T-lymphocytes in prion-affected brains (7). The distribution of CD8+ T-cells coincides with the distribution of activated microglia (Fig. 2). Since, at the end-stage of murine prion disease, there is massive neuronal degeneration, the presence of activated microglia is hardly surprising. The key issue is when does microglial activation first occur in the disease process, and how can microglial activation in prion pathogenesis be separated from the inflammation likely to be induced by the delivery of the brain homogenate to the brain parenchyma. We have found that there is little to distinguish between the acute inflammatory response in the CNS after the injection of ME7 or NBH up to 4 wk after intracerebral challenge (37). In the region of the injection site, the number and distribution of activated microglia and CD8+ T-cells was similar, comprising a peak of microglial and T-cell responses at 2-5 and 2-7 d respectively. In both cases, the blood-brain barrier was restored by 1 wk postinjection, and the acute inflammatory response had completely resolved by 4 wk. It is most likely, therefore, that the acute CNS response is secondary to the surgical procedure, and, more generally, to the injection of brain homogenate. There are additional factors that contribute to the neurodegeneration that is only seen later in ME7-injected mice.
An interesting point that arose from the study of the acute events following the injection of the brain homogenates was that it was not possible to attribute any acute neurotoxic action to ME7. There are studies that implicate fibrillogenic fragments of PrPSc in the neurotoxicity observed in in vitro models (38-40), but the evidence that PrPSc is neurotoxic in vivo remains circum- stantial. Indeed, although PrPSc co-localizes with areas of vacuolation and astrocytosis (41,42), there are reports of cases in which the neuropathology of prion disease occurs in the absence of PrPSc accumulation (43).
Fig. 1. Typical neuropathology seen in sections of brain taken from prion-affected mice with established clinical signs of disease (incubation period). Note the reduced thickness of the pyramidal cell layer (arrow heads) and the increased cellularity of the surrounding parenchyma (*), which is typical of sections of brain taken from prion-affected mice (B), compared with age- and time-matched controls injected with normal brain homogenate (A). The neuronal loss is associated with a marked astrocytosis, as seen using glial fibrillary acidic protein immunocytochemistry (C) and conspicuous microglial activation (D), as seen with an antibody to CD68. Consecutive sections show that the areas of microglial activation are also associated with the presence of CD3+ T-cells, using the pan T-cell marker KT3 (E), almost all of which belong to the CD8+ cytotoxic T-cell subset (F). Vacuolation is not observed in fresh-frozen sections of brain (G), but is visible on fixed, paraffin-embedded tissue (H). Both G and H are from ME7-injected mice with clinical signs of disease. Scale bars = 50 ^m
Fig. 2. The natural history of T-cell distribution in murine prion disease. Diagram illustrating the progress of CD8+ T-cell distribution at the different survival times indicated, following the injection of ME7 brain homogenate. The representative coronal sections at the level of the injection site were drawn using a microscope drawing tube. Each drawing shows the distribution in a single 10-^m section; each dot represents the location of one CD8+ T-cell. This distribution of CD8+ T-cells is similar to that of activated microglia at corresponding time-points during the course of the disease.
The earliest evidence of pathology that can be attributed to the injection of ME7, as distinct from the injection of NBH, is seen at 8 wk and comprises the co-distribution of activated microglia and CD8+ T-cells in close association with the injection site. There is no ongoing neuronal cell loss in the dorsal hippocampus at this time-point, so it is likely that this well-circumscribed inflammatory response is secondary either to the local accumulation of PrPSc or to subtle neu-ronal dysfunction caused by the accumulation of PrPSc. Because microglia respond to almost any disturbance of brain homeostasis (44), the microglial activation informs us that pathology is initiated between 4 and 8 wk. The pathology triggers an inflammatory response that is highly atypical, and, once this has happened, a stereotyped process ensues, resulting in the predictable spread of pathology to anatomically connected regions of the brain. This process culminates in the development of overt neuronal loss by 20 wk. After this time, the health status of the ME7-injected mice begins to deteriorate, as expressed first by a reduction in muscle strength (45) and a progressive decline in body weight, and, up to 4 wk later, by the development of the typical clinical signs of disease.
In spite of the marked inflammatory response from at least halfway through the course of the disease, indicating an ongoing pathological process, the mice appear to be well on routine monitoring of health status. It is not until the mice are examined more closely, using a panel of behavioral tests, that it is possible to detect subtle changes in behavior. The targeting of the hippocampus by direct focal injection, and the use of a scrapie strain (ME7) known to cause hip-pocampal pathology (46), opened the way to the use of behavioral tests that are sensitive to hippocampal lesioning. Hippocampal lesions are known to produce locomotor hyperactivity and impairment in passive avoidance behaviors (47); the use of open-field tests and multitrial passive avoidance, respectively, has enabled the detection of subtle changes in behavior during the early stages of prion disease. We have shown that prion-affected mice have behavioral changes from as early as 12 wk when locomotor hyperactivity is present, and, at 14 wk, when there is an impairment of cognition on the passive-avoidance task (45).
The few studies that have investigated the temporal development of behavioral changes in murine prion disease have produced conflicting results (48-53). These differences may relate to different mouse strain-scrapie-agent strain combinations, different routes of delivery, and different injection volumes used in these experiments. Our findings are similar to those of McFarland et al. (51), who, although using a different mouse strain-agent strain combination, showed that there was generalized hyperactivity in scrapie-affected mice, from approximately 60% of the way through the incubation period. They did not, however, comment on the activity of the mice at later stages of the disease. Another study, also using a different mouse strain-agent strain combination, reported that there was a reduction in the locomotor activity of scrapie-affected mice at late stages of the disease (52). In complete contrast, Suckling et al. (50) reported on an "excitable" phase, in which scrapie-affected mice became hyperactive shortly before developing the classic signs of disease at the incubation period, but displayed a reduction in mobility early during the course of the disease. Finally, Savage and Field (48) did not show any changes in motor activity in scrapie-affected mice. Our results on the passive avoidance differ from previous work done by Hunter et al., who showed that, in a different mouse strain, there was a mild impairment of learning with the 79A and 139A strains of scrapie, but not with the ME7 or 22C strains (52). Hunter et al.’s study tested the mice when they were approx 95% of the way through the incubation period, and at a time when the authors state that the activity of the scrapie affected mice was reduced (52). It is difficult to interpret these results, because the performance of the mice on the passive-avoidance task is likely to be profoundly affected by their reduced activity. Nevertheless, the early behavioral changes we have reported indicate that there is abnormal hippocampal neu-ronal functioning in prion-affected mice, which may be occurring as a consequence of the inflammatory response in the brain.
The Role of Inflammatory Response in Murine Prion Disease
The Role of Microglia
There is accumulating in vitro evidence that microglia may be activated by PrPSc, and that these microglia produce potentially neurotoxic molecules. The potential role of microglia in the pathogenesis of the prion diseases, based on these observations, is discussed in detail in topic 4. However, it is important to note that studies on microglia in vitro do not necessarily reflect the activities and functions of microglia in vivo. This difference is well illustrated by the contrasting antigen presentation characteristics of microglia in vivo and those of cultured microglia (see ref. 54). A number of studies have examined the activities of microglia and the inflammatory pathways in prion disease in vivo.
Activated microglia, by virtue of their close spatial association with areas of PrPSc accumulation, have been postulated to have a role in the production and processing of PrPSc (5,55,56). PrPmRNA has been detected in isolated microglia (57), and PrPSc immunoreactivity within microglia has been shown in a mouse model of prion disease (58). Furthermore, Jeffrey et al. (59) have ultra-structurally localized PrPSc to the lysosomal compartment within microglia located at the periphery of amyloid plaques. However, although Muhleisen et al. have confirmed that PrPSc deposition occurs in the same regions as microglial activation in human CJD, they have shown that very few microglial processes are associated with PrPSc immunoreactivity, and that activated microglia did not contain PrPSc (6). Together, these data suggest that microglia, rather than synthesizing PrPSc de novo, may have a role in the phagocytosis of exogenous PrPSc, which is then processed within their lysosomal compartment. Indeed, there is a substantial body of evidence indicating that PrPSc processing within the lysosomal compartment may play a central role in the pathogenesis of the prion diseases (60-62). The microglia may themselves become disease targets, as indicated by the presence of microglia with atypical morphology and occasionally intracytoplasmic vacuolation, and a consequent disturbance of their normal homeostatic function in the CNS may then contribute to the development of neurodegeneration in the prion diseases (21).
The mechanisms of neurodegeneration in prion disease remain the subject of investigation, but the most telling clue is that the distribution of neuronal loss is not directly dependent on the deposition of PrPSc (3). It seems possible that the contribution of activated microglia may lie in their neurotoxic potential. It is known that microglial activation is accompanied by the release of a number of mediators that have been implicated in causing neurotoxicity, including proteases, cytokines, and free radicals (63-65). Despite the obvious morphological and immunocytochemical evidence that the microglia are activated in murine prion disease, we have been unable to detect the cytokine interleukin 1 (IL-1P), either immunocytochemically or on enzyme-linked immunosorbent assay, at any point during the course of the disease in ME7-injected mice (66). Furthermore, at terminal disease, using quantitative competitive reverse tran-scriptase-polymerase chain reaction, we have been unable to detect any significant difference between ME7- and NBH-injected brains for IL-1p, tumor necrosis factor-a (TNF-a), IL-6, or interferon-y (IFN-y) mRNAs. These findings are consistent with a recent study showing "weak and inconstant" IL-1P and TNF-a expression in human CJD (3), but contradict previous studies based on immunocytochemistry of cytokine expression, both at end-stage disease and during the course of the murine prion disease (18,67). It is possible that the absence of cytokine expression in our studies is scrapie-agent-strain-related, because the studies that have previously reported cytokine expression used the 22A, 87V, and 301V strains of scrapie. However, given that all of these strains share with ME7 neuronal degeneration and a florid end-stage microglial response (4), it is surprising to find that only some of them are associated with the production of cytokines by microglia.
The absence of pro-inflammatory cytokines in the presence of a florid micro-glial response is surprising, given the data that are available on cytokine production by microglia (68). The profile of cytokine production by microglia has been described using isolated microglia in vitro, which are known not to retain their in vivo phenotype (69). It certainly appears that cytokines are implicated in the neurotoxicity seen in acute models of CNS injury, such as ischemia, and there is evidence that IL-1p, in particular, exacerbates acute neuronal degeneration (70). In contrast to either in vitro or in vivo models of acute CNS injury, the murine model of prion disease is characterized by pathology that evolves over many weeks, rather than as an isolated response to a single one-dose stimulus. The acute models of CNS injury cannot mimic the evolving dose-response relationships that must operate in a chronic disease, in which the contribution of pathogenic factors (e.g., abnormal protein or neuronal disturbances) will be both cumulative and synergistic.
The slowly evolving pathology, which provides a continuous signal to impact on the microglia, has parallels with the phenomenon of tachyphylaxis in peripheral tissues. Tachyphylaxis in the periphery is seen as a desensitiza-tion, with reduced cellular recruitment to sites already exposed to cytokines (71). The intact brain operates mechanisms to attenuate the acute inflammatory response (10,11). It is possible that, in chronic disease compensatory mechanisms supervene to protect the brain from what is clearly a profound inflammatory response. It is possible that an initial low level of synthesis of cytokines, produced early in the course of the disease, switches off any further cytokine production, but another explanation may lie in an opposing increase in anti-inflammatory cytokines.TGF-P is known to have anti-inflammatory actions in the CNS, with associated downregulation of proinflammatory cytokines.
Clearly, cytokines are not the only mediators of inflammation, and other inflammatory pathways, including arachidonic acid metabolites and the complement components, may have a role in the pathogenesis of prion diseases. Walsh et al. (73) have shown that there is upregulation of cyclo-oxyge-nase 2 (COX-2) in activated microglia in prion-affected mice. This is seen at 16 wk in our C57BL6J/ME7 model, and the number of COX-2 positive activated microglia increase with the progress of the disease. The COX-2 positive microglia are particularly numerous in areas of vacuolation, but were also seen in areas where vacuolation is less evident. This increased COX-2 expression is likely to result in the synthesis of prostaglandins and free oxygen radical generation, which may in turn contribute to the pathogenesis of the disease. Prostaglandin 2, one of the major prostaglandins released by microglia in culture (74), downregulates microglial function, including the production of pro-inflammatory cytokines (75). This would concur with the absence of pro-inflammatory cytokines observed in this model, and certainly merits further investigation.
The Role of T-Cells
Our model of murine prion disease is characterized by the accumulation of a subpopulation of predominantly CD8+ T-cells. The presence of these T-cells shows that, despite an intact blood-brain barrier, mononuclear cells can enter the brain parenchyma, and, indeed, Williams et al. (76), using bone marrow chimeras, have shown that some monocytes enter the brain during the course of the disease. The presence of CD8+ T-cells has been described in a number of other neurodegenerative diseases, and also in experimental models of CNS disease. Infiltration of predominantly CD8+ T-cells has been shown in Alzheimer’s disease (77) and amyotrophic lateral sclerosis (78). The recruitment of predominantly CD8+ T-cells to an area of damage induced by middle cerebral artery occlusion in the rat has been shown (79), suggesting that the immune system is also involved in ischemic CNS damage. Partial transection of the spinal cord in the mouse is also associated with an acute recruitment of T-cells to the site of injury (80). The role of these CD8+ T-cells in the pathogenesis of chronic neurodegenerative diseases, and acute brain and spinal cord injury, remains to be elucidated.
It is likely that the T-cells we have observed are monitoring rather than causing neurodegeneration, because T-cell-depleted mice can develop prion disease (81). Consistent with this idea, it is interesting to note that, despite the increased expression of major histocompatibility complex class I seen in our model, the T-cells themselves are not positive for IL-2 receptor, IL-1^, or IFN-y staining, and would appear to be switched off. The unique environment of the brain may mediate the downregulation of recruited T-cells. This phenomenon has been reported in T-cells isolated from the brains of mice with Sindibis virus encephalitis, which showed downregulation of cytokine production (82).
The Significance of Inflammatory Response in Murine Scrapie
The presence of the inflammatory response so early in the course of prion disease, before there is any neuronal loss, indicates that CNS inflammation could contribute to the pathogenesis of the disease. This is highlighted by the spatial coincidence of the inflammatory response with astrocytosis, PrPSc accumulation, and vacuolation, not only in an intracerebral model of prion disease, but also following intraocular injection of ME7 (83). There is also indirect evidence for the contribution of CNS inflammation to prion pathogenesis, from the work of Ehresmann et al. (84), who showed that co-infection of mice with a nonpathogenic adenovirus, which would produce inflammation, accelerated the course of the disease; Outram et al. (85,86) have reported that treatment of scrapie-affected mice with anti-inflammatory steroids delayed the development of clinical signs.
It appears that the inflammatory response and/or PrPSc accumulation contribute to the behavioral abnormalities we have detected during the early stages of the disease, and we have suggested that such abnormalities arise as a result of abnormal neuronal functioning (see refs. 45,87 and see topic 11). The early pathological and behavioral findings represent an important advance in the preclinical diagnosis of mouse prion disease, because they are robust markers of ongoing disease at a time when neuronal loss has not yet occurred. There are also striking parallels with the natural history of the human prion diseases. In particular, the reports of early behavioral and psychiatric disturbances consistently seen in variant CJD (88), but also less frequently reported in the other types of prion disease (89), suggest that there is also an abnormality of neuronal functioning in the human prion diseases.
The challenge now is to tease apart the relationships among the inflammatory response, PrPSc accumulation, behavioral changes, and neuronal loss. This should be done with an eye on other chronic neurodegenerative diseases. In particular, there is now compelling evidence that the inflammatory component in Alzheimer’s disease may contribute to the development of cognitive impairment and disease pathology (15,16,90-94).