Melatonergic System
Melatonin not only regulates the circadian phase [75], but also acts as a hypnotic, is an effective free-radical scavenger and antioxidant, and directly induces gonadotropin-inhibitory hormone expression [76]. Interestingly, bright light during nighttime decreases melatonin secretion [77].
The existence of immunoreactivity against melatonin was demonstrated in the bacterium Rhodospirillum rubrum, one of the oldest species of living organisms, at possibly 2-3.5 billion years [78]. Bacterial melatonin might provide on-site protection of bacterial DNA against free-radical attack. Melatonin is also known to exert antioxidant effects in the brain [79], and sleep is hypothesized to function as an antioxidant or scavenging process in the brain [80].
Melatonin promotes and synchronizes sleep by acting on SCN-expressing melatonin MT1 and MT2 receptors, respectively. Synthesized melatonin receptor agonists exhibiting increased duration of action are expected to provide significant clinical value for treating insomnia patients [81]. The onset of melatonin secretion begins 14-16 hours after waking, usually around dusk [82]. Exposure to bright, midday light has been shown to increase melatonin secretion during the night, without a circadian phase shift [83]. Although the results are preliminary, in a study of 3-year-old children, early sleepers tended to exhibit higher levels of urinary 6-sulfatoxymelatonin (6SM) (6SM/creatinine ratio), the primary melatonin metabolite, compared with late sleepers [84].
Decreased melatonin levels in aged zebrafish have been shown to correlate with altered circadian rhythms [85]. Danel et al. observed an inversion in melatonin circadian rhythm secretion in alcoholics, not only during intake, but also during short- and long-term withdrawal. They concluded that circadian disorganization of melatonin secretion could be responsible for desynchronization in some alcoholic patients [86]. Because melatonin regulates the circadian phase [75], altered melatonin secretion could disturb circadian oscillation, producing various biological alterations. Nevertheless, in the rat, altered melatonin rhythm had no effect on circadian rhythms of locomotor activity and body temperature [87].
Serotonergic System
Exposure to morning sunlight has been demonstrated to activate the serotonergic system [88] and, conversely, a nocturnal lifestyle is unlikely to activate the serotonergic system. Moreover, depression correlates with decreased norepinephrine, serotonin, or both [89]. In addition, selective serotonin reuptake inhibitors, which increase the availability of serotonin at the synaptic cleft, have been widely used to treat depression. Emotional instability, typical in individuals with nocturnal lifestyles, might be associated with insufficient serotonergic activity. The serotonergic system is activated through rhythmic movements, such as gait, chewing, and respiration [90]. Adequate physical activity could, therefore, be important for the activation of serotonin. Exercise-derived benefits for brain function have been demonstrated at the molecular level [91], and physical activity has been reported to decrease the risk of Alzheimer’s disease [92-95]. Physical activity, which activates serotonergic activity, is one of the key factors in promoting brain function in animals and humans.
The concept of low serotonin syndrome, which comprises aggressiveness, impulsivity, and suicidal behavior has been proposed [96]. In adult, male, vervet monkeys, decreased serotonergic activity was reported to be a disadvantage, and enhanced activity an advantage, for attaining high social dominance status [97]. Disturbance in the lateral orbito-prefrontal circuit induces aggressive behavior and loss of sociability [98], and the serotonergic system has been shown to activate this circuit [99]. Serotonin levels, which are increased through exercise, have been shown to enhance learning ability [92]. Serotonergic activity is profoundly affected by the sleep-wakefulness cycle, exhibiting highest activity while waking, and lowest activity during rapid eye movement sleep [100]. Taking these facts together, it has been postulated that irregular sleep-wakefulness rhythm disturbs emotional control and sociability, due to decreased serotonergic activation in the lateral orbito-prefrontal circuit.
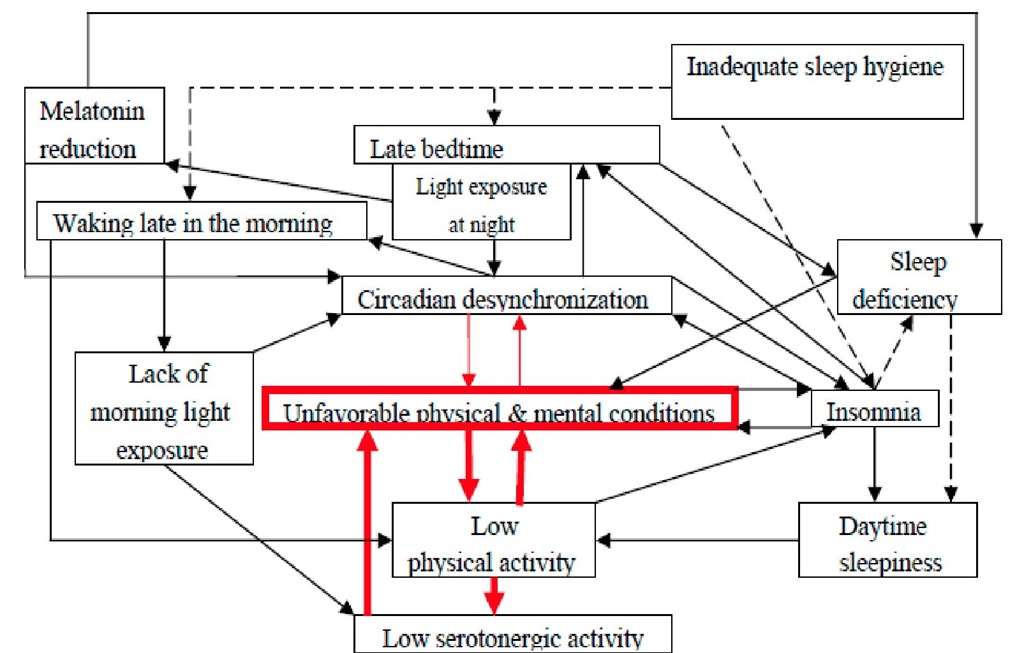
It is likely that circadian desynchronization results in unsatisfactory physical, mental and/or emotional conditions, presumably leading to decreased physical activity. If physical activity becomes too low, then the serotonergic system will not be activated. This is further confounded by a lack of morning light. The following negative cycles (solid filled lines in Figure 1) can be postulated in those with delayed wake-up times, delayed bedtimes, and an irregular lifestyle.
Figure 1. Schematic drawing of the development of asynchronization.
Reported Disease Conditions Associated with Circadian Disruption
Miike et al. [101] described altered circadian rhythms in childhood chronic fatigue syndrome, and reported that these patients suffered from an atypical, but continuous, jet lag condition. A British cohort study over more than 30 years [102] revealed that sedentary behavior during childhood increased the risk of chronic fatigue syndrome/myalgic encephalomyelitis, for which depression is a major symptom. Selective serotonin reuptake inhibitors have been reported to be effective in treating chronic fatigue syndrome patients [103]. It has been assumed that decreased serotonergic activity is involved in the occurrence of this syndrome. Melatonin has also been shown to be effective for chronic fatigue syndrome patients with delayed circadian rhythm [104]. One third of children with chronic fatigue syndrome exhibited abnormal cardiovascular regulation during postural changes (orthostatic dysregulation), which is characterized by instantaneous orthostatic hypotension, postural, or neural-mediated syncope [105]. Orthostatic dysregulation is a well-established clinical concept among pediatricians in Japan.
The characteristic clinical burnout symptoms, first described in 1974 [106], comprise excessive and persistent fatigue, emotional distress, and cognitive dysfunction. These symptoms are common among disorders such as depression, chronic fatigue syndrome, and vital exhaustion [107]. Burnout is positively associated with poor sleep quality, a sensation of not feeling refreshed upon awakening, and sleepiness and/or fatigue during daytime [108]. Burned-out subjects are reported to exhibit a higher frequency of arousal during sleep [107]. A study of University Hospital nurses revealed that daylight exposure for at least 3 hours per day resulted in reduced stress and greater job satisfaction, both of which were favorable factors for reducing burnout [109]. Because bright, midday light increases melatonin secretion during the night in elderly individuals [83], the melatonergic system, as well as the serotonergic system [110], might be involved in the pathogenesis of burnout.
Appels et al. introduced the terminology of vital exhaustion, which is conceptually akin to burnout [111]. In a prospective study of a large sample of healthy men, vital exhaustion was shown to comprise three factors – fatigue, depressive affect, and irritability – and the risk of subsequent myocardial infarction was attributed to fatigue from vital exhaustion [112]. Vital exhaustion is also associated with sleep disturbances. Polysomnographic recordings indicated that deep sleep stages were significantly reduced in exhausted subjects, compared with control subjects, suggesting that normal restoration processes, which occur while sleeping, are impaired in exhausted subjects [113]. In addition, exhausted subjects presented with a greater number of sleep complaints, shorter sleep duration, frequent napping, and poorer sleep quality [111, 114-116].
Fibromyalgia is characterized by widespread pain and muscle tenderness lasting at least three months, as determined by palpation [32]. Patients with fibromyalgia commonly complain of light and non-refreshing sleep, fatigue, cognitive difficulties, and psychological distress, including symptoms of depression and anxiety. Interestingly, a serotonin and norepinephrine-reuptake inhibitor has been reported to be successful in these patients [117], as well as melatonin for treating the pain associated with fibromyalgia [118].
Decreased circadian rhythm amplitude has also been reported in a more common condition – depression [119]. Moreover, decreased amplitude in circadian core body temperature changes was reported in delinquent student patients diagnosed with a desynchronized condition [120]. External and internal desynchronizations were two of the three major components of jet lag [121]. Another major component was sleep deprivation [121]. External desynchronization refers to the conflict between the internal clock and external time cues. As an individual is exposed to new, external, time cues, the internal clock adjusts to the new time zone, which may take several days. Internal desynchronization, a loss of phase coupling between phenomena revealing circadian oscillation, takes place during readjustment of internal clocks, and each system adjusts itself differently. Internal desynchronization can also be induced by acute manipulation resulting in phase alteration [122], which is the case in jet lag. As a result of internal and external desynchronization, sleep loss occurs, which decreases the quality and quantity of various activities [29, 33-38]. This ultimately results in decreased serotonergic activity. For the transmeridian traveler, both physical cues such as daylight and darkness, and social cues, such as mealtimes and noise, encourage realignment of the circadian system.
In contrast, for the shift worker, physical cues are resolutely opposed to nocturnal alignment, as are most social cues stemming from a day-oriented society. Therefore, circadian realignment of shift workers takes longer than realignment from jet lag [123]. In addition, a forced, extraordinary schedule can also induce desynchronization [124]. As previously mentioned, alcoholics have been reported to display an inversion of melatonin circadian rhythm secretion, which could be responsible for their desynchronization [86].
As described in this review, chronic fatigue syndrome, orthostatic dysregulation, burnout, vital exhaustion, fibromyalgia, depression, jet lag, and shift work are likely to be a result of desynchronization and decreased serotonergic, as well as decreased melatonergic activity.
Although each of these disease conditions possesses its own specific origin, major symptoms, and course, there might be a similar pathophysiology between these disease conditions and the condition that many Japanese preschoolers/students are currently suffering from.
Asynchronization
More than half of the preschoolers/students in Japan complained of daytime sleepiness, while about one quarter of junior high school students in Japan suffer from insomnia. Moreover, as shown in Table 2, frequent complaints of students in Japan were compatible with associated features of behavioral-induced sleep-deficient syndrome [32], most likely due to inadequate sleep hygiene. If this were the case, these symptoms should be ameliorated following adequate sleep (by exclusion of dotted lines in Figure 1). However, such therapeutic approaches often fail. The students cannot fall asleep, despite sleep loss, and this is partly due to inadequate sleep hygiene consistent with excessive media exposure and low-level physical activity. Indeed, delayed wake-up times and bedtimes could be symptoms of a delayed sleep phase form of circadian rhythm sleep disorder. Although this article does not discuss this disorder in detail, it should be noted that there is confusion between this disorder and the biological- and lifestyle-related sleep phase delays that are especially common during adolescence [125]. It is possible that certain factors other than simple sleep loss and inadequate sleep hygiene are involved in many of the young people in Japan that exhibit delayed wake-up times, delayed bedtimes, and an irregular lifestyle. It has been assumed that decreased activity in the melatonergic and serotonergic systems, as well as desynchronization, are candidates for explaining pathophysiology.
Presumable Pathophysiology
In 1976, Aschoff and Wever described [126] that activity rhythm (wakefulness and sleep) and other rhythmic variables (e.g., temperature) often have similar circadian periods of approximately 25 hours. However, on occasions, the activity period may become substantially longer (e.g., 33 hours), while other rhythms continue with a period of about 25 hours. Such a state is termed internal desynchronization. Thus circadian desynchronization is used to indicate a loss of phase coupling between certain phenomena, which lead to circadian oscillation. It should be noted that this term arose from basic studies, and was not originally a clinical-related term.
Individuals with delayed wake-up times, delayed bedtimes, and an irregular lifestyle may also exhibit a loss of phase coupling between phenomena, circadian oscillation, and decreased amplitudes of other phenomena, although no concrete evidence has obtained to date. Desynchronization alone is not adequate to describe the clinical conditions that many young people in Japan are suffering from. In addition, many of these individuals likely display reduced serotonergic and/or melatonergic activity. I wonder a novel, clinical entity is required to improve understanding of the pathophysiology of these disturbances [3, 4].
In 1970, Winfree [5] reported that a specific, dim, blue-light, pulse stimulus, with a unique stimulus time and duration, resulted in unusual broadening of the daily eclosion peaks of the fruitfly, Drosophila pseudoobscura, even to the extreme of obscuring circadian rhythm. This phenomenon was termed "circadian singularity behavior", and has been described in a range of organisms, such as algae, plants, and mammals [127-132]. In humans, Jewett et al. [129] reported circadian rhythms of rectal temperature and plasma cortisol were abolished by a single, long duration, bright-light pulse administered during one or two successive circadian cycles. Huang et al. [133] demonstrated that temperature increases and light pulses can trigger singularity behavior in Neurospora circadian clock gene frequency. In addition, Ukai et al. [59] reported that a critical light pulse (3-hour light pulses delivered at a specific circadian time (CT) ~17 (near subjective midnight (=CT18))) drives cellular clocks to singularity behavior in mammals. Interestingly, this phenomenon is transient [133], although removal of the stimulus is needed.
Table 3. Asynchronization.
|
Essence |
Disturbance of various aspects (e.g., cycle, amplitude, phase, and interrelationship) of biological rhythms that indicate circadian oscillation. |
|
Presumable causes |
Light exposure during the night. Lack of light exposure in the morning. |
|
Decreased physical activities. |
|
|
Disturbance of the biological clock and/or the serotonergic system. |
|
|
Disturbances related to the Autonomic Nervous System sleepiness, insomnia, disturbance of hormonal excretion, gastrointestinal problems, sympathetic nervous system predominance |
|
|
Somatic Disturbances tiredness, fatigue, neck and/or back stiffness, headache, persistent yawn, desire for sleep, wish to lie down, inactivity, lumbago |
|
|
Symptoms |
Disturbances related to Higher Brain Function disorientation, loss of sociality, loss of will or motivation, impaired alertness and performance, difficulties to remember, difficulties to concentrate |
|
Neurological Disturbances attention deficit, aggression, impulsiveness, hyperactivity, irritated, hypersensitive Psychiatric Disturbances Symptoms observed in depressive disorders, personality disorders, and anxiety disorders |
|
|
Therapeutic approaches |
Morning light, an avoidance of nocturnal light exposure, conventional approaches – light therapy, medications (hypnotics, antidepressants, melatonin, vitamin B12), physical activation, chronotherapy and alternative ones – Kampo, pulse therapy, direct contact, control of the autonomic nervous system, respiration (qigong, tanden breathing), chewing, crawling |
|
Prognosis |
Early phase: Disturbances are functional and can be relatively easily resolved, e.g., through establishment of a regular sleep-wake cycle Chronic phase: Without adequate intervention, disturbances can gradually worsen, involving loss of serotonergic activity, which is difficult to resolve. |
Taken together with this basic entity – singularity -, I designed a novel clinical concept -asynchronizatiopn-. Asynchronization is the result of disturbed aspects (e.g., cycle, amplitude, phase, and interrelationship) of biological rhythms that normally exhibit circadian oscillation, which presumably involves decreased serotonergic and/or melatonergic activity.
The major trigger of asynchronization is hypothesized to be a combination of light exposure during nighttime, which reduces melatonin secretion, and a lack of morning light exposure, which decreases serotonergic activity. Thus asynchronization symptoms (Table 3) include disturbances of the autonomic nervous system (sleepiness, insomnia, disturbed hormonal excretion, gastrointestinal problems, sympathetic nervous system predominance, etc.), as well as higher brain functions (disorientation, loss of sociability, loss of will or motivation, impaired alertness and performance, etc.). Neurological (attention deficits, aggression, impulsiveness, hyperactivity, etc.), psychiatric (depressive disorders, personality disorders, anxiety disorders, etc.) and somatic (tiredness, fatigue, neck and/or back stiffness, headache, etc.) disturbances are also putative symptoms of asynchronization. Complaints introduced in this article (Table 2) could be symptoms of asynchronization.
To detect the disturbance of biological rhythms, actigraphic recordings [134], as well as diurnal measurements of body temperature, corticosteroids, and melatonin are useful. Takimoto et al. monitored human clock genes in whole blood cells to evaluate internal synchronization [135].
The early phase of asynchronization is hypothesized to be functional and can be relatively easily resolved by establishing a regular sleep-wakefulness cycle. However, without adequate intervention, disturbances can gradually worsen, resulting in decreased serotonergic and/or melatonergic activity, which can be difficult to resolve. In Figure 1, red lines, especially the broad ones, are hypothesized to be involved in asynchronization. A portion of patients with chronic fatigue syndrome, orthostatic dysregulation, burnout, vital exhaustion, fibromyalgia, and depression are thought to suffer from asynchronization.