Introduction
Public healthcare is facing huge future challenges in order to deal with rising costs, growing demands of customers, information flow, demographic changes, and aging population. The healthcare service sector can be seen as an information intensive area during an era of innovation and information technology (cf. Bellamy & Taylor, 1998). According to McLaughlin, Rosen, Skinner, and Webster (1999), it is common to assume that technological interventions are almost inevitable and it is humans’ duty, at least to some extent, to follow the suggested development. In the organizational level of public healthcare, high expectations about the technology and its new possibilities are introduced. Additionally, the customers can seek support and advice for their healthcare needs from thousands online connections at any time of a day (e.g., Silber, 2003). The European Commission (2004) states how “eHealth offers European citizens important opportunities for improved access to better health systems” (p. 22). This trend has implications to human beings and governments.
The electronic health services produced by the information and communication technology (ICT) belong to the era of e-government. The e-government can be seen as an electronic exchange of information and services between different actors (cf. Malkia, Anttiroiko, & Savolainen, 2004; Oliver & Sanders, 2004). The development of information society throughout the last decades has brought up possibilities to adapt, modify, and reorganize healthcare practices and services (e.g., Gallivan, 2001; Turner, Fraser, Muir Grau, & Toth, 2002). The ICT has been used as a tool to reorganize best organizational practices, information management, and government. The ICT has also given a possibility to produce tailored healthcare services and to gain improvements in cost-effectiveness, access, safety, and quality of public healthcare services (Bates et al., 2001; Whitten et al., 2002).
In the future, the healthcare organizations in public sectors will confront many challenges by means of the ICT implementation. This situation is considered here both as the function of healthcare organizations and as the supply of knowledge intensive public health services. The current viewpoint presumes a paradigm that is structured on the basis of specific conceptualization. The purpose of this article is to conceptualize the complex topic of e-health from the governmental viewpoint and to clarify the best organizational practices. Special notation is also given for human resources, information management and the ICT implementation. Finally, some future trends are shortly discussed.
background
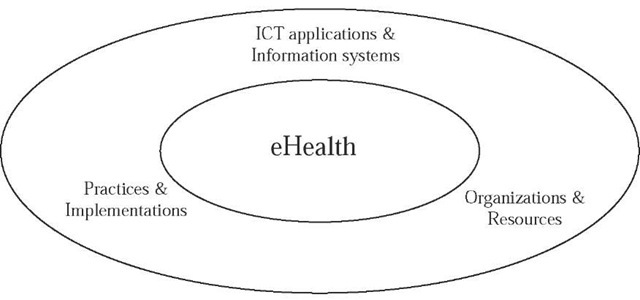
Experts define e-health differently and the term has some overlapping conceptual views. The term “e-health” is derived from the term “electronic commerce” (i.e., e-commerce), which was introduced in the mid-1990s to reflect the growing commercial use of the Internet. The e-health (cf. Eysenbach, 2001; European Commission, 2004; Silber, 2003), when recognized as a governmental issue, refers to the use of ICT applications or information systems to improve or enable health and healthcare services. Now it also refers to the main organizational and resource based factors before, during, and after an introduction of ICT. Finally, the term refers to best practices and implementations produced or needed to confront and manage with the ICT-based healthcare. The e-health concerns customers, patients, professionals, but additionally the whole primary healthcare, home care, and organizations like hospitals. It engages the terms like telemedicine, telematics, telehealth, medical and health informatics, interactive health communication, and so forth. To conclude, the e-health as a governmental concept give good reason for to describe the abovementioned combination by the means of three conceptual dimensions. conceptual dimensions of the e-health paradigm: THE governmental perspective
In the first dimension, the e-health connection can be found by referring to ICT applications and information systems in healthcare and in supporting functions (cf. McGinnis, 1997; Turban, McLean, & Wetherbe, 1999). In many cases, this has included telemedicine and health informatics as patients have been informed, examined and treated over distance by using appropriate applications (e.g., Hailey, Roine, & Ohinmaa, 2002). The e-health is seen now through issues like information system, standardization, and system quality (e.g., digital referrals, data security, access, and privacy, etc.). Also, the usability or user-friendly orientation should be placed under a close scrutiny. Hence, the applications and systems require understanding about technology and its effect on organizational structures, processes, and actors.
Figure 1. E-health concept according to the core governmental dimensions
Secondly, it is considered that by e-health it is possible to renew and to produce more effective healthcare practices and implementations. Now the e-health is studied typically in conjunction with key processes like the management of ICT applications and information (Plsek & Wilson, 2001; Tachakra, El Habashy, & Dawood, 2001; Walker & Whetton, 2002) and by the means of best practices or ICT implementations in healthcare (e.g., Pare & Elam, 1999). The introduction of technology may support or change operational practices in organizations. The operational aspect engages also electronic healthcare services as the e-health services are multileveled. Services represent, for example, the possibility of consumers to interact online, the possibilities for institution-to-institution data transmissions, and the possibilities for peer-to-peer communication of consumers. However, the overall question is about the best practices and implementations in order to successfully complete the e-health in service sector.
As third dimension, the organization and its various resources (e.g., economical and humanistic) have been under intensive study. For example, Parente and Dunbar (2001) found that hospitals with integrated information systems have higher total and operating financial margins than those without these systems. Whitten et al. (2002) did a systematic review and found no good evidence that telemedicine is cost-effective. Additionally, the e-health can be seen in terms of human resources. This is the case, for example, with the acceptance of ICT-based organizational solutions (Mathieson, Peacock, & Chin, 2001) and with the professional human resources (e.g., Syvajarvi, Stenvall, Harisalo, & Jurvansuu, 2005). The interest has also been in health services and in policy to provide a diverse range of services (e.g., Silber, 2003; Turner et al., 2002). Both customers and professionals can be seen as key actors, because they use applications and participate in electronic service interaction (e.g., Hailey et al., 2002).
Hence, the e-health from governmental perspective can be defined as health service and information delivered through different technologies. Applications of the ICT and information systems support health, healthcare, and health services. In case of current governmental perspective, the dimension of ICT applications and information systems concentrates mainly on technological system, standardization, and usability issues. The ICT applications can be seen as architectures to understand and plan information system components in the form of an organizational infrastructure. The most crucial questions are the standardization of information systems and their usability in organizational environment.
It seems worldwide that open technical standards to provide e-health are lacking. McGinnis (1997) studied health informatics and stated the critical importance of data exchange standards for communication between healthcare providers. The usability instead is traditionally defined (cf. Isomaki, 2002) by attributes like learnability, efficiency, memorability, errors and satisfaction. However, without neglecting the human factors like learning, sensation, and perception, memory, problem solving, and so forth. An optimal system should be easy to learn, it should be efficient to use, the system should be easy to remember, the error rate with the system should be low, and the system should be pleasant to use. Corresponding arguments of usability and human-centered design are also offered by ISO quality standards.
Second governmental dimension of e-health was about practices and implementations. E-health as practices and implementations emphasizes the need to combine knowledge and the use of ICT in various ways. In this article, the management as an organizational process has the viewpoint of ICT-based e-health. McLaughlin et al. (1999) claimed that in hospitals it is needed a wider perspective than social, since managers and users need to have a commitment to longtime innovative process. Clark (1995) suggested that leaders have the main responsibility for development work, because the problem with technological changes was frequently that people and technology didn’t meet or people didn’t participate.
The management has also direct link to best practices in organization and its health service production. Martin (2000) claimed that the quality of public services and cost-effectiveness depend on management. Smith (2004) studied how to inspire and motive professional service teams and indicated the importance of discussion and collective responsibility. The e-health can be seen as a part of knowledge intensive public services in a knowledge intensive society. The previous conceptualization invoked to describe the current e-health practices and implementations more generally as seminal goals for public healthcare organizations. However, it should be reminded that information technology does not necessarily lead so radical organizational changes as expected (Bellamy & Taylor, 1998; Nicholson, 2003).
The third governmental dimension of e-health involved organizations and resources. The governments try to manage with the increasing costs of public administration. Simultaneously the need to improve the cost-effectiveness of public healthcare has become apparent. One way to resolve the dilemma has been the use of electronic health services. However, the results have been controversial. Whitten et al. (2002) made a massive evaluation and they included 24 of 612 identified articles presenting cost-benefit information. About 30% of those 24 tried to solve the economic function of telemedicine without a clear outcome.
However, in public organizations the ICT has had often a transformative role. The e-health is understood and projected as being able to reshape the way healthcare services are delivered. The demands set by stakeholders are obvious. Governments want accountability to ensure that the funds are used effectively. Healthcare providers want a better quality of work life through the ICT tools. Patients and customers want access to the high quality healthcare service. One response has been the virtual life of organizations (cf. Nicholson, 2003). The virtual life in current context can be defined as a group of people or organizations that interact through interdependent task guided by common good purpose. In addition, the actors have learned to interact across space, time and inter-professional or organizational boundaries by using the ICT-based e-health solutions (Syvajarvi et al., 2005).
Organizations and E-HEALTH: implementation and human resources as crucial factors
Numerous organizational e-health projects with various goals are ongoing worldwide under public administration. For example, the European Commission launched an Action Plan for a European eHealth area in 2004. The aim is to support EU member states to materialize the benefits available from e-health, and to respond to the growing need for coordinated activities of e-health (European Commission, 2004). These kinds of activities denote a coherent agenda for the implementation of e-health. Hence, the e-health implementation may cause changes in organizational design and such changes typically require new organizational structures, processes, and personnel arrangements. From governmental perspective, the e-health either allows or forces an organization to rearrange especially its human resources. The focus is thus to analyze the relationship between e-health implementation and HR-centered organizational practice. Human resources are considered as a key area of e-health implementation.
Human resources have indeed an essential function both in knowledge intensive healthcare practices and in knowledge innovative services. The implementation of e-health has indeed organizational effects as it should concurrently support the patient mobility, facilitate the citizen-centered healthcare, but particularly to provide healthcare professionals new tools to sustain or improve the quality of public healthcare service. The implementation should allow greater flexibility, for example in case of inter-professional and organizational practices, to enhance information and knowledge exchange between humans. It is given here a synopsis of e-health implementation that contains previous governmental dimensions.
Many nations worldwide are known as countries with high technology. The extensive use of ICT and the adoption of various technological solutions represent everyday practice. In these knowledge intensive nations, the public policy has been largely based on the assumption that society will develop and succeed by focusing on ICT. For example in many European countries the information technology has been harnessed to promote social welfare. The ICT has been used for strengthening and developing the welfare society. The public service organizations and citizens thus have confronted the wave of e-government (e.g., Malkia et al., 2004; Oliver & Sanders, 2004). At the same time research has concentrated on the possibilities, quality, and costs of technology. However, what the implemented information technology means to public health service sector, public organizations, and especially to organizational human resources has usually received less attention. Under the issues of e-government and public services, there are several approaches to the human-centered e-health implementation.
Firstly, from the point of how the employees’ attitudes and approval affect the success of implementation (Mathieson et al., 2001). This kind of approach has produced theoretical models to explain how implementation depends on reasoned action of humans and the technology acceptance. Considering a more professional view, for example, the doctors who have received training in technology and understand technological concepts are more likely to grasp the positive impact of technology in healthcare (Pare & Elam, 1999). Burge, Creps, and Wright (2001) assumed that doctors are key persons to adopt technology in healthcare organizations, however, the doctors are not enthusiastically accepting the technology if it does not help everyday work. Tachakra et al. (2001) suggest that telemedicine includes the ability to rearrange the distribution of work; especially concerning the tasks of doctors and nurses. The ICT-based e-health seems not to be a question of single profession as it reflects over entire professional work society.
Secondly, the ICT has been studied by the innovative theories. Again models have been presented how a technological innovation is adopted in an organization through various phases. Gallivan (2001) developed a frame of references how to merge a technical innovation into the organizational operation. Thus, there are themes like management support, high resources, organization culture, own responsibility of learning, broad work roles, work security, and individual characteristics, which either increase or decrease the innovative implementation. These studies argue that the success of information technology in organizations more generally reflects the systems of innovations’ advance in organizations. Finally, as technology is implemented to organization more clear and exact strategies accompanied with leading spokesmen are required (Walker & Whetton, 2002).
Thirdly, the setup “e-health vs. implementation” stimulates the leadership and management dimensions. Clark (1995) suggests that the use of ICT is an organizational issue that needs efforts in the direction of change. The leaders have thus a responsibility to create and sustain participation, but also trust (cf. Harisalo & Stenvall, 2004). In good accordance, Plsek and Wilson (2001) found complexity in leadership and management of healthcare organizations. They assumed that leaders should found ways to make the change more attractive and meaningful for workers. This is done by securing the open information flow of good practices. The earlier observation about the complexity of knowledge intensive health services denotes the importance of information management. The information management refers to interdisciplinary procedures designed to provide and improve the appropriate information systems and resources by planning, organizing, executing, and evaluating necessary management operations. Thus, the human resource perspective both involves multi-professional diversity practices and presupposes the proper activities of human resource management (Syvajarvi et al., 2005).
Fourthly, the human resource centered ICT implementation considers the development of information systems according to usability factors, organizational practice, and the humanization of computerized information systems (Cummings & Worley, 2001; Isomaki, 2002). The usability of information systems is included in this framework. The information system development (ISD) can be introduced by different phases. It is stressed that the ISD tasks must be completed with knowledge concerning users and contextual analyses. Isomaki (2002) found that only a few information system designers have potential to contribute to the humanization of information systems. Cummings and Worley (2001) considered organizational change as a function of implementation process. They indicated how implementation causes organizational change and this can be controlled throughout singular phases like by information or system contracting and gathering, familiarizing, planning and accomplishing, evaluating and stabilizing. The humanization and e-health-based information system development can be seen as a part of organizational development (OD). Organization development in public health service sector applies this kind of knowledge and practice in order to help organizations to achieve effectiveness and social quality of work life.
The fifth and final aspect to comprise human resource and e-health implementation consists of the cognitive human capacity and service administration. The human capacity indicates the multilevel competencies of professionals. The service administration indicates both the service knowledge and management, which are approached in a customer-centered way. The e-health services are a challenge for both individuals and collective work society. Hence, individual, collective, and organizational competencies (e.g., Hamel & Prahalad, 1994; McLagan, 1997) are clearly required in different phases of the implementation. These competencies represent the foundation of service knowledge, which denotes the ability to arrange and manage both professionally and organizationally with the electronic public services. In present context this entirety (i.e., professional and organizational practices), the e-health implementation and customer relationships can be supported by appropriate and flexible service management. The public service management can comprise, for example, the dimensions of project management, human resource management, network management and customer relationship management. The concept of service management can be also seen as one value creator for service innovations or improvements, and with modifications, as a suitable management approach for organizations from various sectors (cf. Boyne, Martin, & Walker, 2004; Fitzsimmons & Fitzsimmons, 2004; Martin, 2000).
future trends
In the near future organizations will once again face a dynamic and turbulent environment. That requires flexible and fast response ability from the healthcare organizations and public services. The ongoing era of e-government has enabled organizations to acquire such structures and processes that support new or additional ways of interaction between electronic service providers and customers. Hence, the future trends of e-health indicate implications for health service users, service suppliers and entire society. The purpose of this section is to discuss shortly some essential future trends of e-health. The future possibilities and needs of e-health are introduced according to present literature and reflected alongside the three main dimensions described in current conceptualization. Thus, the final section is based on future prospects and e-health’s relationship to e-government.
The present view indicated that the public health care services will be going through major electronic turnarounds. The e-health revolution accompanied with the future possibilities are far away from straightforward. Many different issues have to be considered in order to make successful ICT-based transitions in public services. In case of organizations and resources there is going to be a further increase in information intensity of the e-health. Public institutions and human actors are stressed and challenged over again with more sophisticated, and hopefully with more user-friendly and appropriate information technology. There will be a need for competent health professional as continuous cognitive pressure is evident. A clear e-health challenge for public healthcare organizations seems to be how to manage with differences in processes, with strong professional culture of healthcare personnel, with cognitive pressure set by ICT, and with hierarchical or traditional structures.
These prospects as seen as future trends of e-health indicate cooperation, but also knowledge and information integration both in organizational and professional level. For example, healthcare professional will probably have fast and unhindered access to the latest knowledge and to the other relevant information needed in clinical practice. It is also assumed that the number of virtual organizations and new innovative services will be increased. The organizational and resource-based future of e-health has to be affected more by customers and patients. The e-health services are targeted as support for the customers (i.e., for those who daily cope with individual health). Thus, as the impact of ICT on healthcare professionals is extensive, similarly the e-health should be harmonized to the specific needs of the users. For example, citizens will increasingly have an opportunity to access their own health data and to contact directly to health professional (e.g., online booking, e-prescribing, home-care monitoring, health information bank, etc.). It is expected that the customer-centered approach will be even more vital as a resource for the future development of e-health. In knowledge intensive society, more demanding customers can be recognized.
In the future, the applications appear to be even more plentiful for consultations with other organizations, professionals, and patients. Portable and mobile tools will be increasingly adopted in healthcare settings together with many web-based gateways or portals. For example, the question can be about the new innovative e-health systems for retrieval, feedback, participation, clinical data management, and in general about the electronic health recording systems (EHR). There will be quite many views about the needs of e-health-based information systems and probably only a few will get it right. The challenge will be the standardization of ICT applications and information systems. Also the users themselves should be equal partners in development teams. As indicated before, people will probably found themselves in the era of virtual life. This indicates the increasing use of collaboration-support information systems.
Finally, the e-health future has implication in the dimension of practices and implementations. The ICT can be seen as a powerful change agent for the whole healthcare sector and it is important to recognize the importance of non-ICT factors in e-health. In this sense, alongside the system implementation it seems to be significant to concentrate on workplace practices and implementations. The best practices and implementations will be valued even more in the complex future of e-health. The e-health interventions based on ICT re-engineering, human-centered information systems, human resource and change management, and practical work innovations will play crucial roles for wellness in workplaces.
It seems that practical work tools or models that support decision making, management, preparation and processes will have an enormous importance. Public healthcare organizations will continue to invest huge amounts of resources into the latest ICT. It seems that new investments on organizational practices and implementations should support both professionals and customers. For example, one challenge is to combine multi-professional practices and service security for the customers benefit. During the continuing era of e-government, the e-health concept will be even more inevitable and natural part of the public healthcare service.
conclusion
The current governmental perspective of e-health has focused into three core dimensions. Current conceptualization has indeed some overlapping areas, but it is important that the approach to e-health is not done only by means of ICT factors or some single science. Hence, the e-health should follow the multi-scientific paradigm as the concept itself has been adopted by the experts of medicine, health science, applied information technology, social science, information and communication science, and by governmental and management science.
It was found how rich the topic of e-health is. The e-health was studied through the ICT implementation and human resources in the knowledge intensive healthcare service organizations. Hence, the implementation of e-health was recognized as a function of various practices and human resources together with future organizational possibilities in public service sector. Alongside the implementation procedures, the human resource was found to be fundamental. Thus, professional, inter-professional and customer perspectives were critical factors. Current perspectives go under the e-government. It combines the perspectives of governmental and management science, social science, health science, and applied information technology. The future trends of e-health thus involve various combined implications to customers and professionals, to service and system suppliers, and to organizations.
KEY TERMs
E-Government: An electronic exchange of information and services between different actors. Usually refers to local or state government activities that take place by digital processes and various networks.
E-Health: Health services and information delivered through different technologies in order to improve or enable health, healthcare and services with variable contents and transactions (cf. Eysenbach, 2001).
E-Health Usability: The design and technical features that allow electronic healthcare applications and information systems to be suitable for intentional use in a user friendly way.
Health Informatics: Knowledge, skills, and tools to support the delivery of healthcare information and services (cf. Silber, 2003).
Health Information System: An ICT-based routine constructed for the purposes of delivering health and medical care. Information system can be seen as physical process that supports an organization by providing information to achieve goals.
Information Management: Interdisciplinary procedures designed to provide and improve appropriate information systems and resources. Refer to planning, organizing, executing, and evaluating the necessary management operations.
Standardization of E-Health: The method to reduce or eliminate inconsistency, potential added costs and quality problems in applications and information systems of the electronic healthcare.