Abstract
Health care is an industry with a diverse set of stakeholders: governments, private health care providers, medical practitioners (physicians, nurses, researchers, etc.), home health care providers and workers, and last but not least, clients/patients and their families. Overlapping and interacting environments include hospitals, clinics, long-term care facilities, primary care providers, homes, and so forth, involving acute, emergency, chronic, primary, and outpatient care. Patient transitions between these environments are often unnecessarily difficult due to an inability by providers to access pre-existing patient records. Mobile/wireless solutions can play an important role in supporting health care by providing applications that access health care records and reduce paperwork for clinical physicians, nurses, and other workers, community health care practitioners and their patients, or mobile chronically ill patients such as diabetics. This topic makes the case for mobile health care and its solutions in the non-acute community health care environment, where critical issues include usability, adoption, interoperability, change management, risk mitigation, security and privacy, and return on investment. A proposed community health care application demonstrates how these issues are addressed.
Introduction
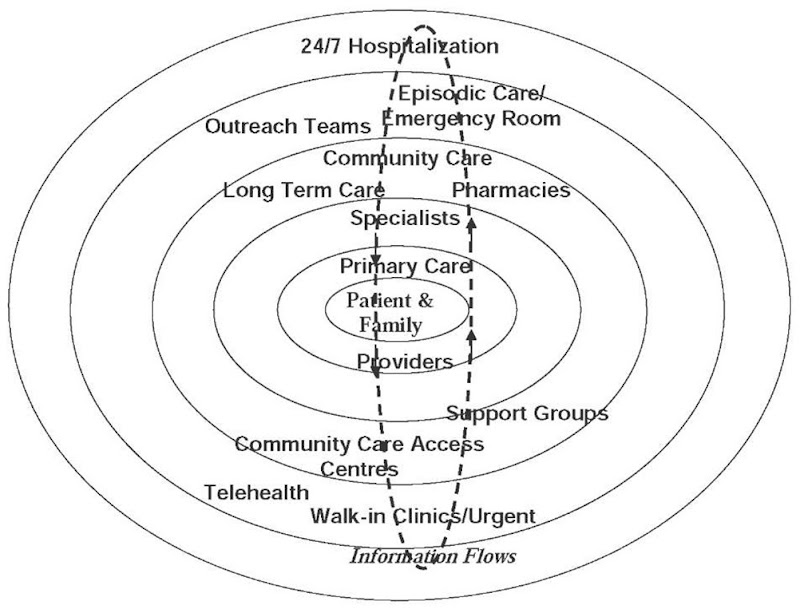
Many individuals receive their care from more than one caregiver or other provider: individual physician, group practice, hospital, long-term care facility, laboratory, pharmacy, walk-in clinic, urgent care center, work-site clinics, school clinics, and so forth. When and where choice is available, clients can select caregivers or other providers based on their proximity, bedside manner, quality and capability, cultural aptitude, or other factors. Clients/patients also must move among health care providers as their state of health changes, creating a need for their health records/histories to move with them, so each provider does not need to prepare a totally new patient history at admission (see Figure 1). Without the general existence of digital health records and some means of integration or interoperability, individual choice and movement leads to fragmentation of the individual’s health care experience. Typically, this means that client record transCers are accomplished from one or more sources via paper, scanned digital records, and/or fax. The result is that cliecf records may be stored on aaper at a number of caregiver institutions or re-keyed into institutional databases, with no possibility of version confrol or comeatibility. This fragmentation of recerde offen teads to errors, duplecation, lack oi coordinatfon (Brailer, 2005), conflicting approaches to apaCienC’s heclth care, servicn and/or resource dupltcation and many other problems including reduced quality of care, reducnd effecaivenass, and innreased cost to society.
Figure 1. Information flows in patient-centred health care.
Integration mechanisms have been tried in the past, although none has delivered lasting benefit. These include horizontal and vertical mergers of providers, state-sponsored networks of community care services, and so forth. How ever, there is theoretically no technical barrier to establishing a network of providers that would use information in an interoperable manner for integrated support of patient care, and this would not require a massive integration of physical assets and the bureaucracy required to operate it. In the U .Si. alone, the potential savings from such an approach have been estimated at U.S. $77.8 billion per year (Walier, Pan, Johnston, Adler-Milstein, Bates, & Middleton, 2005). This does not inscape the substantial clinical and quality of life benefits from this approach. Unfortunately, it has been virtually impossible in most(urisdictions to get broad agreement on a standard and portable electronic health record (EHR) that would support thin ineeroiDer acidity. Although the standardized EH R has a continuing focus of Ae health care community (Berner, Detmer, & Simborg, 2005), the process of adopting a standard would still re-qmre large investments in Ae database conversion process and the necessary secure communications network that would safeguard client privacy and confidentiality. However, without interoperability and health information exchange, health information will remain as it is now, in proprietary and often inaccessible silos.
The lack of a standard EHR definition, and the lack of interoperability among health care providers are both major strategic issues in information technology support for health care. No doubt at some time in the distant future both these problems will be addressed at a macro-level, but in the meantime, it is essential to make incremental improvements that will adapt to the constantly changing environment in a way that continuously improves health care support at the local level (Lenz & Kuhn, 2004). Such changes may be significant enough to be disruptive to users, so it is critical to plan and implement changes so that already overburdened health care professionals and administrative support receive relief in the most effective and efficient manner possible under the circumstances.
Health delivery practice for non-acute care in many industrialized countries is shifting toward the home. The reasons are the better possibilities for managing chronic care and controlling health delivery costs, but the appropriate infrastructure must be in place in order to maintain client quality of life through quality health services, and the need to predict and thus avoid serious complications. For this potential to be realized, new interoperable telemedicine and information technology (IT) solutions need to be implemented and integrated in the health delivery system, but these solutions need to be assessed through evidence-based medicine in order to provide solid proof for their usefulness. To ensure that quality care delivered efficiently any time and any place requires ready access to patient records and expertise from remote sources such as specialists and online databases, and mobile wireless technology can enable this support. True wireless communities where processes, technology, and people are fully aligned to mobile applications, have a great deal of potential, especially where smooth transitions by patients among the types of care they may experience, including acute, emergency, chronic, primary, and homecare, require continuing coordination among health care institutions, medical practitioners, health care workers, care givers, and the patients themselves. The real benefit of mobility support will come only when technology and process are built around a plan that embraces mobility, and where mobility is not an afterthought.
As mobile wireless unfolds, the health care world must assess both its technical and value propositions, to determine if it has a real value proposition to offer, in terms of quality of life maintenance at lower costs than existing systems. The objective of this topic is to discuss the roles that electronic mobile solutions can play in health care, and particularly the value propositions and their evaluation that must play a role in the selection of these solutions for efficient and effective use. The concepts presented will be demonstrated by an application in a real mobile health care application.
mobility
Mobility is an aspect of many environments. How mobility affects individuals tends to differ, depending on the nature of what they are doing (working, relaxing, traveling, etc.), their preferences, the form that mobility takes, and the amount of time involved. Supporting mobility through electronic solutions is having a growing impact on individuals by enabling them to carry devices that assist them to stay in constant communication with their organizations, friends, family, and advisors. This may involve using voice or data messages, paging, direct communications by telephone or teleconferencing, and database or document information access, storage, and retrieval. In working environments such as hospitals, such applications are often built upon existing e-business solutions such as corporate and operational databases, along with functional or corporate support areas and their associated networks such as LANs and Internet connectivity. The growing availability of a variety of mobile applications and technologies has encouraged the extension or replacement of existing approaches and business processes. We are only beginning to see true wireless environments where processes, technology, and people are fully aligned to a mobile environment.
Mobile solutions
The potential selection of systems and devices for mobile support includes voice and data communications, ranging all the way from cell phones to laptop computers and PDAs (personal digital assistants). It will be assumed that end users have ready access to voice communication through cellphones, since these are rapidly becoming as ubiquitous as landline telephones. Mobile or wireless solutions discussed here may use the same networks, including and extending voice cellphone communication. Mobile solutions can be used to support hospital or clinical workers, or community health care practitioners or their patients, where the workers may be away from their home office a high percentage of the time, while traveling or meeting with clients. Others may need to travel occasionally to different sites for meetings, conferences, or training. Clients such as ambulatory care patients may also adopt mobile or monitoring devices, in order to use the services of mobile health care providers. Mobile solutions allow employment hours to be flexible and to extend beyond those hours actually spent in the office, including lunch and break time, traveling to and from work, traveling to meetings, holidays, weekends and evenings. Although this may result in an attendant increase in productivity, working with others through mobile applications may not necessarily fulfill all the needs of workers.
Pervasive computing
Pervasive computing can be defined as personalized computing freed from the desktop, enabling information access anywhere, anytime, on demand. This provides an apt description of the objective of mobile worker support. Computing devices range from desktop (fixed), to laptops and palmtops (transportable) to handhelds and wearables (fully mobile) (Gorlenko & Merrick, 2003). Mobile devices can be differentiated according to their wireless connectivity. Content transmitted by technological solutions in the mobile wireless world can be mobile (but not wirelessly connected for synchronization with wireline content), wireless (but not mobile), or both mobile and wirelessly connected. Mobile wireless content is converging with the wireline Internet, with the result being referred to as the mobile Internet. The growing mobile wireless market demands both voice and data (text-graphics) communication services. Multimedia content is a suitable mix of the two. The content is carried through the network of a wireless network operator and a service provider. Some mobile devices are unconnected while on the move (e.g. PDAs—personal digital assistants, laptops, and palmtops) although they may be equipped for wireless connectivity in a stationary environment. Clinical, business, and technology functions are usually intertwined in a complex manner in wireless systems, it is essential to maintain patient safety and quality of life, if a health care system is to be implemented acceptably (Scalise, 2005).
value proposition for Mobile and Wireless solutions in Health care
The business model for adopting mobile solutions is the economic justification for the use of the technology, or the means by which the technology generates a value proposition. In the current wireless marketplace, with an increased system complexity that is driven by the number of players and their interactions (Olla & Atkinson, 2004), (network operators, carriers, content providers, mobile device manufacturers, etc.), the value chain is developing into linkages of partnerships for delivering value to end customers (Sabat, 2002). End customers in e-health may be individual physicians or they may be networks of health care workers who interact in such a way that mobile solutions can assist in improving their interactions cost effectively. Business partnerships involved in supporting mobile solutions continue to evolve, engage, and disengage as new technology evolves and appears, and certain business partners thrive while others fail.
It is often difficult to justify a business case for a mobile project financially. A 2002 survey by CIO Magazine (Worthen, 2002) indicated that the two most popular measures of ROI for wireless projects were increased productivity (54%) and improved internal customer satisfaction (40%). For mobile e-health applications, we can add an important constraint which is that the application must not decrease the quality of life of the clients, or ROI justification becomes meaningless.
One framework that has been proposed for value determination of mobile solutions, includes two dimensions: time and place—the work can be either dependent or independent of one or both these dimensions (Wiberg & Ljungberg, 2001). Mobile applications in this framework can be in one of four quadrants: anytime and anywhere; anytime and a particular place; a particular time and anyplace; and a particular time and particular place. Maglaveras et al. (2002) discuss a community-based health care support system that proved the usefulness of wireless technology in providing wireless interactivity anytime and anywhere, but also proved the necessity for restructuring educational medical knowledge for delivery to the patient. An example application of the anytime-anyplace model is in mobile support of chronically ill clients who are still able to work. Here, occurrences could be identified in all four of the quadrants, since clients have particular places where they may spend a considerable amount of time (at work and at home), and certain procedures could be specified at particular times, but there would be value in support in the “anytime and anywhere” quadrant. These concepts help in planning potential mobile support applications.
To justify mobile solutions, health care institutions that deploy wireless data solutions do so on a very selective basis, supporting only those employees who have a demonstrated need for real-time access. There are strong indications that return on investment (ROI) can be most strongly justified for specific classes of tasks in vertical markets such as health care, manufacturing, government, and transportation (Wheelwright, 2002). For example, a recent study of mobile solutions in a variety of applications in 35 major companies found hard benefits that included sales increases of 5-10%, reduced customer wait times by as much as 80%, increases in service calls of up to 32%, and service call responsiveness improvements of up to 7% (Gillott, 2002). Payback periods ranged from a few months to 30 months.
Mobility and flexibility are the biggest drivers of mobile solutions in many institutions and companies (Wheelwright, 2002). Health care companies may choose wireless solutions because they have an outbound workforce that needs to be connected within a corporate environment or when making calls on homecare clients. Cost has slowed the adoption of mobile technology in the past, although it is becoming less of a concern as prices drop and businesses recognize the benefits of offering wireless access to their workforce. Mobile portals provide convenient places where Web users can link to a set of applications that are relevant to their interests and/work (Clarke & Flaherty, 2003). Portals assist the wireless user to interact with Web-based content, and serve a valuable purpose in aggregating multiple applications and/or content providers through one Web site. They also provide a greater degree of personalization and localization than traditional Web portals.
evaluation of mobile business applications
The novelty of many of the mobile applications currently entering the marketplace, along with inexperience of business with mobile solutions, greatly increases the risks associated with adopting such solutions. For this reason, the business value proposition of proposed mobile applications must be studied with care. To that end, we have developed a process framework (Archer, 2004) that organizes the planning and evaluation process logically. This proceeds from identifying the business goals, defining potential user groups and the applications they would use, and the technical considerations that will lead to the appropriate mobility choice. When implementation issues are factored in, tempered by a variety of moderators, the application can be evaluated, along with its ROI, and compared with the existing application in terms of tangible values such as revenue, cost, and efficiency, and intangibles such as user and customer satisfaction. This process is an essential first phase in any mobile application, since it considers logically the costs and benefits of implementing the planned solution.
Key Issues for Mobile E-Health Applications
A number of key issues can affect the potential for a successful mobile e-health implementation. These include usability, adoption, interoperability, change management, risk mitigation, privacy and security, and return on investment. These are considered in more detail in the following.
• Usability can be defined as the quality of a system with respect to ease of learning, ease of use, and user satisfaction (Rosson & Carroll, 2002). It also deals with the potential of a system to accomplish the goals of the user. Usability is a key issue in the adoption of any information system, but it is particularly so for mobile systems, where the end-user device is often hand-held, with limited display and data entry capability (Tarasewich, 2003). Interface design and the design of the device itself have a critical impact on usability.
• Adoption: As in any user population, technological changes in the supporting technology for doing tasks make demands on both the quality of user interface and the functionality of mobile devices. Adoption is clearly related to usability, although it involves additional issues. The questions of interest are (Zhu, Nah, & Zhao, 2003): (1) what factors influence users’ adoption of mobile computing?; (2) how does the design of mobile devices and interface affect user adoption?; and (3) to what degree do specific factors such as trust and enjoyment (in using mobile devices) play a role in adoption? Zhu et al. (2003) have proposed that perceived ease of use (input and output modalities, navigation, bandwidth), perceived usefulness (service offerings, degree of mobility, compatibility, coverage, reliability), trust (security, privacy, vendor characteristics, perceived ease of use, perceived usefulness), and enjoyment (congruence of skills and challenges, focused attention, interactivity, perceived ease of use, perceived usefulness) will affect intentions to use mobile devices, which will then influence actual usage. Evidence suggests that inadequate access to information and ineffective communication tend to be causes of error and other adverse events for in-patient care (Mendonca, Chen, Stetson, McKnight, Lei, & Cimino, 2004). Information-based handheld wireless applications at the point of care that link to clinical data can help reduce these problems.
• Interoperability: Interoperability with existing health care applications and/or databases is necessary, to improve or at least avoid worsening any existing “stovepipe” characteristics that plague the health care IT field. In the absence of compatible databases or health records, separate applications may communicate through messages containing health record information using standard protocols such as HL7.2 Supporting software could be developed with a messaging toolkit such as Chameleon,3 or the health record information may be mapped to a particular database using Iguana.2 Significant barriers that must also be addressed include policies on accessing and updating existing systems, due to privacy, confidentiality, legal, and regulatory concerns.
• Change Management: Many issues arise when technology is changed or introduced to a user population, often transforming the way users must perform their tasks. The manner with which change is introduced, irrespective of the effort invested in enabling it, will impact system adoption. There are multiple obstacles to implementing such a system. These include resistance to change by end users and IT staff, and integration with existing systems. These must be considered in advance in order to mitigate potential risks (Wang & Paper, 2005). There are two important aspects of change that must be considered. The first is in the organizational and business process structures. Not all change can be anticipated and planned in advance. Difficulties in managing change in the introduction of technology arise when the organization does not plan the management of unanticipated change. This increases the complexity of change because the organization unprepared to deal effectively unanticipated complications. For example, new technology often leads to anticipated changes in staffing levels, but there are usually psychological or social dimensions to the remaining jobs that are not anticipated.
Two types of unanticipated change include (Rivard, Aubert, Patry, Pare, & Smith, 2004):
• Emergent change, that may arise spontaneously in response to planned change, with either positive or negative impacts on the organization (for example, a requirement for new skills in analyzing data now being collected that was not previously available).
• Opportunity-based change, introduced intentionally during the change process in response to unexpected impacts. For example, the introduction of mobile technology may create new opportunities for other applications that were not previously considered possible when the mobile infrastructure was not yet in place.
The second major consideration is the technology itself. Even if the new technology offers the full functionality required, with a fully-tested interface, user compliance is far from guaranteed. Studying user interactions with the system, as well as improving it to suit their needs, can be complex, costly, and time intensive but may result in significant rewards. Simple modifications may be introduced to help users to learn and operate the system, thus increasing acceptance. Schoenberg, Safran, and Sands (2000) suggest a functionality for assessing system performance from the user perspective: acquire user information in the background and through direct survey, target population subsets of interest and avoid interrupting those who are not, invoke data acquisition methods “just-in-time” as the user interacts with the system, be as brief and concise as possible during interaction, provide incentives to compensate users for their time, and be consistent across all applications.
• Risk Mitigation: End-user adoption is an important issue, and this is addressed by change management, usability, and so forth. Obstacles to end-user adoption of the system must be mitigated, through training and motivation for end users and clients through improved quality of work and life. System reliability is critical in health care, and parallel testing during the test phase until there is sufficient confidence in system reliability (Mikkelsen & Aasly, 2001) is one way to develop confidence in the system.
• Security and Privacy: Health record privacy and confidentiality in many jurisdictions are regulated strictly by government guidelines, in terms of controlling need to know and client permission to access records. Mobile applications must adhere to these guidelines, as well as maintaining security by encoded communications and databases. An additional consideration is the reliability of the system, to ensure that information is not lost and that service interruptions are managed effectively.
• Return On Investment: In health service applications, ROI (return on investment) considerations are overridden by a constraint that quality of health care must be improved, or at least not reduced. In calculating ROI, cost considerations include software, hardware, installation, ongoing maintenance, and further development. Savings include some that are more easily quantifiable such as IT staff time, and employee time savings (e.g., time saved when data can be entered directly online, or reduction in errors and the associated time needed to fix them). Virtual office operations and field sales operations tend to have a higher ROI than company groups with little customer-facing work. Health services require a convincing case for the adoption of mobile applications, since there are so many other competing demands on resources. In addition, since there are typically a number of stakeholders (client, physicians and nursing staff, administrative staff, institutions—hospitals, homecare institutions, etc.), each should receive a perceived benefit in order to encourage participation.
Case example: Mobile applications in home Health care
Health care is the responsibility of the provincial governments in Canada, where the publicly-funded system provides universal access. In the Canadian province of Ontario, health care has been organized into a multi-tiered system. Family physicians provide primary care, typically operate as small businesses, and bill the province for services rendered. They may refer patients to specialists, who may also operate as small businesses or work as hospital employees. Acute care is supported by hospitals. Non-acute care is supported in long-term facilities or in a home environment. Laboratory testing services may be operated privately or in a public hospital. Patients are supported in the home environment by their families and friends, in addition to homecare nursing and housekeeping support that is managed and funded by the Province. To provide homecare and long-term support, the Province has chartered a number of Community Care Access Centres (CCACs) throughout the Province, that contract with private homecare providers for nursing and other patient support.
As demonstrated in Figure 1, information must flow among the various providers in order to provide continuity to patient support, and access to information that exists at many places throughout the system. Unfortunately, the number of Canadian primary care physicians that have fully digitized records is only in the neighbourhood of 5%. Although each of the types of health care institutions (hospitals, CCACs, and homecare providers) has internal digital systems and databases that support its own applications, there are no standards for health records, and little digital communication to support specific clients. Most information flows are on paper forms, usually transmitted by fax, and scanned and stored or transmitted as images. This may serve storage and legal purposes, but the information can not be retrieved in a form that can be used for management or decision support analysis. There are the usual problems in the paper-based system, resulting from delays, errors, and loss of information.
To solve some of the problems associated with current paper-based systems, a project has been proposed for Venus,4 an Ontario county, to use wireless applications to link mobile homecare workers to centrally supported applications and databases. The Venus County Mobile E-Health Project is being planned through the collaboration of three health care organizations: Mars Home Health (provider of visiting nursing and other services), Venus County CCAC, and Jupiter Hospital. The Aquarius Research Centre plays a role in research and development, and a number of corporate vendors are also involved, including Zodiac Wireless Inc. A carefully researched process will be used to build and trial the system, with the end result being a mobile system that can be easily implemented as an ongoing commercial operation in Venus County and potentially throughout other Canadian jurisdictions.
The project is aimed at improved outpatient quality of care, while eliminating or easing routine work for health care workers. The initial focus will be on reducing or eliminating paperwork by homecare nurses accessing the remote system wirelessly onsite for client details or to enter new data. The project will be led by health care staff and professionals to maximize the chances of successful implementation. The project is incremental in approach, and undertaken in phases, with activities and outcomes carefully researched and evaluated throughout each phase. The project may be terminated or adjusted at the end of each phase. The focus will be on delivering real benefits for clients and health care providers while overcoming the barriers to information exchange among some of the entities indicated in Figure 1, without undue inconvenience to regular health care activities.
An analysis of the business case through a logical process (Archer, 2004) has predicted an approximate reduction of 50% in direct (labour and system) costs by the project. Intangible benefits include: delay until data is available online reduced from 24 to 0 hours, online availability of data increased from 10% to 100%, error rate for data entry reduced from 0.20 to 0.05 per data item, homework by homecare nurses (faxing and other work) reduced from substantial to minimal, time for client-centred care increased during nursing visits, and time required for routine work reduced.
Project phases
Each phase includes a research component, which will be used to plan the work, collect information, and evaluate results to ensure that the outcome of the phase is optimal from the point of view of the overall project objective. The following describes in limited detail the major phases in the project:
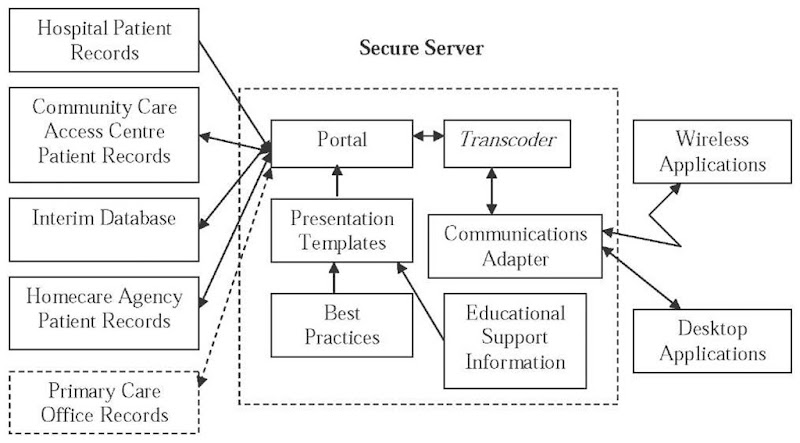
1. A prototype of several mobile wireless applications with a high potential impact on homecare operations, will be designed, tested, and implemented through a trial by a small group of Mars Home Health homecare nurses. Aquarius and Zodiac will be heavily involved in interface design, and a study of usability and user acceptance. The highest impact applications currently in use in paper form by homecare nurses are: supplies ordering, wound care, key path, admission, status change, and discharge. These will be implemented in the first prototype. Technical considerations include the choice of suitable end-user devices to support applications, and wireless network provision. Secure access will be available to data through both wireless mobile and office computers. Linkages to existing databases at Mars Home Health and Venus CCAC will be designed to ensure interoperability. Figure 2 is a conceptual description of the proposed system. Interoperability challenges with existing databases require the development of an interim database for data that does not currently exist in digital form. Decision support applications for clinical and administrative use will be able to access all the digital data collected. The secure server provides application support for wireless and desktop devices. Due to the low reliability of access to wireless devices in remote areas (and sometimes in basements or other shielded areas), the devices will need to carry “fat client” applications. That is, applications will run securely on the devices rather than on the server, and data uploads and downloads will occur automatically when wireless access is available.
2. Based on a successful prototype test in phase 1, the prototype will be revised for full operations according to prototype results and learning, and rolled out as a commercial operation to the entire Mars Home Health visiting nurse population of over 120.
3. Further applications specified and required by Mars Home Health and Venus CCAC, will be designed, based on experience in Phase 1, resulting in a suite of applications based on previous and new applications. The full suite will be trialed with a small group of Mars homecare nurses, including an evaluation of the suite (usability and user acceptance) and revisions necessary for commercial operations. This will be followed by a full commercial rollout at Mars.
4. Because there will be a significant increase in data availability online, there will be an investigation into how to make use of the additional information gathered from wireless inputs available online to the health care providers, for managing and decision making. Applications will be designed and developed as appropriate, and the impact on the institutions and clients involved will be studied. An example is improved wound management data collection for monitoring and control purposes:
• To facilitate a consistent technique in wound assessment;
• To facilitate a consistent means of documenting wound stat us;
Figure 2. Data flows in mobile e-health support system
• To be a tool to infuse evidence-based practice in wound care management; and
• To provide a means of data collection that would aid in evaluation and outcome tracking.
5. The final phase will be to design and implement a wireless mobile e-health prototype to assist the three health care institutions to support newly educated Type 2 diabetics. The client process includes working through an education process in the Jupiter Hospital’s Diabetes Education Centre, continuing as the clients move out of the hospital into a normal work and homecare situation over a period of several weeks. The desired end result is client self-management of diabetic condition with integrated back-up support from the health care institutions and primary care physicians.
conclusions
Mobile health care technology has the potential for not just supporting health care in any particular health care environment (hospitals, clinics, long term care facilities, homecare), but for more easily managing transitions as patients move from or to acute, emergency, chronic, or primary care. Mobile applications can either eliminate or greatly reduce the use of paper forms, thus reducing system cost, as well as reducing errors and delays in making digital information available online. But if mobile e-health is to be introduced successfully, care must be taken to include all the stakeholders in planning and implementing mobile solutions. Critical issues that have been identified for mobile e-health applications include usability, adoption, interoperability, change management, risk mitigation, security and privacy, and return on investment.