Introduction
Neurogenic claudication was first related to lumbar stenosis (Verbiest H, 1954). Since, decompressive surgery was indicated in patients who failed to respond to conservative therapy. It is followed by posterior fusion in cases where the motion segment showed instability or in case where a secondary instability is expected to develop after surgery. However, while many patients have benefited from fusion procedures, successful fusion has not always been accompanied by clinical improvement (Adelt D et.al, 2007)
Evidence is growing that fusion may in fact have undesirable long-term effects on the remainder of the spine, particularly on the immediately adjacent motion segments(Kong D-S et.al, 2007; Etebar S, Cahil DW, 1999). This adjacent-level degeneration is typically seen rostral to a fused segment but may also occur caudal to a fusion, especially when the fusion occurs at the L4-5 level. The phenomenon is thought to be due to the altered biomechanics of the fused spine, where in abnormal forces acting upon the intervertebral discs and facet joints adjacent to the fused segment precipitate the accelerated failure of these stabilizing elements (Kanayama M et.al, 2001). From this evidence for adjacent-segment degeneration emerged the concept of "dynamic" or nonfusion stabilization of the lumbar spine.
Rational
Posterior dynamic stabilization, in which pedicle screw fixation is coupled with a flexible longitudinal connecting system, presumably allows for the normalization of intersegmental motion (Kaech DL et.al, 2001). This stands in contrast to traditional fusion surgery, in which the goal is complete and immediate elimination of motion and, ultimately, arthrodesis (Kaech DL et.al, 2000). While both strategies seek to address the underlying pathology of microinstability, the dynamic stabilization approach promises to do so in a more physiological manner. By "restoring" normal motion, mobility is theoretically preserved rather than eliminated, and the forces acting above and below the construct are altered to a lesser extent, reducing the potential undesirable effects of fusion (Kaech DL, Jinkins JR, 2002). Recently, new concepts, such as soft stabilization, dynamic stabilization, and motion preservation, have been explored as alternative treatment options to lumbar fusion.
Interspinous process spacers have been introduced as a possible alternative to spinal decompression and fusion for the treatment of neurogenic intermittent claudication (NIC) and discogenic lower back pain (Bowers C et.al, 2010). The interspinous devices distract the Neural Foramen, unload the intervertebral disc, and limit spinal extension, improving central canal and foraminal stenosis. Interspinous Distracter (ISD) is designed to stabilize the motion segment after neural elements decompression in lumbar stenosis, tolerating flexion and extension in this segment thus preserving the adjacent segment from deterioration.
The first interspinous device, the Wallis system (Abbott Spine), was developed in 1986 and used in patients with recurrent disc herniation. It was found to improve outcome in patients who underwent a second discectomy incorporating the Wallis device (Mariottini A, 2005). The second generation of the Wallis implant, made with elastic polyetheretherketone (PEEK), has been shown to reduce pain severity in patients with mild to moderate disc degeneration, lateral recess, central spinal stenosis, and significant lower back pain when used in combination with other surgical interventions. Other interspinous spacers used in Europe but not approved for use in the US include the DIAM (Medtronic Sofamor Danek) and the Coflex (Paradigm Spine) (Mariottini A, 2005; Senegas J, 2002). The X-Stop device (St. Francis Medical Technologies) was approved by the US FDA in November 2005 and has been shown to be superior to nonoperative therapy in patients with NIC (Zucherman JF, 2004).
While the time course and prevalence of adjacent-segment disease are not fully known, there is increasing evidence in the spine literature that its effects may be seen soon after fusion surgery and in as many as 30% of patients(Christie SD et.al, 2005). In a recently published large retrospective analysis (Chen et.al, 2001) reported rate of clinical adjacent-segment disease was 30.3% and showed that patients in whom adjacent-level disease developed had significantly worse Oswestry Disability Index scores than those without adjacent-level disease. They further identified age > 50 years at time of surgery, increasing length of fusion, and extension of the fusion to L1-3 as significant risk factors for the development of adjacent level disease. No significant difference was identified between posterior and circumferential fusion.
Our experience is based on 87 cases performed between September 2008 and January 2011 with different lumbar spine pathologies (Table1). The ages of our patient were between 45 and 70 years, with a mean age of 55 years. All patients were treated with Interspinous Distracter (ISD).
|
Number of cases |
Pathology |
Male / female ratio |
|
33 |
Bi-Foraminal stenosis |
24/9 |
|
21 |
Lig. flavum hypertrophy |
6/15 |
|
18 |
Suspended vertebrae |
12/6 |
|
9 |
Facet syndrome |
All females |
|
6 |
Adjacent syndrome |
3/3 |
Table 1. Pathology of the patients at the time of presentation.
Decision making
Diagnostic criteria
Preoperative patient evaluation included plain lumbar film, lumbar MRI, lumbar CT and lumbar osteodensitometry.
MRI assesses the canal and foramina stenosis and the joint synovium. In the latter, weakness or absence of the intracapsular (intra-articular) white signal on T2 weighted sequences signals is characteristic of degenerative disease of the joint.
Lumbar CT assesses the lumbar facets.
All patients with confirmed osteoporosis by osteodensitometry were excluded from this type of treatment.
Indications
Patients are eligible for enrolment if they have:
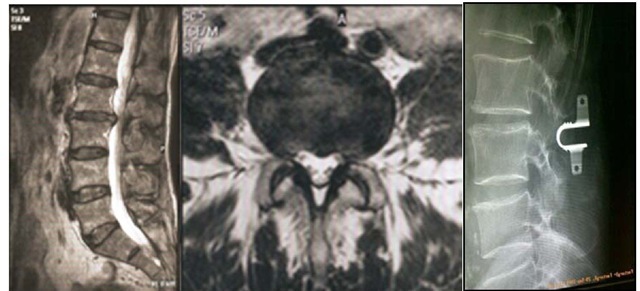
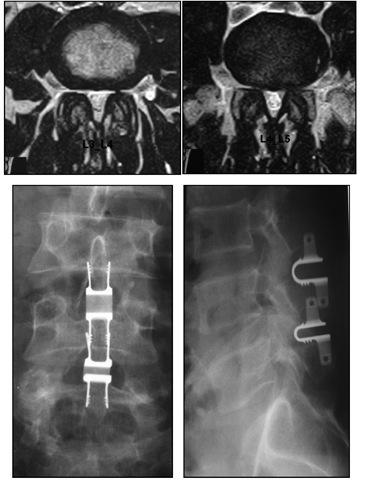
- Degenerative disk disease and subsequent bilateral foraminal stenosis (Figure 1).
Fig. 1. Biforaminal stenosis at the level of L2-L3
- Foramino-canalar stenosis, due to ligamentum flavum hypertrophy, declare symptoms consisting of bilateral lower limb paresthesia upon walking.
- Low back pain irradiating to both lower limbs due to suspended vertebra was shown mainly due to facet degenerative disease (Figure 2).
- Facet joint syndrome (Figure 3).
- Adjacent segment syndrome which refers to degenerative changes that occurs in the mobile segment next to spinal fusion (Schlegel JD, et.al 1996). It’s exact mechanism remains uncertain, but fusion technique specifically shifts the center of rotation leading to increase stress on the facets and/or disc of the adjacent mobile segment. It increases mobility of the adjacent segment, and the intradiscal pressure immediately neighboring a fused segment. And so, it can lead to disc degeneration. Finally, posterior dynamic stabilization is done to decrease and/or avoid the harmful effects of rigid fusion like, listhesis, instability, hypertrophic facet joint arthritis, herniated nucleus pulposus, and stenosis.
Fig. 2. L4 Suspended vertebra treated with 2 interspinous spacers L3-L4 and L4-L5, fixing the L4.
Fig. 3. Facet syndrome: lack of synovial fluid at the level of L4-L5 joint; a sign of degeneration.
Contra indications
- Presence of lumbar stenosis of more than 2 adjacent levels
- The level of stenosis above L1-L2 level or below L4-L5 level
- Have a fracture of the spinous process of the stenotic level
- Operated previously by a laminectomy with removal of the spinous process
- Degenerative and congenital spondylolisthesis
- Osteoporosis defined by the WHO as thinning of bone tissue and loss of bone density over time
Hospitalization and follow up
In our institution, patients are admitted for 24 hours before the day of the procedure. In pre-op, the patient is asked to hold anti-platelets and other anti-coagulation for 5 days. Only LMWH can be tolerated up to 12 hours before the procedure.
Post op, spinal cord X-ray of the operated region is done. The patient is ambulated with abdominal belt for 1 month.
Usually, the patients had regular follow up at 1, 3 and 12 months.
Biomechanics of interspinous spacer:
Several models of interspinous distracter (ISD) have been proposed to stabilize the spine tolerating in the same time a certain degree of mobility of the concerned motion segment and preserving the adjacent segment from later damage. Biomechanical studies show that those devices offer a non-rigid fixation and can return a destabilized specimen back to the intact condition in terms of motion in flexion/extension and axial rotation (Samani J, 2002; Tsai KJ et.al, 2006) . It is a biomechanical alternative to a total laminectomy with pedicle screw and rod fixation (Lee CK, 1988).
Furthermore the implant does not significantly change the intradiscal pressures at the adjacent levels, yet it significantly unloads the intervertebral disc at the instrumented level in the neutral and extended positions (Vena P et.al, 2005).
Thus the characteristics of those devices meet the profile needed for cases where minor to moderate instability is expected in the treatment of lumbar stenosis preventing as well a future deterioration of the adjacent motion segment.
Surgery
Operative technique
Preparation
The procedure is done under general anesthesia. All patients were operated in a prone position, flexed on a Wilson surgical frame with the thoracolumbar spine segment in neutral to a slightly kyphotic position, avoiding hyperlordosis for a better interspinous distraction.
Product used
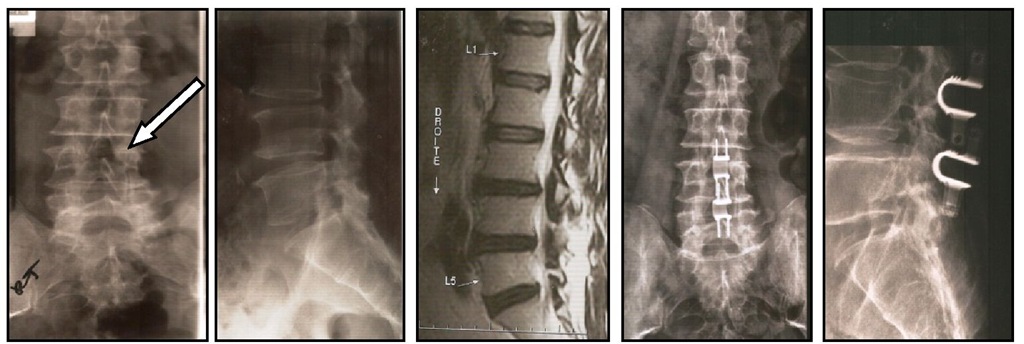
Different interspinous spacers types, the DIAM (Medtronic Sofamor Danek), the Coflex (Paradigm Spine) and The X-Stop device (St. Francis Medical Technologies), are used in our institution (Figure 4).
The instrument used
A set of lumbar laminectomy is used. In addition, a set of interspinous spacer measurer is utilized to define the depth and width of the spacer to be used.
Fig. 4. Right case of DIAM spacer. Left case of X-Stop spacer.
Operative procedure
The level of the procedure is localized under fluoroscopy after positioning. Middline vertical skin incision is done. Dissection of the subcutaneous layer and the paraspinal muscles until identification of the articular facets.
The decompression of the neural elements for stenosis is made through surgical interlaminar fenestrations with flavectomy and opening of the lateral recess, and not by the old-fashioned laminectomy. For the insertion of the ISD the interspinous ligament is resected with temporary disinsertion and retraction of the supraspinous ligament.
Adequate preparation of the interspinous space; removal of all soft tissues and flattening of the bony walls to a straight parallel nidus were ended with an adequate insertion.
Proper depth of the incorporation of ISD was determined following direct spacing of 3-4 mm between the deepest point of the device and the dural sac placing through that space a midsize hook.
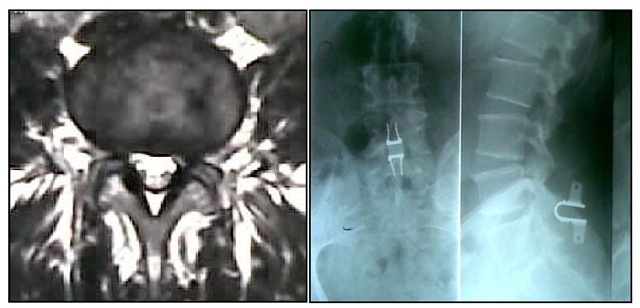
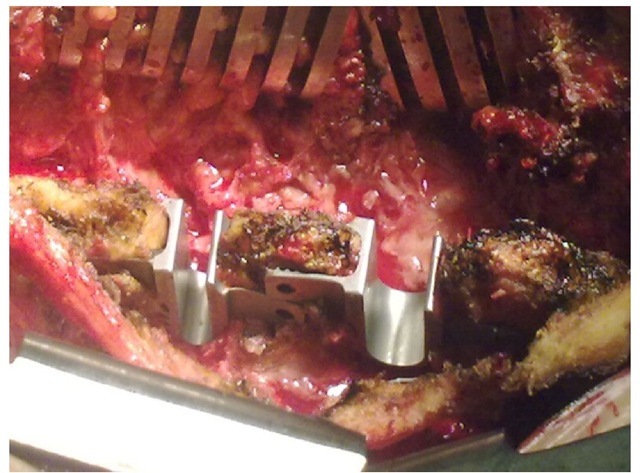
One or two interspinous spaces were treated according to the preoperative plan. ISD were inserted, the laterally retracted supraspinous ligament was always stitched to its initial location at the top of the spinous processes (Figure 5).
Discectomy is performed in cases where the protruded/ herniated disc is still compressing the root(s) despite the ligaments resection and the bone recalibrations are done. In cases where the disc is protruded/ herniated, medially dissectomies was not done.
Regular closure of layers and placing of deep hemovac drain ended the surgery.
Post-operative care
The patient is out of bed the day after surgery and discharged on day 3 after surgery, or on day 2 when drain was not inserted.
Fig. 5. Interspinous distracter implanted between spinous processes L3-L4 and L4-L5, the desinserted and retracted laterally supraspinous ligament, will be sutured to its initial place.
Control lumbo-sacral x-ray is done in 2 views to evaluate the created distraction. All patients were put in a lumbar brace, for a period of one month during their daily activities (Figure 6).
Long term results
Overall improvement was noted in ISD-treated patients, with considerable satisfaction in 75 % of patients on average. The patient at first reported an improvement of their radicular pain with a mean reduction of 3/10 on visual analog scale (VAS) (scale for 0: absent pain to 10 severe intolerable pain necessitating Intra venous treatment). In the pre-operative, radicular pain when existent had a mean score of 8.3/10 on VAS. Whereas, in the immediate post op period, the pain was at 4.9/10 on VAS.(Table 2).
Postoperative walking distance progressively increased during the next 3 months. Patients achieved maximum improvement after an average period of 6 months, with a mean score of 2.1/10 on VAS, and up to 45% of patients were pain free.
The prominent characteristic of this surgery is a low level of postoperative pain.
Fig. 6. Top: Bi foraminal stenosis more so at the level L4-L5 then at L3-L4 levels. Bottom: X-ray of adjacent interspinous spacer.
|
Cases |
Improvement after treatment with ISD |
|
Bi-Foraminal stenosis |
73 % |
|
Lig. flavum hypertrophy |
83 % |
|
Suspended vertebrae |
67 % |
|
Facetar syndrome |
66 % |
|
Adjacent syndrome |
96 % |
Table 2. Percentage of improvement in each case.
In postoperative scanning follow-up of the patients examined, a mineralization of the spinous process in contact with the implant was found, in particular at its base which appears to absorb high stresses due to lordosis (Sawnson KE et. al, 2003).
Patients are improved in all their clinical aspects: low back pain, radicular pain and walking distance. Moderate to severe low back pain improved in 75% of patients, leg pain and claudication were improved in 87% and walking distance improved in 74% of the patients (Park S-C et.al, 2009). Patient satisfaction is 89%. These results were achieved by 1 year and did not deteriorate over the long-term.
As described above the procedure has minimal post-operative back pain. And so, after the decompression done by removal of ligamentum flavum and the re-establishment of normal dynamics of the spine play a major role in the resolution of back pain. Restoration of the height of the intervertebral disc relieve the pressure on the sino-vertebral nerve which plays a major role in decreasing paraspinal muscles spasm and though the back pain. In general, back pain evaluated by the VAS with a mean score of 8.2/10 preoperatively resolves in 78 % of patients immediately.
Complications
In general, material are well tolerated. The rate of complications is between 1 and 10 % over all. Two sets of complications exists; the early and the delayed.
Early complications include device dislocation/ malposition, spinous process fractures, erosion of the spinous process, infection, hematoma, and neurological sequelae.
One case of migration was observed in one series (Dieter A et.al, 2007). There were no broken or permanently deformed implants in all series.
How to avoid complications 3.8.1.1 Fracture of the spinous process
A potential complication of placement of an ISP device is fracture of the spinous processes, particularly related to osteopenic patients.
In our experience, we do osteodensitometry for all patients to assess bone density in pre-op. During operation, we should avoid bone erosions of the adjacent spinous processes.
Intraoperative spinous process fracture occurred in < 1% of all cases.
Patient with the delayed spinous process fracture at more than a year had what has recently been referred to as a "sandwich phenomenon" fracture of the middle spinous process in adjacent double-level ISD placement.
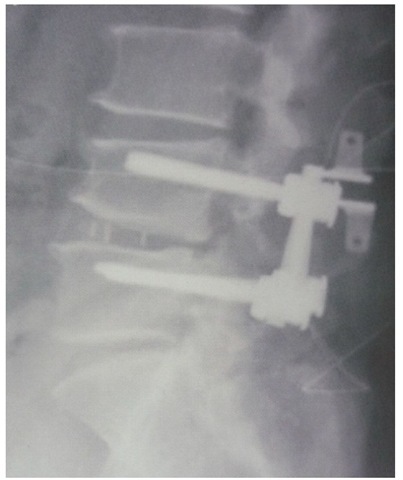
Neurological manifestations and reoperation
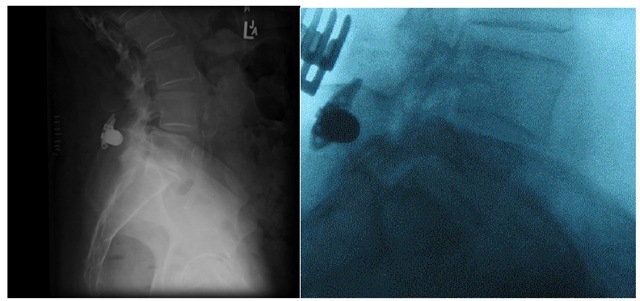
Recurrent symptoms required reoperation, microsurgical decompression and posterolateral fusion in 1.2% of cases (Figure 7).
To avoid this type of complications, a complete posterior decompression through ligamentum flavum excision and discectomy in the presence of herniated disc should be done.
Selection of patient without spondylolysthesis is mandatory to avoid postero-lateral fusion later on.
Fig. 7. Adjacent segment syndrome treated by interspinous distracter
Conclusion
Interspinous spacer after surgical decompression for spinal stenosis by excision of Ligamentum flavum demonstrates excellent short term and long term results for improvement in back pain, neurogenic claudication and patient satisfaction. It provides restoration of disc height and reduction of vertebral slip. It helps in restoring normal lumbar mobility and decrease nerve roots compression. It offers an alternative to rigid stabilization for lumbar stenosis with mild to moderate instability. If indicated, its use is favored compared to rigid stabilization because it preserve motion and has less harmful effect compared to the risk of failed back syndrome.