Introduction
Conservative treatment is the "gold standard" treatment for low back pain, in spine degenerative conditions. However, in cases where there is a failure in conservative measures, surgical treatment becomes an option (Roh et al, 2005). These procedures traditionally included decompression of spinal elements, correction of deformity and arthrodesis of the diseased spinal segment but, in some conditions, they both may be used in a combined manner (Schwarzenbach et al, 2005).
The technique of fusion with the use of only bone graft was first reported by Hibbs and Albee in 1911 (apud in Huang et al, 2005), for prevention of progression of Pott disease. Pioneers in using metallic instrumentation for stabilization, associated with bony fusions, were Harrington (1976) for scoliosis surgery, Roy Camille (1979) and Steffe (1986) with screw-plate system, Magerl (1984) with external fixation for frature treatment, and Dick (1985), with the internal fixator (apud in Schwarzenbach et al, 2005). Since then, lumbar fusion became the "gold standard" surgical treatment for a wide range of painfull conditions. The primary goal of lumbar stabilization is to treat pain from disc or facet, in the instable spinal unit. In these cases pain emerges apparently under load (Christiansen et al, 2004).
However, no surgical treatment is perfect. Christiansen and coworkers (2004) obtained positive results in approximately 70% of cases of fusion surgery. An important complication, in the medium-term follow-up, is degeneration of the disc, adjacent to a fusion segment (Rham and Hall, 1996), known as adjacent disc degeneration (ADD). In this study, ADD occured in 30% of cases, five years after fusion. Articular hypermobility in the segment above fusion segment was reported by Luk and collaborators (1987) in 50% of cases, of which 30% had also stenosis of the spinal canal.
Another post-operative complication, related to fusion, is pseudoarthrosis, compromising the final result of the surgery (Kornblum et al, 2004). In order to achieve good results in fusion, consolidation of the bony fusion is critical (Butterman et al, 1998). However, a study of Muholand and Sengupta (2002) noted that bony consolidation, with achieved fusion segment, does not represent necessarily a clinical success.
Rham and Hall (1996), in their study, also demonstrated that, in pseudoarthrosis, micromovements in the facet joint preserves hypermobility in the adjacent segments, acting like a "protective factor for the development of the adjacent segment degeneration". This finding was also described in 2004 by Ghiselli and collaborators.
With all these evidences, nonfusion techniques arise, aiming the prevention of ADD, and the fact that this new technology does not require bone graft, since these techniques don’t depend on bony consolidation.
The lumbar stability
In 1990, White and Panjabi defined instabillity of the spine as "the loss of the spine’s ability to maintain its patterns of displacement under physiologic loads so there is no initial or additional neurologic deficit, no major deformity, and no incapacitating pain".
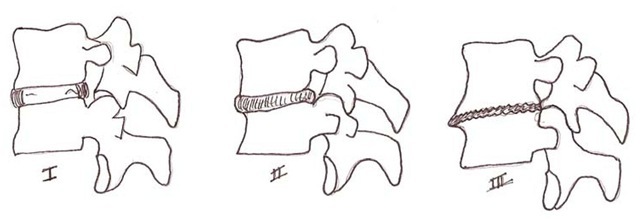
The importance of lumbar stability was originally established by Kruton (1944). Morgan and King (1957) reported that instability was a primary cause of low back pain. The degenerative process of the lumbar spine was better understood after studies of Kirkaldy-Willis and coworkers (1978), and the development of the disease was described later by Kirkaldy-Willis and Farfan (1982), using a concept of three phases: 1) temporal dysfunction, 2) unstable phase, and 3) restabilization. In the last phases, 2 and 3, patients often have stenosis, or deformities, like degenerative scoliosis, often requiring surgery for stabilization, decompression and/or correction of the deformity. (Figure 1)
Fig. 1. The degenerative cascade described by Kirkaldy-Willis and Farfan (1982). At the third phase, the disc lost height and facet hypertrophy promotes segment stabilization, but also narrowing the neural foramen and the vertebral canal (stenosis)
The intervertebral disc plays the most important role in spine stabilization (Roh et al, 2005). Disc degeneration is a physiological process with aging. The extracellular matrix structure changes, mainly in proteoglycans concetration at the nucleus pulposus, leading to disc dehydration causing, because of that, morphological changes in the disc (Biyany et al, 2004). With these changes, biomechanical function of the disc is altered, and the load in this dysfunctional disc starts to injury other structures, such as the endplates, the facet joints and the fibrous annulus (Bernick et al, 1991). Additionally, these degenerative changes can cause a number of effects in the spine and nerve roots. Protrusion or disc herniation can cause radicular compression, central stenosis and considering that there are nociceptors located there, it will, as well, lead to low back pain (Roh et al, 2005).
The basic functions of the spine are: to provide stability, giving mobility to the body, to protect the spinal cord, and to control neural information in order to move the upper and lower limbs (Harms and Tabasso, 1999). For this reason, this architecture has passive elements (bones, joints and ligaments) and active elements (muscles).
Therefore, the spinal stabilizing system consists of three subsystems: spinal column, muscles surrounding the spine, and motor control unit. The spine carries load, and provides information about position, motion and loads of the spinal column (proprioception). With this information, the control unit turns it into action by the muscles (active elements), which must provide dynamic changes in the spinal column, altering the spinal posture and loads (Panjabi, 1992).
Biomechanics of the degenerated spine
Biomechanics of the spine is not simple, because it involves complex movements of flexion, lateral inclination and rotation, and the combination of all these movements. As the spine has a huge amount of spinal units, which provide the movements, its center of rotation is not static. As movement changes, the center of rotation changes as well, and so does the loading on the spine structures, having different points of axial load in the same functional unit, with focus in the intervertebral disc and facet joints (Lumsden et al, 1968). This mobility is possible due to the possibility of intervertebral disc deformation, but is limited by the disc architecture, vertebral body, and the structures in the posterior arch (Harms and Tabasso, 1999).
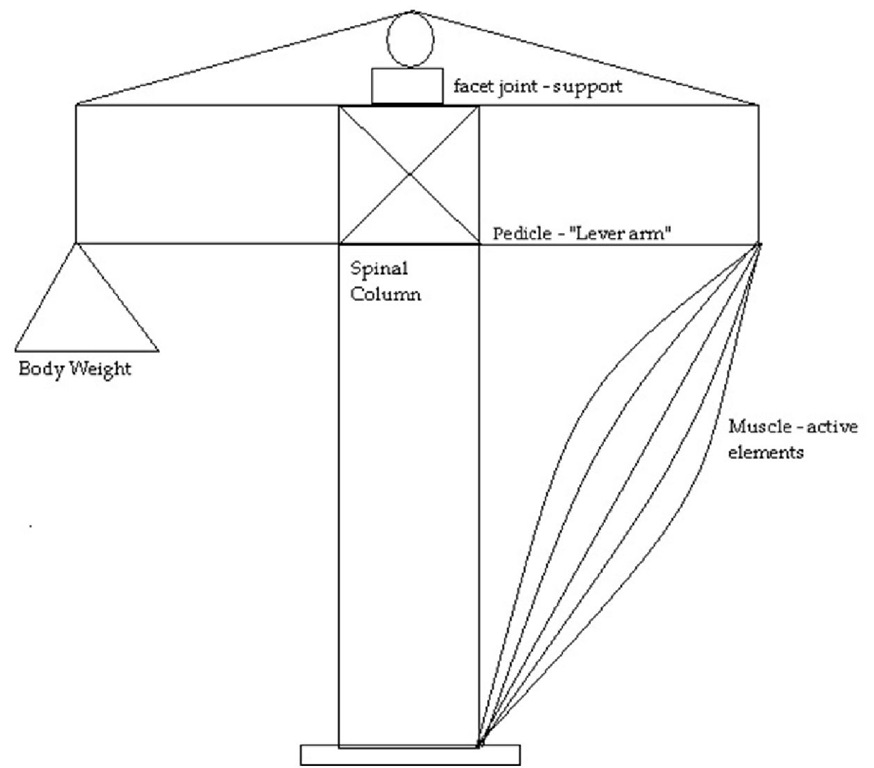
Fig. 2. The "crane", of the lumbar stability. To be stable, all the elements, active and passive, must be intact.
For Better understanding, we can imagine the spine as a crane (Figure 2). In standing position, the body center of gravity is located anterior to the spine, anterior to the vertebral bodies and intervertebral discs. Thus, an axial load is distributed as an axial compressive load in the anterior column, holding 80% of the axial load, and the remainig 20 % as a shear force in the posterior column (Harms and Tabasso, 1999). So, the anterior column receives loads primarily by compression forces, and the posterior column also resists stretching, torque and tilt. Due to these characteristics, the anterior column acts like a distraction device, and the posterior column as a tension band (Harms and Tabasso, 1999). The tensile forces in the posterior columns are actively made by the muscles, and supported by the facet joints and ligaments. The lever arm of this stabilization system depends on the pedicular sizes, influencing in the effectiveness of the posterior musculature (Harms and Tabasso, 1999).
The function and effectiveness of the posterior elements to provide stability depends on the integrity of the anterior column (Harms and Tabasso, 1999). Kirkaldy-Willis and Farfan described this degenerative cascade (1982), the degeneration of the disc (anterior column) causing an overload in posterior elements, thus inducing a degeneration of muscles and facet joints.
Modic (1984, 1991), using Magnetic Ressonance Imaging (MRI) studies, described degenerative changes in the intervertebral disc, with overload to the endplates (Figure 3). Biomechanical failure on the facet joints, and muscular failure, with overload to the endplates, leads to a noceceptive pain (Kusslich et al, 1991), and the progression of the disease leads to cyst formation on the facets, hypertrophy, with narrow disc space, that can cause central or foraminal stenosis (Dubois et al, 1999).
Fig. 3. The overload in the endplates, caused by disc degeneration, induces changes in the MRI. A) Modic type 1, the endplates are black in T1 incidence and white in 2 incidence (edema). B) The enplates are white in both T1 and T2 incidences (fat). C) The endplates are black in both incidences (sclerotic).
Albert and Manniche (2007) demonstrated, in a randomized controlled trial with 181 patients, that Modic changes type 1 is more strongly associated with non-specific low back pain than Modic changes type 2. They also suggested in this study, that disc herniation is a strong risk factor for developing Modic changes in the same level, during the following year (Albert and Manniche 2007).
The adjacent segments
Over the years, the "gold standard" technique to treat severe degenerative lumbar spondylosis has been spinal fusion (Lehman et al 1987, Ko et al 2010). However, since the beginning of this use, the damaging effects of creating rigid segments in the spine, with overload to the adjacent levels (transition syndrome) have been discussed (Fymoyer et al, 1979, Stokes et al, 1981, Aota et al, 1995, Rahm et al, 1996, Christiensen et al, 2004, Fritzel et al, 2003, Cheh et al, 2007, Kumar et al, 2001, Wiltse et al, 1999, Miyakoshi et al, 2000, Lee et al, 1988, Min et al, 2008, Yang et al, 2008, Korovesis et al, 2009).
No surgical technique is perfect, even in this "gold standard" method, patients are subject to a number of short and long-term morbidities. The relative immobility of fused spinal segments transfers stress to adjacent segments, leading to acceleration of adjacent level degeneration, because the sagital alignment of a fused spinal segment is fixed and cannot adapt to variations in posture (Weinhoffer et al, 1995).
A series of studies have shown, in cadavers and in vitro, that fusion increases intradiscal pressures, end plate stresses, and annular stresses at adjacent segments (Lee et al, 1984, Weinhoffer et al, 1995, Cunningham et al, 1997, Rohlman et al, 2001, Eck et al, 2002, Rao et al, 2005, Sudo et al, 2006). The restricted motion in the fused segments, in a active body, having fixed sagittal alignement, increases motion and stress at adjacent levels, in sitting, supine and erect postures (Huang et al, 2005).
This stress doesn’t lead to hipermobility in the adjacent levels after fusion since degeneration progresses. Avoidance of hypermobility at the adjacent levels is frequently attributed to nonfusion technology. A few studies already reported about such an effectiveness of dynamic stabilization techniques (Olsewki et al, 1996, Phillips et al, 2002, Shono et al, 1998, Panjabi et al, 2007).
The incidence of adjacent disc degeneration is not clear. But, it has shown clinical evidence. Sears and coworkers (2011), in a retrospective cohort study, associate the risk of a new surgery for adjacent level degeneration with the number of levels fused. They concluded that, although young patients who underwent single-level fusions are at low risk, patients who underwent fusion of three or four levels had a threefold increased risk of further surgery, compared with single-level fusion, and a predicted 10-year prevalence of 40%.
Szpalski and coworkers (2002) published a comprehensive review of nonfusion implants, which comprises posterior dynamic stabilization, interspinous devices, and total lumbar disc replacement. The potential reduction of the adjacent disc disease is mainly attributed to the avoidance of increased stress at the adjacent segments. Such increased stress is anticipated in instrumented fusion procedures, leading to hypermobility at the adjacent segments. Shono and coworkers (1998) demonstrated that hypermobility at the adjacent levels was proportional to the length and rigidity of the instrumented constructs.
When is surgery necessary?
Low back pain is the first symptom of disc degeneration. The degenerate intervertebral disc is associated with structural failure, with radial failures, prolapse, endplate damage, annular protrusion, internal disc rupture, and disc space narrowing (Dubois et al, 1999, Schnake et al, 2006). Especially the discs, posterior and capsular ligaments, as well as the vertebral endplates have been found to be the major sources of nociception leading to pain (Kusslich et al, 1991). With the progression of the disease, hydration of the nucleus pulposus decreases, and this composition alters, leading to loss of dic height and reduction of its intradiscal pressure. As described by Kirkaldy-Willis (1982), this cascade evolves, leading to overload the annulus fibrosus and the facet joints. Loading with inadequate nuclear turgor leads to shearing forces in the transitional zone between the nucleus and annulus (Huang et al, 2005). As a result, we have ruptures and radial tears in the annulus fibrosus, and overload of the facet joints. This change leads to instabillity. In addition to disc protrusion toward the spinal canal, disc height decreases, and there is spinal canal or neural foramen stenosis, that leads to radicular pain (Yu et al, 1988, Urban et al, 2003).
Pain from degenerative diseases may arise from stenosis, facet overload, the disc itself, and eccentrically loaded vertebral endplate. In patients with radicular pain, secundary to radicular compression, consequece to disc prolapse, surgical procedures have to be carried out, if the conservative therapy fails. However, operative treatment, like discectomy or nucleotomy, leads to progression of the disc degeneration (Dunlop et al, 1984, Gottfried et al, 1986, Brinckmann et al, 1991). In 2004, Jansson and collaborators published that approximately 10% of all operated discs reherniate and approximately 27% of all operated patients have to undergo a second operation within 10 years.
Nonsurgical management must be considered, in low back pain, especially in patients without radicular compression signs.
Stabilization devices leave the pain-generating disc tissues in situ, but restrict certain types of motion and alter load transfer through the functional spinal unit (Huang et al, 2005). Fusion implants are designed to unload the disc and facets by load sharing.
In 1954, Verbiest described the so called neurogenic intermittent claudication secundary to lumbar spine stenosis. Recent studies show that clinical or nonsurgical tratment have poor results comparing to surgical procedures (Weinstein et al, 2008). Surgical trearment based on decompression alone presented poor results, related to progression of symptoms and deformity (Hanley et al, 1995). At the same time, adding an arthrodesis to the decompression procedure increases the operative time and blood loss, and consequently the complication rate (Di Silvestre et al, 2010).
Nonfusion techniques: Advantages and disadvantages
For many years arthrodesis has been acknowledged as the gold standard treatment for a wide variety of spinal pathologies such as deformities, unstable and painful conditions of the lumbar motion segment (Mayer et al, 2002).
Nevertheless, spinal fusion in degenerative disc disease when there is no instability or disturbed curvature, though often performed, is not a consensus among the spinal community (Greenough et al, 1994, 1998, Kozak et al, 1994, Mayer et al, 1998). In most cases, there is indication of arthrodesis when all kinds of conservative therapies fail.
However, the results seem to not always justify these decisions (Mayer et al, 2002). Fritzell and coworkers (2003) observed a 12% 2-year incidence rate of major complications following lumbar arthrodesis, with a reoperation rate of 14.6%. Complications include pseudarthrosis, bone graft donor site pain, instrumentation failure, infection and simple failure to relieve pain (Frelinghuysen et al, 2005, Tropiano et al, 2005). Not to mention the possibility of an adjacent segment degeneration, which have made spinal surgeons think of an alternative method that could avoid such complications (Rham et al, 1996).
It’s important to mention that there are increasing numbers of patients who have undergone spinal fusion for degenerative disc disease with images showing adjacent level degenerative changes, but not necessarily with a strong clinical impact. In a long term follow-up of 30 years, there was a significantly higher incidence of radiographic changes at adjacent levels after lumbar fusion, but this was not accompanied by a significant change in the functional outcomes (Kumar et al, 2001).
Non fusion technologies in spine surgery are being developed to address the arthrodesis’ disadvantages (Jansen and Marchesi, 2008).
Non fusion implant types include total disc replacements, prosthetic nuclear implants, and posterior stabilization devices.
Potential advantages of nonfusion implants (Mayer et al, 2002, Huang et al, 2005):
1. Elimination of the need for bone graft.
2. Reduction in surgical morbidity
3. Elimination of pseudarthrosis
4. Reduction of adjacent level degeneration
Pseudarthrosis and the need for bone graft are truly eliminated, as well as the above mentioned reduction in surgical morbidity. Nevertheless, it is questionable whether nonfusion technologies significantly decrease the incidence of adjacent level disease, especially if segmental motion is not well maintained. Furthermore, if bone graft substitutes prove to be efficacious and economically viable alternatives to autogenous bone grafting, avoidance of autograft harvest will no longer be a significant advantage of nonfusion implants.
Potential disadvantages of nonfusion implants (Mayer et al, 2002):
1. Mechanical failure and device migration
2. Implant subsidence
3. Same level degeneration
Considering the fact that nonfusion implants are characterized by motion, therefore they are subject to mechanical failure or migration.
It is believed that subsidence is a significant contributor to poor outcomes after total disc replacements and this is probably the most significant challenge to long-term outcomes with these implants. Optimized implant design and end plate coverage may diminish the chances of subsidence happening.
The preservation of segmental motion obtained in nonfusion technology created the concept of symptomatic same level degeneration, as opposed to what is seen in a solid fusion. The possible sources of same level degeneration are the intervertebral disc, the facet joints, and the ligamentum flavum.
In conclusion, the potential pitfalls and benefits of nonfusion implants have to be carefully considered before the selection of this technology. Long-term randomized prospective studies are necessary and are currently unavailable, so non fusion procedures should be reserved for use in a small population of highly selected patients.