Introduction
The investigation of motor vehicle accidents resulting in fatality and pedestrian deaths constitutes a significant percentage of the work load of a busy forensic facility.
A firm understanding of the pattern of injury in these cases is a fundamental prerequisite and is heavily relied upon in the law courts, as frequently, the pathologist may be called to give evidence, or at the very least, to furnish a report which adequately addresses the questions posed by the investigating officers.
The purpose of the forensic pathologist in investigation of road and traffic fatality is as follows:
1. to establish the cause of death;
2. to determine the pattern of injuries;
3. to note the presence of any natural disease;
4. to determine the role (if any) of alcohol or drugs;
5. to report these conclusions based on a full examination.
In many cases the cause of death is self-evident. Frequently, after high speed collision, the body incurs extensive trauma and disruption. In many cases, however, the external examination fails to disclose an adequate cause of death, or at the very least, provides evidence of minimal trauma. It is fundamental that a definitive cause of death be provided and it is only after the completion of an adequate autopsy that this requirement is fulfilled. The determination of the pattern of injuries is crucial in the reconstruction of the series of events leading to the fatality. This information is relied upon heavily by trained investigating officers and may be crucial at the time of a coroner’s investigation or possibly the hearing of cases in the higher courts.
The presence of significant naturally occurring disease must also be disclosed, as a small number of cases of road trauma resulting in death may be directly attributed to an overwhelming medical event. In these cases, the event is frequently witnessed, either by a passenger or by a pedestrian or driver nearby. Frequently, the vehicle is seen to waver or lose control and not infrequently, the driver is able to pull the car over to a safe position at the side of the road prior to collapse or death. In these cases, the cause of death is not infrequently one of cardiovascular origin, but in other cases, the disease process may be more obscure.
Of great significance in the investigation of road fatality is the role of alcohol, on its own, or in combination with drugs, prescription or otherwise. Of increasing significance today is the influence of illicit drugs such as the opioids and cannabinoids.
The final written report must include an adequate list of injuries and the influence of these injuries on the organ systems, comment regarding the presence of natural disease and the influence of alcohol or drugs, if any. It is this final report that is used by the coroner or medical examiner and its worth is dependent on the skill of the pathologist in charge of the case.
The ideal situation would dictate that the forensic pathologist attend every road fatality. Clearly this is not feasible given the number of fatalities per annum and the number of pathologists employed in a given metropolitan institution. Interpretation of injuries, however, is often facilitated by a personal visit to the scene or inspection of the vehicle or vehicles involved. Failing this, the inspection of the scene photographs is often invaluable.
The pattern and severity of injuries are essentially dictated by:
1. the direction of impact;
2. the design of the cabin;
3. the force of the impact;
4. the behavior of the vehicle after the impact;
5. whether the driver/passenger was injected from the vehicle;
6. whether a restraining system was in use (seat belt or airbag);
7. whether death may have been compounded by a factor such as fire or inhalation of toxic fumes.
The injury pattern may, for simplicity, be divided into those seen in drivers and passengers.
Driver Injury
In the event of a high speed head-on collision, in addition to rapid deceleration, the car frequently dips, causing the driver to slide forward into the steering column and at the same time, elevate, allowing the head to impact with the fascia. This complex movement results in flexion of the cervical and thoracic spines and at the moment of contact with the head to the fascia, lead to compression of the axial spine. The axial compression may be such that the pelvic girdle may fracture. The driver, frequently being aware of the impending situation, may adopt a ‘bracing posture’. The bracing posture is typified by outstretched forearms and a gripping action on the steering wheel, together with a forced rigidity and straightening of the braking leg.
As seen with axial spinal compression, the force may be transmitted from the braking foot, through ankle, leg and ultimately into the acetabulum and pelvis. This pattern of fracture is frequently invaluable in determining driver from passenger when both parties are ejected from the vehicle and particularly, when restraining devices are not used.
Variations on the classic injury pattern may be caused by intrusion of various vehicle parts into the cabin such as the engine, steering column and firewall.
In the situation of rear impact at speed, the cervical spine may undergo severe hyperextension and then later, deceleration with hyperflexion. This complex range of movements may cause substantial trauma to the spinal cord and supporting axial spine and musculature.
Side impacts may show any combination of the above.
Who Was the Driver?
To discriminate driver from passenger in a scenario where restraining devices have been employed, a dedicated external examination is required to disclose the typical distribution of bruising and abrasion caused by lap/sash belts. In many cases, the bruising is immediately apparent, but in others, subcutaneous dissection may be required to disclose points of maximal contact and pressure (Fig. 1).
As suggested earlier, frequently the driver is aware of the impending situation whereas the passenger is often oblivious. The presence of bracing type leg fracture and/or pelvic fracture may adequately discriminate between driver and passenger. Indeed, the bracing actions may well be demonstrated in the driver at the level of forearm, wrist and shoulder whereas this pattern may be entirely absent in passengers.
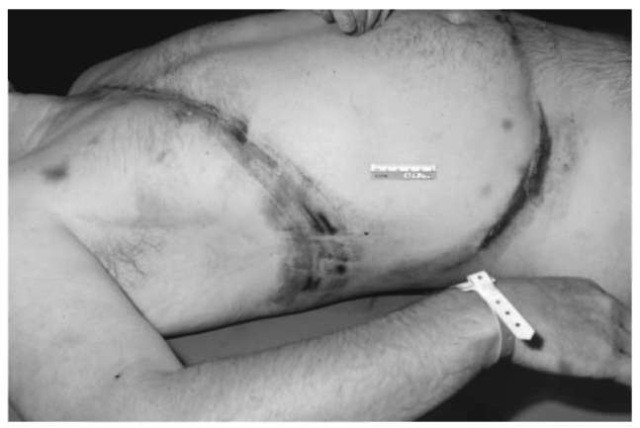
Figure 1 Typical lap/sash passenger distribution of bruising and abrasion.
A dedicated examination of the deceased (and clothing) by a crime scene investigator may be rewarding. The discovery of glass, automotive paint, plastic and fabric may help to accurately place the deceased in the vehicle, and therefore assist in discerning driver and passenger.
Pedestrian Death
Pedestrian fatalities may account for more than 50% of all road-related deaths. Many texts have classified the pattern of injuries seen in pedestrians into primary and secondary. The primary injury is defined as the injury caused by the first impact of the vehicle on the victim whereas the secondary injury is caused at the time of impact with the ground. Other texts have referred to primary, secondary, tertiary and quaternary injuries. This rather complex classification may suggest to coroner or barrister that these injuries are easily discriminated and therefore, at the time of the inquest, may be frankly misleading. This classification discriminates the injuries thus as follows.
1. The primary injury is caused by initial impact with the vehicle.
2. The secondary injury is caused by the initial impact with the vehicle once the body has been propelled on to it (i.e. onto the bonnet or windscreen).
3. The tertiary trauma is caused by contact with the ground after the body has left the vehicle.
4. The quaternary injury is caused by further vehicles traveling in either the same or opposite directions.
It is often not fully appreciated that in many cases, after impact with a conventional vehicle, the victim is ‘scooped’ up onto the bonnet and then despatched to the ground either across the bonnet or over the roof towards the rear of the vehicle. This scenario is especially pertinent in cases where application of the brakes by the vehicle immediately prior to collision has caused the front end to dip somewhat.
Naturally, larger vehicles such as vans and trucks tend to impact on the victim in a full frontal fashion leading to a forward propulsion. The victim may then go under the vehicle and be crushed by the wheels or damaged by protruding parts of the vehicle. This rather simplistic outline needs to be tempered with the consideration of the height of the victim (i.e. adult or child).
Leg trauma is identified in approximately 85% of pedestrian fatalities. Indeed, 25% of fatal outcomes disclose evidence of compound fracture to tibia and/or fibula. The classic texts frequently describe fracture patterns which are purported to indicate the activities of the victim immediately prior to impact. It is said that if the fracture is oblique in orientation, it indicates weight bearing at the time of impact. A transverse fracture is said to indicate a nonweight-bearing state. By inference, if the points of fracture are at different levels it would suggest that the victim was either walking or running prior to impact. The point of a fracture wedge (often seen on a radiograph) is said to indicate the direction of force.
In reality, the fracture patterns may be complex and therefore do not readily lend themselves to such a simplistic approach. It is suggested that over-interpretation of fracture patterns may, in many cases, be misleading and therefore counterproductive. Additional autopsy techniques are often required. Measurements of the distance from heel to level of abrasion/laceration and fracture line may assist in the estimation of the bumper bar height. Subcutaneous dissection of the lower extremities frequently discloses a zone of hemorrhage at the point of impact, and this can readily be measured from the heel. Subcutaneous dissection of the back may also be required.
Motor Cycle Fatality
The motor cycle fatality may constitute approximately 10% of all road casualties. A review of motor cycle-related injuries in children and adolescents, funded by the Victorian Health Promotion Foundation and Accident Research Centre cited ten factors implicated as contributing to fatality.
1. Being male
2. Being young
3. Being inexperienced
4. Being unlicensed
5. Riding on a borrowed motor cycle
6. Consumption of alcohol
7. Riding in peak hour
8. Negotiation of curves
9. Slippery or uneven surfaces 10. Poor motor-cycle maintenance
The majority of motor cycle accidents appear to occur in the daylight hours (65%). The engine capacity was deemed to be a significant factor with 54.6% of fatalities involving motor cycles with an engine displacement of 250-500 cc.
As would be expected, trauma to the head, chest and abdomen is commonplace. However, a frequently overlooked and unsuspected facet of injury in motor cycle riders is one of cardiac trauma. One study reviewed 546 autopsies in patients who had incurred nonpenetrating traumatic cardiac injury. All of these patients were deemed to have died from their cardiac or associated injuries and of the 546 cases, 64.6% died from cardiac rupture. Of these, 30% demonstrated multiple chamber rupture and the remainder were associated with rupture of the aorta.
Patients incurring such injury may present with alterations of the ECG, myocardial failure, cardiac tamponade or hemothorax. These injuries may present without obvious rib fracture or chest wall deformity and therefore may elude primary diagnosis.
Rupture of the right atrial appendage is not uncommonly demonstrated in blunt trauma to the chest and abdomen. (Fig. 2). The underlying cause for the traumatic disruption of the thin-walled right atrial appendage is deemed to be a ‘water hammer’ like column of blood, the pressure being generated by blunt compression of the inferior vena cava and viscera leading to sudden and catastrophic distention, and ultimately, disruption of the appendage.
Trauma to the head and neck is a frequent and significant injury type, constituting over 50% of all road traffic accidents. The trauma ranges from relatively minor, in the form of laceration or abrasion, to simple or complicated forms of skull fracture. The hinge-type base of skull fracture is commonly seen as a sequel to blunt lateral head impact (Fig. 3).
The cervical spine may be traumatized leading to dislocation of the atlanto-occipital joint, brainstem injury, frank fracture, pontomedullary rent or disruption of the vertebral arteries. The latter may lead to significant basal subarachnoid hemorrhage.
Thoracic trauma may constitute frank cardiac rupture, cardiac contusion, hemopericardium, traumatic rupture of the aorta (particularly of the distal arch segment), hemopneumothoraces, rib fracture (frequently a flail segment), pneumothorax, pulmonary laceration and contusion and disruption of the hilum.
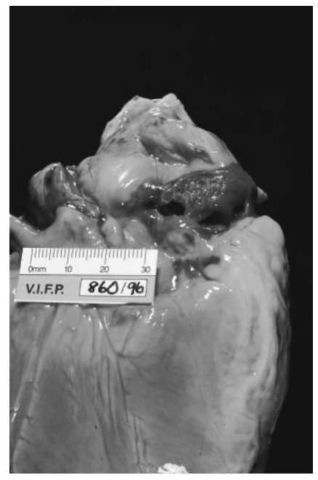
Figure 2 Rupture of the right atrial appendage.
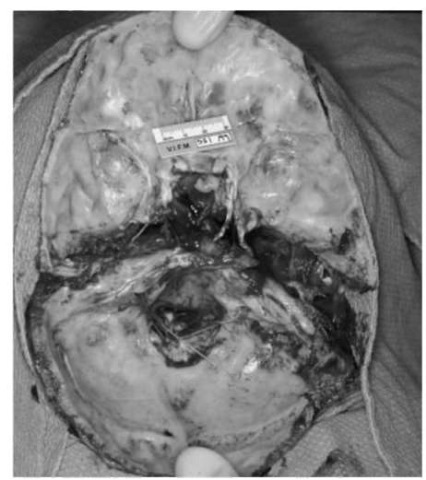
Figure 3 Hinge-type base of skull fracture commonly seen as a sequel to blunt lateral head impact.
Abdominal injuries, in order of frequency, constitute laceration or contusion of liver, spleen, kidney, mesenteries, pancreas, gut and diaphragm. A significant number of cases may manifest as delayed rupture of the spleen, leading to catastrophic hemorrhage days or possibly weeks after the event.
Pelvic injury may be incurred as a result of direct trauma to the pelvis either by anterior impact or transmitted force from fractured femora. A fractured pelvis may lead to rupture of the urinary bladder and intense hemorrhage as a result of torn iliac vessels. This particular form of trauma carries a significant morbidity and mortality.
Complicating Factors
A small but significant number of fatalities may be directly related to causes other than immediate physical trauma at the time of impact; for example inhalation of carbon monoxide or cyanide which may be liberated from combustion of synthetic materials in the cabin. Traumatic asphyxia from compression of the chest by steering column or overturned vehicle is occasionally encountered.
In many cases, the ultimate cause of death may be thermal injury. Evidence of sustained respiration in these cases may be demonstrated by the presence of black particulate material within the major airways and further verified by analysis of carboxyhemo-globin in postmortem blood specimens. In cases of explosion or flash fire, such findings may be absent.
In many cases, an autopsy is requested on a person who has sustained trauma but survived for a time in hospital or convalescent home. These often constitute common entities such as pneumonia, or the effects of fat embolism syndrome. Rare cases may include cardiac fibrosis and arrhythmia secondary to healed cardiac contusion.
Pre-existing Disease
The rare and problematic cases constitute those of pre-existing natural disease. These cases account for approximately 1% of fatalities overall and are often typified by death behind the wheel with minimal apparent external evidence of trauma. The event is often witnessed and the collision, if any, is at low speed. These fatalities may disproportionately represent the older population and in many cases, significant medical and surgical disease is well documented. Direct communication with the treating medical practitioner is often very rewarding.
Such conditions may include acute myocardial infarction in a person with known significant coronary artery disease, a cerebrovascular accident, transient ischemic attack or more uncommonly, diabetes or epilepsy. The diagnosis of epilepsy must be based on a confirmed antemortem diagnosis unless a definitive anatomical lesion can be demonstrated either macro-scopically or histologically. Epilepsy may be suspected if the deceased shows evidence of convulsion, such as biting of the tongue and incontinence. In confirmed epileptics, the presence of anticonvulsant medications must be sought and quantified.
The worth and necessity of toxicological analysis of body fluids in cases of road fatality cannot be over emphasized. All too frequently, the influences of drugs and alcohol are manifest on the roads each year. A worrying trend in road fatality now appears to be the usage of prescription medications, such as the benzodiazepine group which act in a synergistic fashion with alcohol to reduce the ability to adequately control a motor vehicle. The modern laboratory requires sampling of not only blood but bile, urine, liver, gastric content and vitreous humor for such analyses. The sampling of blood from peripheral veins is preferred as blood taken from body cavities may be contaminated by the diffusion of drugs from the gastrointestinal tract. Cardiac and cavity blood may be used for the analysis of carbon monoxide if peripheral blood cannot be obtained.
Investigation of the ‘Hit-Run’ Fatality
The hit-and-run fatality is an uncommon but highly significant event requiring ultimately a multiskilled approach to the examination, both at the scene and in the postmortem room. The conduct of the examination for the investigation of the hit-and-run fatality epitomizes the concept of the team effort.
The body should be received in the mortuary fully clothed and strict instructions should be given to the mortuary attendant that the clothes should remain in situ prior to examination by the pathologist. A full photographic profile needs to be undertaken to document the state of the clothing and in particular, trace evidence such as plastic, glass and paint. These telltale exhibits must be collected, protected and handed over to the investigating authorities with a reliable and demonstrable chain of custody protocol. The clothes may be removed and retained as evidence.
A full photographic profile of incurred injuries should be documented; particularly the use of close-up shots, with and without scale, is required. Particular note should be taken of patterned injuries such as bruises and abrasions which may provide an indication of make and model of the suspected vehicle.
The full autopsy is performed with due regard to accurate description of all injuries in relation to anatomical landmarks. The location, type, dimension and depth of all injuries need to be meticulously recorded. The autopsy may also require subcutaneous dissection of the legs to indicate accurately the level of contact with bumper bars or other protruding parts of the offending vehicle (Figs 4 and 5). Radiology may be required to document fractures not identified by open dissection. It is recommended that foreseeable problematic cases have at the very least, a radiological survey of the lower limbs. The opinion of a specialist radiologist may be required.

Figure 4 Bruising and abrasion indicating the level of contact with bumper bars.

Figure 5 Subcutaneous dissection of the legs to determine accurately the level of impact.
As indicated earlier, a full toxicological analysis of body fluids is required to demonstrate the influence of alcohol or drugs. In some cases, the absence of a particular medication may be as relevant as the presence of a drug in excess.
Conclusion
In closure, it is stressed that the forensic pathologist should impart his or her knowledge and experience to those involved in the investigation of motor vehicle and pedestrian death such as specialist police accident investigation officers and coroner’s staff. The collective experience of a forensic institute is also an invaluable resource in the teaching of undergraduate medical students and those in the legal profession.
