Introduction
The analysis of drugs of abuse in biological specimens belongs to a branch of the forensic sciences known as analytical toxicology.
Since the beginning of the twentieth century, several epidemics of drug abuse have occurred, in both eastern and western countries, but the use and abuse of illicit drugs started to become a serious problem in society around the mid-1960s, coinciding with the ‘hippy’ movement, the Vietnam War and the student revolts taking place in many countries. Drug abuse has now infiltrated other segments of the population, especially the inner cities marked by unemployment, poverty, crime and other kinds of deviant behavior. More recently, the abuse of synthetic or ‘designer’ drugs has escalated among teenagers and adolescents belonging to the rave culture. These substances include ecstasy (methylenedioxymethamphetamine, MDMA) and its analogues, which are produced at clandestine laboratories and marketed at special dance clubs and on the World Wide Web. Some of the chemical structures of these so called ‘smart drugs’ have not yet been classified as narcotics. In some countries, a fairly liberal attitude towards the sale and consumption of ‘soft drugs’, mainly tetrahydro-cannabinol (THC) derivatives (cannabis, marijuana, Indian hemp) has become evident.
Legislation prohibiting the manufacture, production, handling, sale and consumption of narcotic drugs for recreational purposes exists in most countries. Indeed, use of drugs in the workplace is now regulated by statute in the USA, which has created the need for large-scale screening of urine samples to identify the presence of psychoactive substances. Much effort has been directed towards monitoring drug abuse within the criminal justice system, that is, among prison inmates and others held in detention for various crimes. Rehabilitation of drug addicts requires regular monitoring of body fluids for illicit drugs as a means to control for relapse. Driving under the influence of drugs is another area where increasing attention is being given by the news media and government authorities charged with improving traffic safety and reducing drug-related deaths on the highway. The qualitative and quantitative identification of an abused substance in a blood sample from the person suspected of drug-impaired driving provides important prosecution evidence. Analyzing drugs and poisons in body fluids is also a fundamental element of postmortem toxicology when the cause of death has to be established, and also in emergency medicine when overdosing with drugs is suspected.
Classification of Abused Drugs
Drugs of abuse are often classified according to their chemical structure and the pharmacological effects they produce on the body, e.g depressants, stimulants, hallucinogens, and whether or not well-defined medicinal uses exist, e.g. as anxiolytics, sedatives, hypnotics or analgesics, or whether the drugs are simply taken for pleasure and to elicit feelings of euphoria. Table 1 presents examples of both licit (prescription) and illicit drugs classified according to their pharmacological effects.
Table 1 Broad classification of drugs of abuse according to their main pharmacological effect
| Pharmacological effect | Drug class | Examples |
| Central nervous system | Barbiturates | Butalbital, pentobarbital, phenobarbital |
| (CNS) depressants | Benzodiazepines | Diazepam, oxazepam, flunitrazepam, nitrazepam, temazepam |
| Opiates | Heroin, morphine, codeine | |
| Others | Ethanol, fentanyl, dextropropoxyphene | |
| CNS stimulants | Cocaine | Cocaine, ‘crack’ |
| Amphetamines | Methamphetamine, amphetamine | |
| Designer drugs | DOM, DOB, MBDB, MDA, MDE, MDMA | |
| Others | Phenmetrazine, cathinone, methcathinone, khat | |
| Hallucinogens | Phenylethylamines | Mescaline |
| Tryptamines | Dimethyltryptamine (DMT), psilocybin, psilocin | |
| Ergot alkaloids | Lysergic acid diethylamide (LSD) | |
| Cannabinoids | Hashish, marijuana | |
| Others | Phencyclidine (PCP) |
DOB, 2, 5-dimethoxy-4-bromoamphetamine; DOM, 2, 5-dimethoxy-4-methylamphetamine; MBDB, N-methyl-1-(3,4-methylenedioxyphenyl)-2-butanamine; MDA, methylenedioxyamphetamine; MDE, methylenedioxyethylamphetamine; MDMA, methylenedioxymethamphetamine.
Biological Specimens
Forensic and analytical laboratories specializing in drugs of abuse testing might receive specimens of whole blood, plasma, urine, saliva, sweat or hair as materials for analysis. In postmortem toxicology, tissue samples, stomach contents, vitreous humor and cerebrospinal fluid are also among the materials submitted for analysis. The analytical methods used are little different if the specimens are obtained from the living or from the dead, but in autopsy work the interpretation of the results requires some special considerations. Translating the concentration of a drug or narcotic measured in a blood sample obtained at autopsy into the concentration present at the time of death or the dose of drug administered is fraught with difficulties. Most forensic toxicologists consider such estimates unreliable and only general guidelines can be given. The special considerations for interpreting concentrations of drugs of abuse in postmortem specimens will not be dealt with in this section of the topic.
Drugs of abuse can be determined in either blood or urine and the choice between the two specimens will depend on the purpose of the testing. When impairment of performance and behavior resulting from taking drugs is important, e.g. in connection with drug-impaired driving, the analysis of blood or plasma specimens becomes essential. Being under the influence of drugs requires some knowledge about exposure of the brain to the psychoactive substance, and blood or plasma concentrations are therefore the closest approximation. For monitoring and control of abstinence from use of drugs, urine is the preferred fluid because the detection window is appreciably longer compared with that for analysis of blood samples. Table 2 gives the approximate detection times for being able to identify various drugs of abuse and their metabolites in blood and urine specimens.
Table 2 Approximate detection times of drugs of abuse and their main metabolites in blood and urine
| Drug | Metabolite | Blood | Detection time (h) Urine |
| Amphetamine | — | 72upto168a | |
| THC | — | <12 — | |
| Carboxy-THC | 48-168 | 168—to several weeks’3 | |
| Cocaine | — | <12 | 24 |
| Bensoylecgonine | 24 | 72 | |
| Heroin | — | < 0.5 | — |
| 6-acetylmorphine | 3 | 24 | |
| Morphine | 24 | 72-96 | |
General Procedures
Fig. 1 shows a flow diagram illustrating the sampling and processing of biological specimens for analysis of drugs of abuse, e.g. in workplace drug testing programs.
Preanalytical
Obtaining the appropriate biological specimen is not a trivial matter; when urine is collected, the sampling should be observed because drug addicts might attempt to adulterate the specimen in various ways. An appropriate volume of specimen (>30ml) is usually collected in a clean dry container without preservatives (e.g sodium fluoride), taking care to label the sample with the donor’s name, and the date and time of sampling. Special tamper-proof security tapes are available and should be used to seal the sample container prior to transport and storage in the laboratory. All these safeguards help to ensure the validity of the final analytical result. The chain of custody of biological specimens from the moment of sampling, during transportation to the laboratory and during the analytical procedure must be documented until the specimen is finally stored in a refrigerator, deep-frozen or destroyed. Chain-of-custody aspects are often much discussed and debated in connection with drugs of abuse testing, especially if the results are challenged, which often happens weeks or months after making the initial analysis.
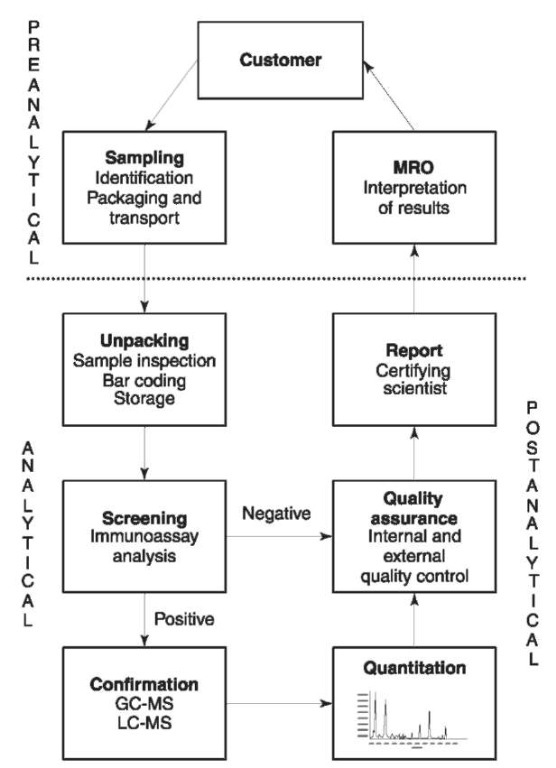
Figure 1 Scheme for obtaining and processing biological samples for analysis of drugs of abuse. MRO, Medical review officer.
In connection with urine drug testing, attempts are sometimes made to manipulate or adulterate the sample, e.g. by dilution with water or other liquids, so that the concentration of the abused drug decreases below the threshold for positive test results. Urine samples might be tampered with in vitro after voiding, by adding various chemicals or household products (soap, detergent, lime juice) to make the assay more difficult or impossible to perform, or in vivo,by drinking water or alcohol to cause a water-induced diuresis. Determination of the urine creatinine content is one method used to monitor for highly dilute specimens: cutoff concentrations of 0.2-0.5 mgml-1 (1.6-4.0mmoll-1) are generally used. The temperature of the urine immediately after voiding (32-38°C or 90-100°F), its pH (pH 5-8) and specific gravity (1.003-1.030) are other ways to control for adulterated or otherwise suspicious samples.
Analytical
The most widely used analytical strategy involves making an initial screening analysis to exclude those specimens that do not contain any drugs of abuse above a pre-established threshold concentration. The preliminary screening tests are generally performed on a specimen of urine, whenever available; otherwise a blood sample after protein precipitation can be used for analysis. The drug screening analysis is performed by means of immunoassay techniques. Several classes of drug are usually screened for simultaneously (opiates, cocaine metabolites, amphetamines, cannabinoids as well as lysergic acid diethylamide (LSD) and phencyclidine). Those specimens identified as positive during this screening test are analyzed again using a confirmatory and more specific method of analysis, such as gas chromatography-mass spectro-metry (GC-MS).
Postanalytical
Knowledge about the stability of drugs in body fluids during storage becomes an important issue whenever the analytical result has to be verified at some later date. A decrease in concentration of drugs of abuse generally occurs during storage, and data for barbiturates, benzodiazepines, cannabinoids, cocaine, LSD and phencyclidine have been published. The rate of loss of analyte seems to depend on the physicochem-ical properties of the drug, especially factors that influence binding to the container, the kind of body fluid analyzed (blood, urine or saliva), the pH of the medium and the storage temperature. Specimens stored deep-frozen will retain the initial drug concentration for longer.
Immunoassay for Drugs of Abuse Testing
Immunoassay technologies were designed to provide a cost-effective way of identifying presumptive positive specimens before embarking on a quantitative confirmatory analysis by a more selective technique. The immunoassay methods for analyzing drugs of abuse were developed primarily in connection with workplace drug testing to meet statutory guidelines. Table 3 gives the threshold concentrations (cutoff levels) for drugs of abuse in urine as recommended by the Substance Abuse and Mental Health Services Administration (SAMHSA) and the European Union (EU) for drug testing. The SAMHSA guidelines for analysis of opiates were changed during 1998 regarding the cutoff levels for positive results and also the need to identify 6-acetylmorphine as proof of heroin intake.
The basic principle of an immunoassay (IA) involves the reaction between an antibody and an antigen (the drug or its metabolites). The drug molecules in the biological sample compete for binding sites on the antibody with an antigen labeled or marked with either an enzyme (EIA), a fluorescent group (FPIA) or a radioisotope (RIA).
The enzyme multiplied immunoassay technique (EMIT) is by far the most widely used EIA technology for drugs of abuse screening analysis. The EMIT method monitors the change in absorbency at 340nm when the coenzyme nicotinamide adenine dinucleotide (NAD+) is converted to its reduced form NADH. The EMIT technology is ideally suited for use with large-scale, fully automated analytical systems that are capable of making thousands of determinations each day (e.g. Hitachi 911). The development of methods for ‘on-site testing’ of urine for drugs of abuse is currently in vogue. Small handheld devices containing the antibody and labeled antigen are available, to which the test material (urine or saliva) is added. A positive or negative test result is obtained within a few minutes of initiating the reaction. To meet the increasing demand for drugs of abuse testing, numerous kits for on-site testing have appeared on the market and these are intended to be used away from the laboratory and without the need for any special training or technical skills on the part of the test operator. Extensive marketing of these on-site drug testing kits has occurred, although their reliability in terms of percent false-positive and false-negative responses differs widely. Some of these drug test kits have been criticized because the performance evaluations were done by trained personnel working in a laboratory environment.
A definite drawback with on-site drugs of abuse testing kits is the need to make a subjective evaluation of the results. Usually this involves identifying and interpreting some kind of color change, which is often not well defined. Recently, however, efforts have been made to develop on-the-spot tests for drugs in saliva. Because the concentrations in saliva seem to correlate well with concentrations in blood, the saliva test might be used at the roadside for screening impaired drivers.
Cross-reactivity of immunoassays
The crossreactivity of immunoassays towards other drugs, metabolites or endogenous substances is an important consideration. The antibodies used in the reaction exhibit different affinities for different drugs or analogs because the antibodies are always calibrated for a certain drug or metabolite over a specified range of concentrations. Reagents for benzodiaze-pines might show good sensitivity for nordiazepam and oxazepam, whereas the response to flunitrazepam might be unacceptably low, which can lead to a false-negative result for this sedative drug. The degrees of crossreactivity for each specific assay are usually provided by the manufacturer and these should be carefully scrutinized to understand better the capabilities of the reagent and which drugs or metabolites might interfere with the test.
Table 3 Guidelines for reporting urinary drug concentrations in connection with workplace drug testing
| Screening | EU | SAMHSA | Confirmation | EU | SAMHSA |
| drug group | (ngmr1) | (ngmr1) | drug/metabolite | (ngmr1) | (ngmr1) |
| Amphetamines | 300 | 1000 | Amphetamine | 200 | 500 |
| Methamphetamine | 200 | 500a | |||
| Cannabinoids | 50 | 50 | Carboxy-THC | 15 | 15 |
| Cocaine metabolites | 300 | 300 | Bensoylecgonine | 150 | 150 |
| Opiates | 300 | 2000b | Morphine | 200 | 2000b |
| Codeine | — | 2000b | |||
| 6-Acetylmorphine | — | 10b | |||
| Phencyclidine | — | 25 | Phencyclidine | — | 25 |
Methods of Confirmatory Analysis
All specimens identified as positive by an immunoassay screening procedure must be reanalyzed using a more sensitive and selective method. This normally involves use of gas chromatography (GC) or high-performance liquid chromatography (HPLC) in combination with mass spectrometry (MS). Indeed, mass spectrometric methods, preferably with deuterium-labeled internal standards, are considered mandatory in many drugs of abuse testing laboratories. Accordingly, MS is a prerequisite for definitive testing to confirm the positive immunoassay results so that the concentration of abused drug or drugs can be reported with certainty. A summary of analytical techniques used for quantitation is given in Table 4.
Confirmatory analysis necessitates taking a fresh aliquot of the blood or urine and extracting the drug from the biological matrix by means of various cleanup procedures. Because many drugs and metabolites excreted in urine are conjugated with glucuronic acid or sulfate, the drug conjugates are often hydrolyzed to liberate the drug and thereby increase its concentration before proceeding with the quantitative analysis. The hydrolysis of glucuronide conjugates is either done by carefully heating the urine with hydrochloric acid or by the use of various enzymes (p-glucuroni-dase) at a controlled pH. Table 5 lists various drugs of abuse together with the main metabolites commonly encountered in urine samples sent for analysis to forensic toxicology laboratories.
Clean-up procedures
The methods used to extract drugs from a biological matrix are similar for both blood and urine specimens, although with blood samples one is usually looking for the parent drug as well as metabolites, whereas with urine only the metabolites might be present. No universal procedure exists to extract all drugs from the biological matrix because of the vast differences in physicochemical properties. Owing to the low concentration of an active drug or its metabolites, together with many possible interfering substances, there is a need to choose a particular clean-up procedure that will concentrate the analytes.
The traditional method of extracting a drug and/or its metabolites from a biological matrix (blood, plasma or urine) involved the use of liquid-liquid extraction. This required adjusting the pH of the body fluid with a suitable buffer solution so that the substance of interest remained predominantly in unionized (lipid-soluble) form. An organic solvent such as chloroform was then added to the buffered body fluid or tissue homogenate and mixed vigorously, often by mechanical shaking for 30min or more in an attempt to bring the drug from the aqueous phase into the organic phase. Evaporation of the organic solvent to dryness concentrated the drug prior to making a derivative suitable for chromato-graphic analysis. Cleaner extracts could be obtained by making a back-extraction from solvent to aqueous phase and again over into the solvent, but this extra step usually gave a lower percentage recovery of the drug.
Table 4 Analytical techniques used for quantitative analysis of drugs of abuse
| Method | Sensitivity | Specificity | Expertise/cost | Applications for drugs of abuse testing in forensic toxicology |
| HPLC-UV | * | * | ** | Polar drugs/metabolites, such as benzodiazepines |
| HPLC-fluorescence | *** | ** | *** | Polar drugs/metabolites at low concentrations, such as LSD |
| HPLC-EC | *** | ** | *** | Polar drugs/metabolites at low concentrations, such as cannabinoids |
| HPLC-MS | *** | **** | ***** | Polar drugs that are present at very low concentrations, such as LSD, psilocin |
| GC-FID | ** | Drugs with oxidizable carbons, present in ^gml-1 concentrations | ||
| GC-EC | *** | ** | *** | Halogenated and nitroaromatic drugs, such as benzodiazepines and other drugs that can be derivatized with halogenated reagents |
| GC-NPD | *** | ** | *** | Drugs at low concentrations containing a nitrogen or phosphorus atom. |
| GC-MS | *** | **** | **** | Drugs present at low concentrations |
| GC-MS-MS | **** | ***** | ***** | Drugs at very low concentrations, structural identification of unknowns |
Table 5 Principal drugs of abuse encountered in forensic toxicology and their main urinary metabolites
| Parent drug | Main metabolites |
| Heroin | 6-Acetylmorphine, morphinea |
| Morphine | Morphinea, normorphine |
| Codeine | Codeinea, morphinea, norcodeine |
| Fentanyl | Norfentanyl |
| THCb | Carboxy-THCa, 11-hydroxy-THC |
| Amphetamine | Phenylacetone, 4-hydroxyamphetamine, norephedrine |
| Methamphetamine | Amphetamine |
| MDMA (ecstasy) | 4-Hydroxy-3-methoxy methamphetaminea (HMMA), MDA |
| MDE | 4-Hydroxy-3-methoxy ethylamphetaminea (HME), MDA, |
| MDA | 4-Hydroxy-3-methoxy amphetaminea (HMA) |
| Phenmetrazine | 4-Hydroxy phenmetrazinea |
| Cocaine | Benzoylecgonine, ecogonine methylester, norcocaine, cocaethylenec |
| LSD | Nor-LSD |
| Diazepam | Nordiazepama, oxazepama, temazepama |
| Oxazepam | Oxazepama |
| Flunitrazepam | 7-Aminoflunitrazepam, 7-acetamidoflunitrazepam |
| Phenobarbital | Hydroxylated metabolites |
| Phencyclidine | No major urinary metabolites |
In recent years, because of time constraints and possible health hazards associated with handling large volumes of organic solvent (e.g. chloroform or ether), other methods of extracting drugs from biological samples have been developed: in particular, solid-phase extraction (SPE). SPE columns or cartridges are commercially available and have become widely used in laboratories specializing in drugs of abuse testing. These disposable SPE cartridges are easy to use and permit the rapid extraction of acidic, basic or neutral drugs from a biological matrix with good recoveries. The columns or cartridges used for SPE are packed with an inert sorbent material such as silica or polymer resins, with attached functional groups, that preferentially bind to the drugs of interest, allowing the impurities to pass through the column. The drug is
finally eluted from the column after washing with suitable solvents or buffers. The choice of solvents and the kind of SPE columns depend on the target drug to be analyzed in the biological specimen. Examples of extraction and detection protocols for amphetamine, carboxy-THC, unconjugated opiates and cocaine metabolites are shown in Table 6.
Choice of an internal standard
The quantitative analysis of drugs of abuse in body fluids almost always involves the use of an internal standard. Accordingly, the first step in an assay requires adding to the biological specimen a known amount of an analog of the drug of interest before starting the clean-up and quantitative analysis. When GC-MS or HPLC-MS are the methods used, the internal standard of choice is generally a deuterium-labeled analog with a molecular weight usually 3-11 mass units higher than the illicit drug. The chemical properties of the deuterium-labeled analog are practically identical to those of the analyte, and similar mass fragmentation patterns are obtained. The deuterium compounds are slightly more lipophilic than the nonlabeled substances and this might give slightly shorter chromatographic retention times. Adding an internal standard also helps to compensate for incomplete extraction recovery during the clean-up procedures, and at the same time minimizes losses of analyte that occur during transport through the GC column and in the injector port.
Table 6 Confirmatory (verification) methods suitable for analysis of principal drugs of abuse in urine
| Assay | Amphetamines | Carboxy-THC | Unconjugated opiates | Cocaine and |
| conditions | metabolites | |||
| Sample | 0.2 ml urine | 1.0 ml urine | 1.0 ml urine | 1.0 ml urine |
| volume | ||||
| Internal | Pentadeuterated analogs | Trideuterated carboxy- | Trideuterated analogs | Trideuterated analogs |
| standard | THC | |||
| Pretreatment | None | Hydrolysis KOH 120C° for 10 min | None | None |
| pH setting | KOH pH13 | Acetic acid pH 4 | Phosphate buffer pH 6.1 | Phosphate buffer pH 6.1 |
| Extraction | Isooctane | Bond Elute THC SPE | Bond Elute Certify SPE | Bond Elute Certify SPE |
| Derivatization | TFAA | PFPA/PFPOH (4:1) | Acetonitrile: BSTFA 1% TMCS (3:1) |
PFPA/PFPOH (4:1) |
| GC column | 30m* 0.25mm HP5MS | 30m* 0.25 mm HP5MS | 30m* 0.25mm HP5MS | 30m* 0.25 mm HP5MS |
| SIM ions | Amphetamine | Carboxy-THC | 6-acetylmorphine | Cocaine |
| 140, 118, 91 | 622, 607, 459, 445 | 399, 340, 287 | 303, 272, 182 | |
| Methamphetamine | Morphine 429, 414, | Bensoylecgonine | ||
| 154, 118, 91 | 401 | 361, 346, 240 | ||
| Phenmetrazine | Ethylmorphine 385, | |||
| 273, 167 | 357, 234 | |||
| MDA 275, 140, 162 | Codeine 371, 343, | |||
| MDMA 289, 154, 162 | 234 | |||
| MDE 303, 168, 162 | ||||
| LOQ | 200 ngmr1 | 5ngmr1 | 20ngmr1 | 50 ngmr1 |
Derivatization
Derivatization of an analyte entails converting the molecule into a structure more suitable for chroma-tography and/or detection. It also assists in: (1) enhancing the analyte’s thermal stability and volatility; (2) improving the analyte’s chromatographic characteristics; (3) increasing the sensitivity of the assay; and (4) ensuring optimal mass spectrometric characteristics of the analyte.
Many drugs and their metabolites contain functional groups with active hydrogen atoms, for example amino groups, alcohol groups and carboxylic acid groups. Active hydrogens tend to enhance polarity and facilitate hydrogen bonding, which negatively influences volatility, thermal stability and reactivity. After derivatization, the drug passes more easily through the GC injector without being thermally degraded and without binding to the chromatographic column material.
Although derivatization is an easy task to perform, care is necessary to optimize the conditions. The extract should not be heated to high temperatures for prolonged periods because this can produce interfering substances and lower recovery of the analyte. The obvious way to choose a derivative is to inspect the molecular structure and functional groups present in the drug, and then consider which analytical techniques are suitable. This will often determine the strategy for preparing a suitable derivative. Derivati-zation requires additional steps in the pretreatment of the sample and therefore should be easy to perform, with the potential for automation.
Table 7 gives examples of the principal derivatizing agents applied to the analysis of some common drugs of abuse. For GC and GC-MS the usual procedures are silylation, alkylation and acylation reactions. Silyl derivatives tend to be easily hydrolyzed and the extracts should therefore be protected from moisture during the reaction. This can be achieved by dissolving the sample in a solvent containing a small amount of the derivatizing agent, or even by injecting the reaction mixture directly into the GC column. Alkylation includes replacement of an active hydrogen with an aromatic or aliphatic group, e.g. a methyl group to produce a volatile derivative with good stability. Acylation involves the conversion of alcohols and amines into esters and amides, respectively. The most common acylating reagents are anhydrides containing halogens, preferably fluorine, such as pen-tafluoropropionylanhydride (PFPA). Perfluoroacyla-tion improves the sensitivity ofGC analysis, especially when an electron capture detector is used for analysis, and at the same time the sensitivity and selectivity of mass spectrometric detection is also improved.
Table 7 Derivatization reagents and applications for confirmatory analysis of drugs of abuse
| Functional group | Drugs of abuse | Reagents | Derivatization procedure | Comment |
| Primary amine-NH2 | Amphetamine | TFAA, PFPA, | Perfluoroacylation | Amines form stable amides |
| MDA | HFBA | with the acetylating reagents and are preferred to silylation | ||
| Secondary amine -NH-R | Methamphetamine MDMA, MDE, MBDB |
TFAA, PFPA, HFBA | Perfluoroacylation | |
| Carboxyl -COOH | Benzoylecgonine | PFPA/PFPOH | Perfluoroacylation | Carboxylic acids form esters |
| BSTFA, MSTFA | Trimethylsilylation | in a two step reaction with PFPA/PFPOH |
||
| Carboxyl -COOH and | Carboxy-THC | Methyl-8, TMSH | Alkylation | Methylation usually produces |
| hydroxyl -OH | PFAA/PFPOH | Perfluoroacylation | more stable derivatives and less fragmentation compared to perfluoroacyl derivatives | |
| Hydroxyl -OH | Morphine, codeine | TFAA, PFPA, | Perfluoroacylation | Acylated hydroxyls have less |
| HFBA, BSTFA, | Trimethylsilylation | thermal stability than | ||
| MSTFA | silylethers and a peakfronting can be seen as a result of decomposition on the column |
Gas chromatographic analysis
Gas chromatography is the mainstay of analytical toxicology laboratories because this technique allows separation of the components of a mixture and quantitative analysis in a single step. Separation of the components is based on physical or chemical properties of the drugs, such as their partition coefficients, solubility, polarity and volatility. A carrier gas, which is usually helium or nitrogen, serves to transport the analytes from the injection port through a chromato-graphic column and into the detector. During this process, the components of a mixture equilibrate between the moving and stationary phases and, depending on the rate of movement through the column, a separation is accomplished. After separation the various components and the amounts present are measured both qualitatively and quantitatively by one of a number of detector systems.
Flame ionization detector (FID) The FID is a universal detector that responds to almost any compound containing carbon and hydrogen atoms. The intensity of response depends on the number of oxidizable carbon atoms in the molecule. After passing through the column mixed with the carrier gas, the analytes are burnt in a hydrogen-air flame. The current produced from the ionized compounds is measured by an electrode situated above the flame. The current is amplified and the response fed to an electronic integrator and recording system. The FID has excellent linearity over several orders of magnitude but the sensitivity is limited to the microgram per milliliter range.
Nitrogen-phosphorus detector (NPD) This detector uses the same principle as the FID but by introducing alkali metal vapors through an electrically heated rubidium bead, in combination with a lower flame temperature, this dramatically increases the response to compounds containing nitrogen and phosphorus atoms. By slight changes in the operating conditions one can achieve phosphorus:carbon response ratios of 50 000:1 or nitrogen:carbon response ratios of 5000:1. The detector is widely used in the toxicolo-gical laboratory because many drugs contain nitrogen atoms, but the NPD is also very useful for the analysis of, for example, phosphorylated pesticides.
Electron capture detector (ECD) The ECD contains a radioactive isotope, e.g. 63Ni, that bombards the carrier gas with electrons. Electrons are absorbed by compounds with high electron affinity, such as halo-genated compounds or those with nitro- or carbonyl groups. The response is measured as the drop in current, not as an increase as with the other detectors. Benzodiazepines are readily detected by ECD because they often contain both halogens and nitroaromatic structures. The ECD has been used to analyze many drugs, especially if halogenated derivatives can be prepared.
Mass selective detector (MSD) The MSD is the most universal and still the most selective detector, and mass spectrometric methods are widely used for analysis of drugs of abuse, especially when the structural identity of the compound has prime importance. With the MSD the target compounds are excited by either electron bombardment or by the collision energy from a reagent gas (e.g. ammonia or methane) in an ion source. The excited molecules fragment in ways predicted by their functional groups and chemical structure. This gives a ‘fingerprint’ of ions that shows the characteristics of the molecule and permits an almost unambiguous identification. With GC-MS methods, both retention time and mass fragments are used to identify the unknown substance by comparison with results from known standards. These standards contain the target drug at appropriate concentrations and are extracted and derivatized in the same way as the authentic sample.
Analysis of Specific Drugs Amphetamines
Amphetamines are central nervous stimulants with a chemical structure related to biogenic amines derived from phenylisopropylamine. Different side chains are possible and various groups might be joined to the aromatic ring, e.g. ecstasy (MDMA). Within this class of drugs amphetamine, methamphetamine, MDA,MDMA and MDE are widely abused. Amines are readily extracted from aqueous solutions, such as urine, at an alkaline pH. The extraction of amphetamines with organic solvent (e.g. isooctane, ethyl acetate or butyl chloride) followed by derivatization with a perfluoroacyl reagent (e.g. TFAA, PFPA or HFBA) are commonly used (Tables 6 and 7). The derivatives can then be analyzed by GC-MS in full scan or selected ion monitoring (SIM) mode, with at least three prominent fragments being used for identification and quantitative analysis. Derivatization of the analyte is necessary before embarking on GC-MS analysis of amphetamines because of their low molecular weights and the fact that they undergo alpha-cleavage thus producing base peaks with mass-to-charge ratio (m/z) 44, 58 or 72, depending on the particular N-substitution. This low mass range means that background signals and ‘noise’ are troublesome and numerous endogenous compounds might interfere with the analysis. Increasing the molecular weight by derivatization before analysis yields m/z fragmentation patterns with less background noise, and a more sensitive and specific identification is possible. Many laboratories have developed confirmation methods dedicated to rapid and reliable analysis of amphetamine and methamphetamine because they represent the most commonly abused drugs in many countries. Also the enantiomers of amphetamine and methamphetamine can be separated by GC-MS with the aid of chiral chromatographic columns, or chiral derivatizing reagents. Accordingly it is possible to distinguish the d- and /-forms of these amines, which might be necessary to rule out legal use of some over-the-counter drugs such as Vick’s inhaler which contains the /-isomer of methamphetamine.
Fig. 2 shows a chromatogram obtained from the analysis of a control sample containing amphetamine and related compounds as their perfluoracylated derivatives. The use of this broader analysis is popular in many forensic toxicology laboratories when the preliminary immunoassay screening analysis yields positive results for amphetamines. The confirmation analysis determines exactly which drug or drugs are present that might account for the positive screening test result. Because of the increasing number of phenylethylamines currently being abused, there is a continuous need for development in forensic urine drug testing methods.
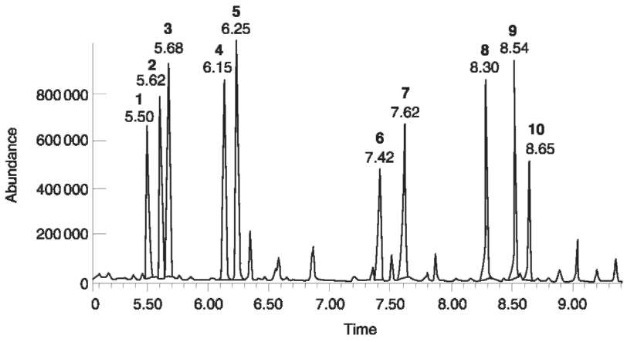
Figure 2 Total ion chromatogram (TIC) from the analysis of a standard sample containing amphetamine and related drugs. 1, Amphetamine; 2, phentermine; 3, norephedrine; 4, ephedrine; 5, methamphetamine; 6, phenmetrazine; 7, methylenedioxy-amphetamine; 8, methylenedioxymethamphetamine; 9, methylenedioxyethylamphetamine; 10, methylenedioxyphenyl-2-butana-mine.
Marijuana
The main pharmacologically active substance in preparations from Cannabis sativa is tetrahydrocannabinol (THC). There are many metabolites of THC, but most analytical methods have been developed to determine carboxy-THC, the main urinary metabolite. Carboxy-THC is excreted as the glucuronide in urine and, before extraction, a hydrolysis is performed, usually by heating with sodium hydroxide to cleave the glucuronide. Extraction of carboxy-
THC can be done either with solvent-solvent extraction at acidic pH or using SPE. Because carboxy-THC is an acid, liquid chromatography became a popular method for separation followed by electrochemical detection for quantitative analysis and HPLC methods gave enough sensitivity to detect drug concentrations in the nanogram per milliliter range. More recent demands for mass spectral identification of drugs of abuse in body fluids made it necessary to change from HPLC to GC-MS for the confirmation of carboxy-THC. The successful GC separation of car-boxy-THC requires derivatization of the functional groups and several approaches have been used. Two of the most common derivatization methods are methylation or perfluoroacylation of the alcohol and carboxylic acid groups. Methylation gives rise to few ions with high intensity, whereas perfluoroa-cylation gives more ions, but these are in the high mass range where the background noise is low, as shown in Fig. 3. Thus, both derivatizing procedures result in very sensitive analytical methods for determination of carboxy-THC in body fluids.
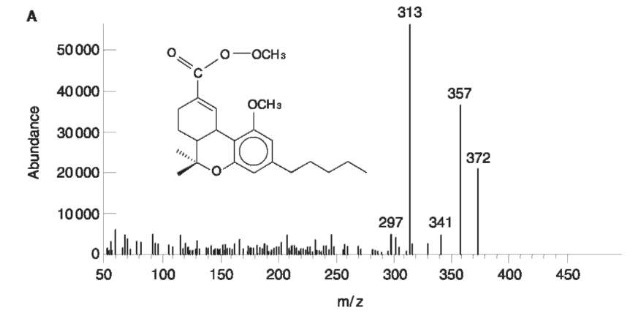
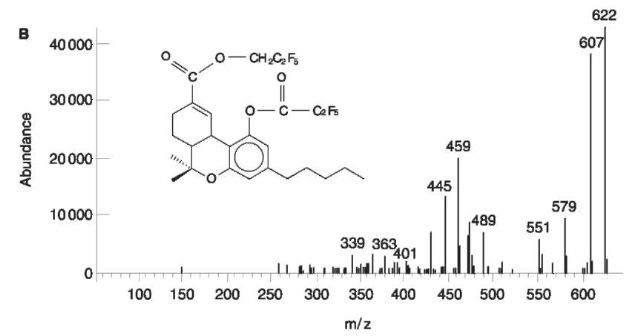
Figure 3 Mass spectrum of (A) methylated carboxy-THC using trimethylsulfonium hydroxide (TMSH) as derivatizing agent; and (B) perfluoroacylated carboxy-THC using pentafluoropropionic acid anhydride/pentafluoropropanol (PFPA/PFPOH) as derivatizing agents.
Opiates
Analysis of morphine and codeine in urine is readily done with GC-MS methods but special considerations are needed to distinguish which drug has been taken because morphine is a metabolite of codeine (Table 5). Both morphine and codeine are mainly excreted in urine as their glucuronides, and hydrolysis is usually performed before extraction and analysis. Enzymatic (p-glucuronidase) or acid (HCl) hydrolysis can be used to cleave the glucuronide, and recoveries appear to be more effective and reproducible after acid hydrolysis. Because the ratios of total morphine and total codeine are used to distinguish between heroin or codeine intake, the efficiency and reproducibility of the hydrolysis reaction is crucial for correct interpretation.
In addition to evaluating morphine:codeine ratios, one can determine 6-acetylmorphine, which is considered a specific metabolite of heroin, together with the unconjugated morphine and codeine. At a 10ngml-1 cutoff level for 6-acetylmorphine it may be possible to prove use of heroin if this occurred within about 24 h before sampling the urine.
Despite some difficulties with the chromatography and quantitative analysis, morphine, codeine and 6-acetylmorphine are usually derivatized with tri-methylsilylating agents such as BSTFA or MSTFA. Chromatographic separation of morphine, codeine, norcodeine and other opiates, such as hydromorphone and hydrocodone, has proven difficult in routine casework, and the identification by means of qualifier ions is complicated because some ions are the same for different analytes. Fig. 4 shows a chromatogram and mass spectra of morphine, codeine, hydromorphone and hydrocodone as their TMS derivatives.
Quantitation can be complicated because silicon (28Si) is a so called A+2 element, containing a naturally occurring isotope with a molecular weight 2 mass units higher (30Si). This isotope can interfere in the quantitation if the analyte is present at high concentrations, and if a trideuterated internal standard is used. This problem becomes more acute during the analysis of morphine, which has two TMS molecules attached, and thus two silicon atoms can contribute to the m/z of the internal standard. A better analytical strategy is perfluoroacylation, which gives derivatives without silicon and also produces m/z values in a higher mass range than TMS derivatives. However, the perfluoroacylated derivatives of opiates are thermally unstable and can degrade on the column. Recent developments and lower costs of LC MS instrumentation will prove attractive to forensic tox-icologists because the various glucuronides can also be quantitated along with the parent drugs, offering better grounds for judging impairment and evaluating deaths from heroin/opiate overdose.
Cocaine
Cocaine has a short elimination half-life and is rapidly biotransformed after administration. The main metabolites are benzoylecgonine (BE) and ecgonine methyl ester (EME). Other metabolites such as norcocaine and cocaethylene have been analyzed in both blood and urine, but most laboratories use methods that detect cocaine, BE and EME. Cocaine can easily be degraded to BE in vitro so precautions are necessary to avoid this happening, particularly when the analytical results are used to estimate the time since administration. BE is a zwitterion, which complicates its extraction from the biological matrix by the possible charge distribution at either the nitrogen atom or the car-boxylic acid. However, solid-phase extractions using mixtures of a cation exchanger and a hydrophobic carbon chain have been used with good results. BE contains a free carboxylic acid group which must be derivatized before analysis, whereas cocaine remains unaffected by the derivatization reagent. Both silylat-ing and perfluoroacylating reagents can be used for analysis of cocaine and its metabolites with good results. Moreover, opiates can be extracted under the same conditions as cocaine and BE, which allows identification of heroin and cocaine and their metabolites in the same analytical run.
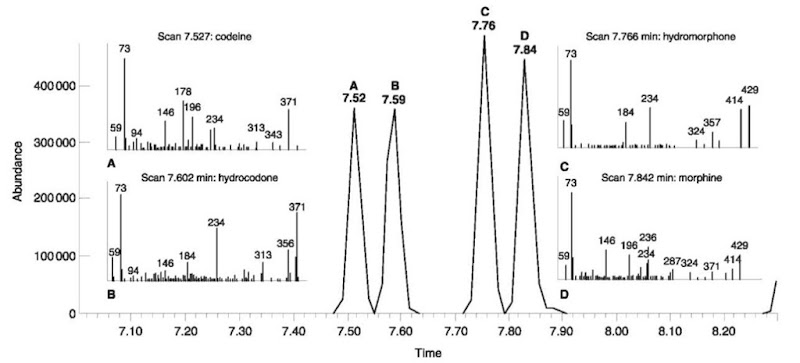
Figure 4 Total ion chromatogram (TIC) and mass spectra from (A) codeine-TMS; (B) hydrocodone-TMS; (C) hydromorphone-2TMS, and (D) morphine-2TMS. Almost baseline separation of the analytes are achieved using a HP-5MS 30m*0.25mm inner diameter column. Initial temp 150°C, ramped at 35°Cmin-1 to 260°C, then ramped at 5°Cmin-1 to 285°C. Incomplete silylation of hydrocodone and hydromorphone as their enols can further complicate the chromatogram.
Hallucinogens
The classical hallucinogens include mescaline, psilo-cybin and lysergic acid diethylamide (LSD). The two former drugs occur naturally in the peyote cactus and psilocybe mushrooms, respectively, whereas LSD was synthesized by Albert Hoffman in 1943 from ergot alkaloids. The effective doses of LSD and psilocybin are very low and the drugs are extensively metabolized, which creates problems for the forensic toxicol-ogist faced with analysis of these substances in body fluids. Moreover, the drugs are not very stable in body fluids after sampling, which creates difficulties for making reliable quantitative analyses. Psilocybin is rapidly transformed to psilocin, which is excreted in the urine predominantly as a conjugate. Published methods for analysis of psilocybin and psilocin are tedious, involving enzymatic hydrolysis, freeze drying or dialysis. Subnanogram quantitation of LSD in urine was reported by use of HPLC and fluorescent detection after solvent-solvent extraction with diethylether:n-heptane (1:1). Also GC-MS and GC-MS-MS procedures have successfully identified LSD and some of its metabolites at picogram concentrations. The introduction of LC-MS and LC-MS-MS will further increase the potential for qualitative and quantitative analysis of LSD and psilocin in body fluids.
Other abused drugs
A host of other drugs and chemical substances are candidates for abuse and are encountered by forensic toxicologists. In the USA phencyclidine (angel dust) is a leading drug of abuse, although this substance has not been especially prominent in European countries. More recently, y-hydroxybutyrate (GHB), which is easy to prepare, has received attention as a date-rape drug in some countries. The fast-acting sedative flu-nitrazepam is also used in date-rape crimes, especially in combination with alcohol. Prescription drugs (sedatives and hypnotics) of the benzodiazepine group are also candidates for abuse but legitimate medical indications make it difficult to legislate against their use. Nevertheless, analytical methods have been published for measuring the concentration of benzodiazepines in body fluids using immunoassay screening techniques and GC-MS with deuterium-labeled internal standards for confirmation.
Concluding Remarks
Developments and innovations in analytical chemistry and instrumentation are helping to keep pace with the escalation in abuse of drugs and other psychoactive substances in modern society. Forensic toxicolo-gists can demonstrate unequivocally that a person has indeed taken a particular drug, provided samples of blood and urine are obtained at appropriate times. Besides a multitude of drug-screening procedures (immunoassays), more sophisticated and time-consuming procedures are necessary for definitive testing. This requires careful extraction of the drug and its metabolites from the biological matrix and performance of a quantitative analysis, along with identification of the chemical structure of the abused substance. In analytical toxicology, mass spectro-metric analysis with a deuterium-labeled internal standard is without any doubt the method of choice.
