Each year, the words "you have diabetes" are spoken with greater frequency, often to unsuspecting individuals. Among Americans, the prevalence of diabetes has grown dramatically during the 20th century. Today, more than 16 million Americans have diabetes—90 percent of them are older than 40 years. Interestingly, half of these adults do not even know they have the disease because symptoms develop gradually and, at first, are hard to identify. Early diagnosis is important, though, because the longer diabetes goes untreated, the greater your risk for serious complications.
What Is Diabetes?
Diabetes mellitus is a disorder of metabolism—the way the body uses digested food for energy and growth. The origin of the name "diabetes mellitus" is Greek, referring to sweetness or honey (mellitus) that passes through (diabetes). After a meal, food is broken down into simpler forms and absorbed by the body. Simple sugars, amino acids, and fatty acids are used by the body or converted by the liver into sugar (glucose), the preferred fuel the body burns for energy. For cells to use this form of sugar, insulin—a hormone that is produced by the pancreas—must "unlock" the cells to allow glucose to enter.
The pancreas, a long, thin organ that is about the size of a hand, is located behind the stomach. Normally the pancreas produces the right amount of insulin to accommodate the amount of sugar that is in the blood. Diabetes is actually not a single condition but a group of diseases with one thing in common—a problem with insulin. In a person with diabetes, the pancreas does not produce sufficient insulin to meet the body’s needs. This insufficiency may develop if the pancreas stops producing the right amount and quality of insulin, if the rest of the body’s cells do not respond properly to insulin, or a combination of both. Insulin is required for glucose to be metabolized properly. If there is not enough insulin, excess glucose builds up in the blood, and the resulting condition is called hyperglycemia.
Persistent hyperglycemia causes almost all the symptoms that may alert an individual to the development of diabetes.
These symptoms can include frequent urination, extreme thirst, blurred vision, fatigue, unexplained weight loss, recurrent infection, tingling or loss of feeling in the hands or feet, and hunger.
With diabetes, the excess glucose spills into the urine, and the urine output increases. Consequently, the person with diabetes becomes dehydrated and thirsty. Fatigue results when the supply of glucose to cells is not available, causing energy levels to decline. To compensate for the lost fuel, the body burns stored fat, and weight loss and hunger may occur. Left untreated, persistent hyperglycemia is also responsible for most of the long-term complications of diabetes (see Long-Term Complications of Diabetes, this page).
There are several types of diabetes—different disorders with different causes. The two most common types are described here.
Type 1 Diabetes
Type 1 diabetes occurs in 1 in 10 people with diabetes. In these individuals, the pancreas produces little or no insulin. To control blood sugar, insulin must be taken. Most people whose diabetes is diagnosed before age 30 have the insulin-dependent type. It used to be called insulin-dependent diabetes mellitus or juvenile-onset diabetes. Type 1 diabetes affects both sexes equally. In most cases it is due to an autoimmune disease in which the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. This type of diabetes commonly develops in childhood, but it can occur at any age. It can develop unnoticed for several years and then suddenly become apparent, often after an illness. Some people—particularly children and teenagers—may first become aware of the disease when they develop ketoacidosis. This is a serious complication in which the blood becomes more acidic because of severe insulin deficiency.
Type 2 Diabetes
Type 2 diabetes accounts for about 85 to 90 percent of diabetes in people older than 30. It was previously called non-insulin-dependent or adult-onset diabetes. Most persons with type 2 diabetes are overweight or obese.
For people with this type of diabetes, total absence of insulin is not the problem. The problem is that the body does not make enough insulin to meet its needs and the insulin does not work normally to control glucose levels. This is termed "insulin resistance" and leads to hyperglycemia.
Excess weight is by far the greatest risk factor for development of type 2 diabetes. Most people who develop type 2 diabetes are overweight, a condition that appears to impair insulin action. Someone who is overweight and has diabetes may be able to achieve a normal blood sugar without medication simply by losing weight. Losing as little as 10 percent of body weight has been shown to lower blood glucose. Surprisingly, persons who are not overweight by traditional criteria also may be at risk for diabetes. Excess body fat distributed mostly in the abdomen increases the chance for development of type 2 diabetes. Other risk factors include age, race, heredity, and lack of physical activity.
Type 2 diabetes may go undetected for many years, because hyperglycemia develops slowly and the disease may not immediately produce the classic symptoms of diabetes. Unfortunately, even without symptoms, there are hidden dangers, including damage to major organs such as the heart and kidneys. Because the disease usually develops after age 40, and the incidence increases more steeply after age 55, it is important that people in middle age be screened for the disease and see their physician if symptoms develop.
Type 2 diabetes is more common among Native Americans, Hispanics, African-Americans, and westernized Asians than among people of European ancestry.
Long-Term Complications of Diabetes
Numerous studies have shown that keeping the blood glucose level close to normal delays the onset and prevents the progression of eye, kidney, and nerve diseases caused by diabetes. Even if blood glucose has not been controlled in the past, any improvement in diabetes control may help to avoid or delay complications of diabetes and their progression. Treatment of high blood lipid values and high blood pressure, which are commonly associated with diabetes, is also important.
Eye disease—In the absence of good glucose control, eye disease develops in nearly everyone with diabetes. Diabetic retinopathy occurs because high blood sugar (especially coupled with high blood pressure) can damage the small blood vessels in the retina (the light-sensitive area within the eye). Diabetes also can lead to cataracts, damage the macula (the area in the eye where the optic nerve is located), and increase the risk of glaucoma.
In addition to keeping your glucose levels under control, it is important to have regular eye examinations with an ophthalmologist, who dilates the eyes and does a thorough examination of them. A non-dilated eye test is not adequate for screening.
Blood sugar can be kept within normal levels by balancing the main treatment tools for diabetes—nutrition, weight control, exercise, and medication. In some people, blood sugar may be controlled by a combination of loss of excess weight, good nutrition, and regular exercise. Others may need medication.
Kidney failure—In the absence of good glucose control, a person with diabetes is 20 times more likely to develop kidney failure than someone who does not have the disease. Kidney disease results when chronic high blood sugar damages the small vessels in the kidneys which are responsible for filtering waste from the blood. Ultimately, kidney failure may occur, requiring dialysis or a kidney transplant. People with diabetes should have the function of their kidneys evaluated routinely.
Nerve damage—Also called neuropathy, nerve damage occurs in 30 to 40 percent of people with diabetes. Nerve damage can cause numbness and tingling, pain, insensitivity to pain and temperature, and extreme sensitivity to touch. Experts think the damage results from the effect of chronic high blood sugar on blood vessels that supply nerve cells. The feet are especially vulnerable to neuropathy.
Cardiovascular disease—Chronic high blood sugar is associated with narrowing of the arteries (atherosclerosis), high blood pressure, heart attack, and stroke. It is also associated with increased blood levels of triglycerides (a type of blood fat) and decreased levels of HDL ("good") cholesterol. Unless appropriately treated, an individual with diabetes is 5 times more likely to have a stroke and 2 to 4 times more likely to have coronary artery disease. Also, smoking dramatically accelerates the development of these cardiovascular complications. Anyone with diabetes should stop smoking.
infections—High blood sugar impairs the function of immune cells and increases the risk of infections. The mouth, gums, lungs, skin, feet, bladder, and genital area are common sites of infection. Nerve damage in the legs and feet can make someone with diabetes less aware of injuries or infection, increasing the risk of amputation. With proper care of the feet, foot complications can be minimized or avoided.
Can Diabetes Be Prevented?
Although an area of active research, there is currently no proven means of preventing type 1 diabetes. However, these lifestyle changes minimize the risk of, and may actually prevent, type 2 diabetes:
Maintain a healthful weight—Most people who develop type 2 diabetes are overweight. Aggressive efforts aimed at achieving and maintaining a healthful weight may be beneficial, especially in combination with exercise.
Eat a balanced diet—A diet low in saturated fat and sugar and high in complex carbohydrates and dietary fiber also has been linked to a reduced risk of diabetes.
Exercise—People who exercise regularly have a significantly lower incidence of type 2 diabetes.
How Is Diabetes Diagnosed?
It is important that diabetes be diagnosed early, before too much damage is done. As a first step, the American Diabetes Association recommends that everyone should visit a physician and get a fasting blood glucose test at age 45. A sample of blood is drawn after fasting overnight, and its glucose level is measured. A normal fasting result is between 70 and 110 milligrams of glucose per deciliter of blood (mg/dL).
A retest every 3 years is advised. If an individual has any risk factors for diabetes or any symptoms, testing at more frequent intervals or at an earlier age is recommended. Diabetes is diagnosed when a fasting blood glucose value is more than 125 mg/dL or a glucose value is more than 200 mg/dL accompanied by symptoms of diabetes. The diagnosis should be confirmed by repeat testing on a different day.
Tools for Controlling Diabetes
Persons with diabetes can live a full life by following a few basic principles to control their disease. Diabetes can be managed with at-home blood glucose tests, healthy nutrition habits, weight control, routine exercise, and medications (if needed).
The most important step is to learn to control the blood sugar value, which means maintaining it as near to normal as possible or in the goal range determined by your physician. Vigilant control of blood sugar levels may dramatically reduce the risk of eye, kidney, and nerve damage. This also lowers the risk of heart attack, stroke, and limb amputation, in addition to promoting a more desirable level of blood lipids.
Blood sugar can be kept within normal levels by balancing the main treatment tools for diabetes— nutrition, weight control, exercise, and medication. In some people, blood sugar may be controlled by a combination of weight loss, good nutrition, and regular exercise. Others may need medication.
Blood Sugar Levels
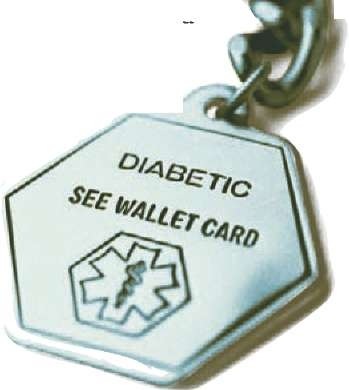
The level of glucose in the blood depends on several factors: when meals are eaten, how many calories are consumed, activity level, and the dose of medication prescribed. The stress of an illness may also alter the level of blood glucose. Successful daily management of diabetes may prevent or minimize emergencies that may result when blood sugar levels are too high or too low. Because these emergencies can cause mental confusion or loss of consciousness, people with diabetes should wear a medical alert identification and acquaint family members, friends, neighbors, and coworkers with the signs and symptoms of an emergency and steps to a proper response.
Blood sugar levels can be monitored with home testing meters. Testing not only measures the amount of sugar in the blood but also enables the person to identify the reasons behind high and low values so that adjustments can be made in the dose of diabetes medications. Frequently the person can learn how to adjust the dose of oral medication or insulin to achieve the desired glucose value. The health care team caring for the person with diabetes can determine reasonable blood sugar goals.
Nutrition
The old restrictive diets for diabetes no longer apply. It is now known that the best diet for diabetes control is consistent with what everyone should eat for good health. How much you eat is just as important as what you eat in controlling blood sugar. To keep blood sugar on an even keel, people with diabetes should not eat large meals or skip meals; they should eat smaller servings at regular intervals instead. As for the menu, choices should follow Food Guide Pyramid recommendations—emphasize whole grains, legumes, and vegetables. These foods are higher in complex carbohydrate and fiber and can help control blood sugar. Even though fruit contains sugar, it should not be avoided.
Because people with diabetes are at higher risk for cardiovascular disease, it’s important to keep the fat intake to about 30 percent of total daily calories and to limit cholesterol-containing foods. Items at the top of the Food Guide Pyramid—such as fats and sweets—should be eaten sparingly. Research has shown that the total amount of carbohydrate consumed at a given time, rather than the type of carbohydrate, is the most important factor in control of blood sugar. Therefore, if not present in excess, sugar can be included as a part of a well-balanced meal.
Many tools are available to help with meal planning. For most people, eating three meals at regular times and avoiding excessive sweets are enough to control blood sugar. Dietitians may provide a simple method, such as the Food Guide Pyramid, to encourage variety, proportion, and moderation in food selections and to also ensure healthful food choices.Other techniques may be needed and recommended by your physician, registered dietitian, or certified diabetes educator.
Weight Control
Because many people who have diabetes are overweight, maintaining a healthful weight and level of activity is the key to keeping the disease under control and minimizing the risk for serious complications. The more overweight people are, the more resistant their cells become to their own insulin; losing weight decreases that resistance. Often, weight loss of just 10 percent can improve blood sugar and have lasting beneficial effects.
Exercise
With exercise, some people with type 2 diabetes may even reduce or eliminate their need for insulin or oral diabetes medication. Anyone who has diabetes should check with a physician before starting an exercise program. Studies have shown that those at high risk for diabetes who exercise have a 50 percent lower incidence of type 2 diabetes. Exercise helps control weight, makes cells more sensitive to insulin, increases blood flow, and improves circulation in even the smallest blood vessels. A leaner body also helps burn calories more efficiently. Moreover, exercise lowers your risk of cardiovascular disease.
Exercise can affect blood sugar levels up to 24 hours. So if insulin is a part of the treatment plan, check with a physician to receive guidelines for frequency of blood sugar testing and insulin adjustment.
Medications
Along with nutrition, weight control, and exercise, medications may be necessary to achieve a desired glucose level. Persons with type 1 diabetes must take insulin by injection. Insulin cannot be taken by mouth because it breaks down in the digestive tract. The type of insulin and number of daily injections depend on individual needs. Insulin also can be administered by pump.
In some persons, type 2 diabetes can be managed by healthful nutrition and exercise alone. If the desired glucose level is not achieved, oral medications may be prescribed. There are several classes of oral medications. Some stimulate the pancreas to produce more insulin, and some help insulin to work more effectively in the body by decreasing the sugar made by the liver and by increasing the sugar removed from the blood to the cells. If oral medications do not achieve the glucose goal, insulin injections may be required.