MEDIAL PTERYGOID MUSCLE
The medial pterygoid muscle arises from the medial surface of the lateral pterygoid plate and from the palatine bone (see Figures 15-15 and 15-16). It inserts on the medial surface of the angle of the mandible and on the ramus up to the mandibular foramen. The principal functions of the medial pterygoid muscle are elevation and lateral positioning of the mandible. It is active during protrusion. The innervation is a branch of the mandibular division of the fifth nerve.
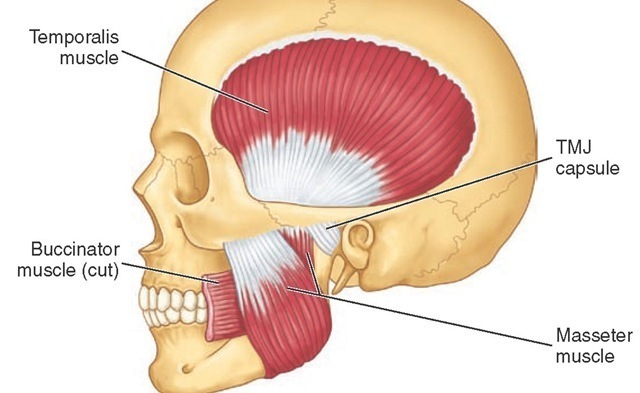
TEMPORALIS MUSCLE
The temporalis muscle is fan-shaped and originates in the temporal fossa (see Figures 15-16; 15-17, B; 15-18; and 15-20).
Figure 15-18 Masticatory muscles shown include the temporalis and masseter muscles. The deep masseter is attached to the zygoma (see Figure 15-17, C). TMJ, Temporomandibular joint.
On passing to the zygomatic arch, it forms a tendon that inserts into the anterior border and mesial surface of the coronoid process of the mandible and along the anterior border of the ascending ramus of the mandible (see Figure 15-16). The anterior fibers extend along the anterior border of the ramus almost to the third molar. The muscle has three component parts and appears to behave as if it consisted of three distinct parts. The temporal muscle is the principal positioner of the mandible during elevation. The posterior part is active in retruding the mandible, and the anterior part is active in clenching. The anterior part may act as a synergist with the masseter in clenching, whereas the posterior part acts as an antagonist to the masseter in retruding the jaw. The temporalis muscle is innervated by temporal branches of the mandibular division of the fifth nerve.
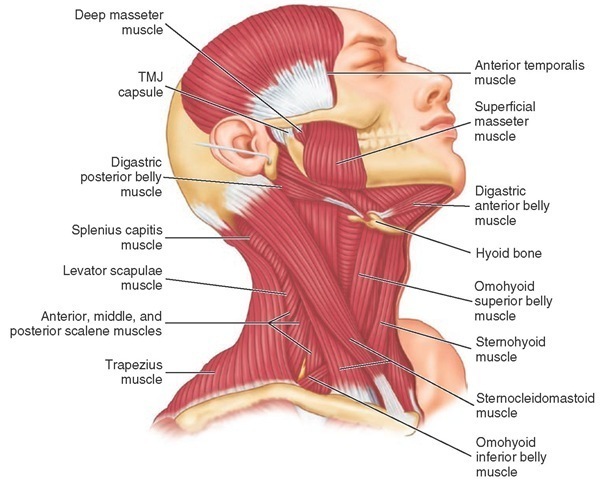
DIGASTRIC MUSCLE
The attachment of the anterior digastric muscle is at or near the lower border of the mandible and near the midline (see Figure 15-20). A tendon is between the anterior and posterior digastric muscles that is attached by a looplike strip of fascia to the hyoid bone. The anterior digastric muscle is covered by the platysma muscle, and beneath lie the mylohyoid and the geniohyoid muscles. All of these muscles are considered to be active during various phases of jaw opening. A mylohyoid branch of the mandibular division of the fifth nerve innervates the anterior digastric muscle (see Figure 14-37); the digastric branch of the facial nerve innervates the posterior digastric muscle.
GENIOHYOID MUSCLE
The geniohyoid muscle lies superior to the mylohyoid muscle and adjacent to the midline. It arises from the mental spine on the posterior aspect of the symphysis menti of the mandible. It inserts on the anterior surface of the hyoid bone. When the mandible is fixed, the hyoid bone is drawn forward and upward; when the hyoid bone is fixed, the lower jaw is depressed. Innervation is from C1, C2, and possibly the hypoglossal nerve (see Figure 14-37).
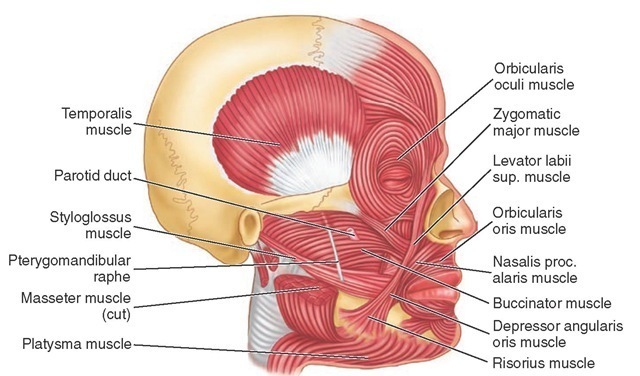
Figure 15-19 Muscles of facial expression and accessory muscles of mastication.
Figure 15-20 Muscles of the neck. TMJ, Temporomandibular joint.
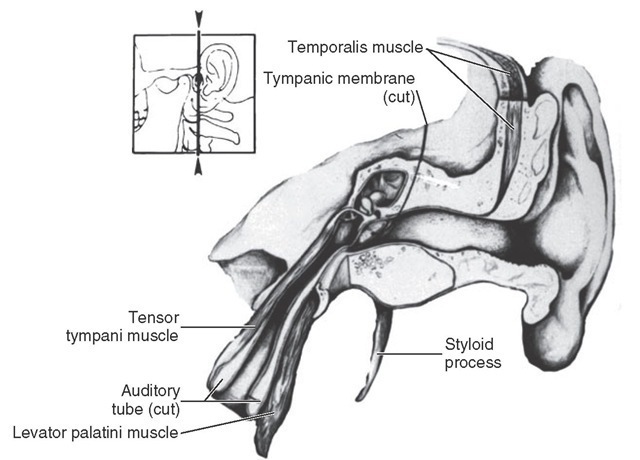
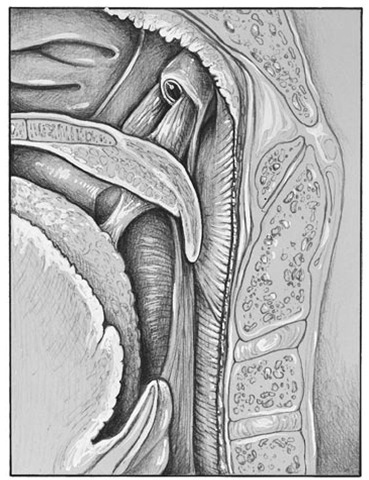
Figure 15-21 Section through the ear showing inner ear structures and the tensor tympani muscle, which is active in stretching the tympanic membrane.
TENSOR TYMPANI AND PALATINI MUSCLES
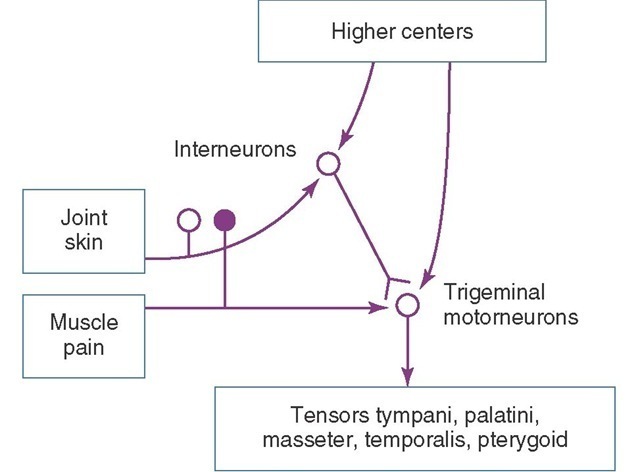
The tensor tympani, tensor veli palatini, and levator veli palatini muscles (Figures 15-21 and 15-22) may have clinical significance for subjective auditory symptoms associated with temporomandibular and muscle disorders (TMDs).1,8,9 These muscles are innervated by the trigeminal nerve and therefore may respond to similar kinds of ascending information from joints, skin, and muscles and from descending inputs from higher centers that converge on interneurons and the trigeminal motor nucleus (Figure 15-23). Disturbances of auditory tube opening during swallowing that may occur with TMJ and TMDs appear to be consistent with restricted function and anatomy of the tensor palatini and levator veli palatini muscles.10 If a causal connection between subjective hearing symptoms and TMDs is to be established, additional evidence-based research is needed.
Figure 15-22 Muscles of the throat. Eustachian tube and tensor palatinus muscle, which is active in opening the auditory tube.
Figure 15-23 Information from joints, skin, muscles, and higher centers converge on the interneurons and trigeminal motor nucleus.
Restricted jaw opening and prevention of yawning seen in TMJ and TMDs can lead to otological symptoms such as subjective hearing loss associated with sensations of stuffiness in the ear.1 Thus, pain in and around the joints and muscles may influence the otomandibular muscles via interneurons in the intertrigeminal area and might be responsible for a few cases of tinnitus associated with restricted jaw opening due to TMJ and muscle disorders.
HEAD AND NECK MUSCLES
The muscles of the head and neck have been of interest to the dentist because of a potential relationship among the occlusion, TMJs, and pain in these muscles and/or muscle contraction headache. The possible role of the epicranius muscles in tension headache has yet to be clarified. The sternocleidomastoid muscle (see Figure 15-20) is often affected in patients with TMJ muscle dysfunction and often co-contracts with jaw clenching. The functions of the orbicularis oris and buccinator muscles (see Figure 15-19) appear to have a significant role for optimal function of complete dentures. The seventh (VII) nerve innervates all the muscles of facial expression.
Other muscles that are of interest to the dentist because of TMJ and muscle disorders are the scalenus, splenius, ili-ocostalis cervicis, and omohyoideus. However, the association between TMDs and myalgia of the muscles has not been established. A number of problems in oral motor function, such as lip posture in the aged, may be related to a generalized deterioration in performance or to a specific motor function rather than the dental state or prescription medication. Most reports on motor disorders and aging have focused on disturbances in control originating in the nervous system.
Mandibular Movements and Muscle Activity
Mandibular movement during normal function and during parafunction (e.g., bruxism) involve complex neuromuscular patterns originating in part in a pattern generator in the brainstem and modified by influences from higher centers (see Figure 15-23), namely, the cerebral cortex and basal ganglia, and from peripheral influences (e.g., the periodon-tium, muscles, and so on). However, a detailed discussion of such movements is beyond the scope of this text. Rather, the discussion relates to muscle activity as seen in electro-myography for jaw opening and closing, protrusion, retru-sion, and lateral movements.
MANDIBULAR OPENING
The digastric, mylohyoid, and geniohyoid muscles are active during jaw opening, either slowly or maximally against resistance. No activity occurs in the temporalis and masseter muscles when the mouth is opened slowly and the jaw is opened maximally, although some activity may occur in the medial pterygoid muscle. When the jaw is opened against resistance, the temporalis muscle remains silent. During opening movements, the lateral pterygoid muscles show initial and sustained activity. In forced depression, the digastric muscle is activated almost as soon as the lateral pterygoid muscle is. Generally, the activity of the anterior digastric muscle follows that of the lateral pterygoid muscle.
MANDIBULAR CLOSING
While the mandible is being elevated slowly, without contact of the teeth, no activity is evident in any portion of the temporalis muscle. Elevation without contact or resistance is brought about by contraction of the masseter and medial pterygoid muscle. The temporalis, masseter, and medial pterygoid muscles affect elevation against resistance. The suprahyoid muscles act as an antagonist of the elevator muscles. Closure into maximal intercuspation (centric occlusion) may involve contraction of facial and neck muscles.
RETRUSION
Voluntary mandibular retrusion with the mouth closed is brought about by contraction of the posterior fibers of the temporalis muscle and by the suprahyoid and infrahyoid muscles. Retraction of the mandible from protrusion and without occlusal contact is effected by the contraction of the posterior and middle fibers of the temporalis muscles. Slight activity of the suprahyoid may be the result of slight jaw opening to allow the teeth to glide over each other from centric occlusion to centric relation.
PROTRUSION
Protrusion of the mandible without occlusal contact results from contraction of the lateral and medial pterygoid muscles and also masseter muscles. Protraction against resistance is brought about by contraction of the lateral and medial pterygoid muscles and of the masseter and suprahyoid muscle group. Protrusion with the teeth in occlusion is achieved by contraction of the pterygoid and masseter muscles. Only slight activity occurs in the suprahyoid muscles. In combined protraction and opening, activity is evident in the medial and lateral pterygoid muscles, the masseter muscles, and sometimes the anterior fibers of the temporalis muscles.
LATERAL MOVEMENTS
Lateral movement of the mandible to the right side (without occlusal contact) is achieved by ipsilateral contraction of primarily the posterior fibers of the temporalis muscle. The suprahyoid muscles are active in maintaining the jaw slightly depressed and protruded. Movement to the left side without occlusal contact is brought about by the contralateral contraction of the medial pterygoid and masseter muscles. Lateral movement to the right side against resistance is achieved by the ipsilateral contraction of the temporalis muscle and by some activity in the ipsilateral masseter and medial pterygoid muscles. Movement to the left side against resistance is achieved by the contralateral contraction of the medial pterygoid and masseter muscles. Lateral movement to the right with occlusal contact is achieved by ipsilateral contraction of the temporalis muscle. Movement to the left with occlusal contact is brought about by contralateral contraction of the medial pterygoid and masseter muscles. Both lateral pterygoid muscles initiate depression of the mandible, and the contralateral muscle initiates a lateral transversion. Lateral movements of the jaw are achieved by ipsilateral contraction of the posterior and middle fibers of the tem-poralis muscle and by contralateral contraction of the lateral and medial pterygoid muscles and the anterior fibers of the temporalis muscle. Parts of the temporal and masseter muscles may act as antagonists or synergists during horizontal movements and minimum separation of the teeth.
CHEWING
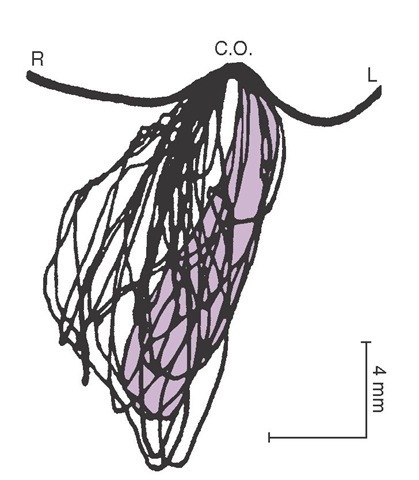
Chewing is highly complex oral motor behavior usually seen in the frontal plane in simple form (Figure 15-24). No archetypal chewing cycle exists. The means of the dimensions of the chewing cycle are between 16 and 20 mm for vertical movements and between 3 and 5 mm for lateral movements. The duration of the cycle varies from 0.6 to 1 second depending on the type of food. The speed of masticatory movement varies within each cycle, both according to the type of food and among individuals. Speed, duration, and form of the chewing cycle vary with the type of occlusion, kind of food, and presence of dysfunction.
Occlusal contacts occur in centric occlusion in at least 80% to 90% of all chewing cycles, especially near complete trituration of the bolus. With closing and opening movements, contact gliding is seen. In the closing phase, the contact glide depends on the type of occlusion and type of food. Where tough food is the normal diet (e.g., as with Australian aborigines) with corresponding occlusal wear, the chewing movement shows a long contact glide (2.8 ± 0.35 mm)12 compared with the short contact glide (0.90 ± 0.36 mm) of Europeans living on a modern diet of easily triturated food.13 The chewing force reaches a maximum in centric occlusion and lasts for 40 to 170 milliseconds, and the peak electromyographic activity of the temporal and masseter muscles lasts for a mean of 41 ± 26 milliseconds. Some chewing force is maintained for gliding tooth contact on the opening phase. In the intercuspal position, the jaw is stationary, or it pauses for approximately 100 milliseconds before the next cycle begins.
Figure 15-24 Mandibular movements during the process of chewing naturally. Incisor point movement is seen in the frontal plane.
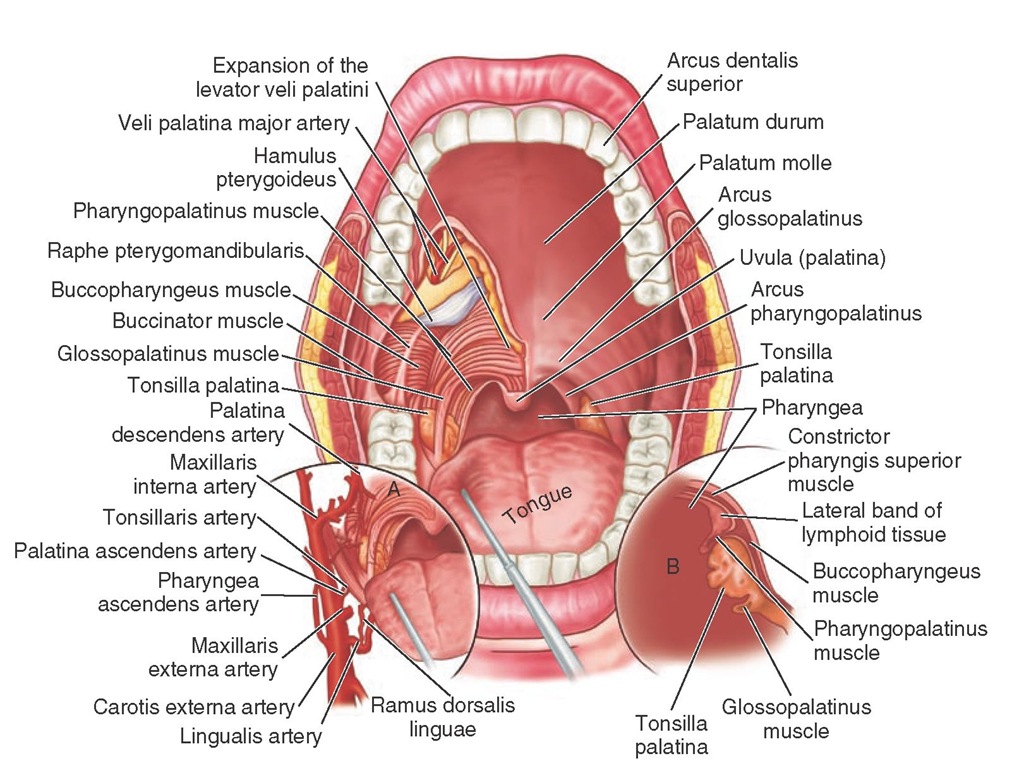
SWALLOWING
Swallowing involves most of the tongue muscles and buccal musculature.14 In the initial stage of swallowing, the bolus moves from the mouth to the fauces (Figure 15-25). The bolus is then moved from the fauces to the esophagus and finally through the esophagus to the stomach. When saliva is swallowed, total participation of the suprahyoid muscles occurs, with marked activity of the digastric and mylohyoid muscles, followed by moderate activity in the geniohyoid muscles. The medial pterygoid muscle is often active; less often, the temporalis and masseter muscles are active with occlusal contact.
ORAL MOTOR BEHAVIOR
Oral motor behavior refers to function and parafunction of the mouth and associated structures. More generally, behavior includes observable actions ranging from simple movements such as retrusion or protrusion to more complex movements such as chewing. To accomplish complex behavior, sensori-motor systems consisting of muscles and neural processes are required for the initiation, programming, and execution of motor functions.
Chewing movements depend on complex integrative neural processes of the central nervous system that may be initiated by either internal or external influences, including innate drives, emotional states, and instructions to patients.
During chewing, a large amount of proprioceptive (i.e., muscle sense) and exteroceptive (i.e., tactile sense) information is fed to the central nervous system (e.g., cerebral cortex, brainstem, basal ganglia, spinal cord). Rhythmic movements such as chewing are largely programmed or preprogrammed and involve learning, which reduces the need for peripheral sensory input. However, inputs from muscle, joint, tendon, and periodontal receptors still have important functions, especially in relation to learning, new experiences, and protective reflexes. Neuronal mechanisms must be present to provide for modification of reflexes and continued updating of masticatory movements by information about such factors as occlusal forces and the state and location of the bolus.
OVERVIEW OF MASTICATION
The act of mastication begins with "setting the system" by sight, tactile sense, and smell to receive the food. Involvement of the tactile sense may range from picking up the food to grasping the food with the incisor teeth. When the food is taken into the mouth, the lips, tongue, and periodontium function to estimate size, hardness, and other characteristics that must be correlated with previous behavior required for chewing. This information sets the chewing program in the pattern generator, including subsequences that relate to central and peripheral influences already in progress. Orofacial receptors such as periodontal mechanoreceptors may monitor occlusal forces and control the jaw-closing muscles.
Figure 15-25 Oral pharynx, with special reference to the palatine tonsil and the musculature of the palate.
The chewing program may be altered according to stages of chewing or in response to information from receptors in specific areas such as the palatal mucosa and tongue. The chewing rhythm may be stopped because of noxious stimuli. It is probable that rhythmic and repetitive chewing behavior is disturbed by dysfunctional states of the occlusion and/or the TMJs through which the bolus is shifted and the jaw moved to another position for the next forceful tooth-food contact. Thus chewing cycles may occur without the development of an actual power stroke in dysfunction states.