Adaptation
In an ideal occlusion, there should be no need for adaptation, but the criteria for it can be guidelines only, because their implementation may reflect clinical skill beyond the ordinary. Even minor occlusal discrepancies in a few individuals may result in acute orofacial pain and/or TMJ and muscle symptoms. It is not uncommon to have some kind of response (structural function and/or psychological) after the restoration of a maxillary central incisor if an occlusal interference to complete closure in centric occlusion has been placed by mistake in the restoration (Figure 16-54). If the interference cannot be avoided comfortably by mandibular displacement in chewing and swallowing by neu-romuscular mechanisms (functional adaptation), if the tooth becomes mobile and is moved out of position (structural adaptation), and/or if the patient cannot ignore the discomfort or the presence of change for even a short period (behavioral adaptation), overt symptoms of dysfunction of the muscles, joints, periodontium, or teeth (pulp) may occur. However, such adaptive response and failure of adaptation are observed only rarely, and such observations do not qualify as scientific evidence. Models of research to test the validity of these clinical observations have suffered from serious flaws in design. Still, no clinician would knowingly put an occlusal interference in a restoration.
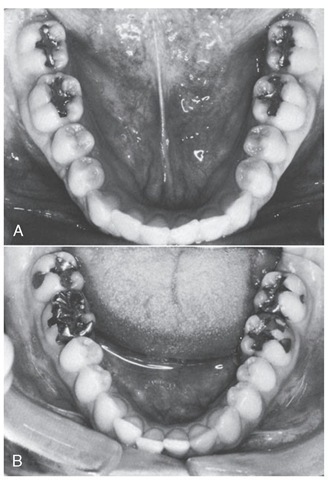
Figure 16-53 Anterior crowding. A, Absence of crowding. B, Crowding following restorative dentistry by only a few months. Clinical findings of very tight proximal contacts and an occlusal interference in centric relation are only presumptive evidence of a cause-and-effect relationship between restorative treatment and anterior crowding.
In addition to physical guidance from the teeth when the teeth are in contact during mastication or empty movements, mandibular guidance may occur before and during contact of the teeth from receptors in the periodontium and TMJs, and from other peripheral sensory receptors, as well as from higher centers in the central nervous system. It has been suggested that the anatomical relationships of the teeth and joints provide passive guidances and that active guidances involve reflexes originating in receptors in or around the teeth.52 The question of feedback from various structures influencing mandibular movements and position is a complex one and cannot at this time be clearly answered.
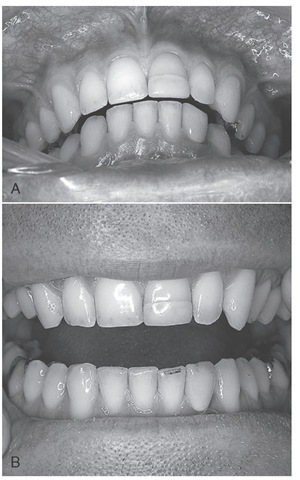
Figure 16-54 Occlusal interference to closure in intercuspal position/ centric occlusion due to restoration of the left maxillary central incisor. A, Centric relation position. B, Articulating paper mark on mandibular left lateral incisor. Temporomandibular disorder-like symptoms were relieved with adjustment of the centric occlusion interference.
The tendency to equate clinical responses with reflexes elicited under laboratory conditions rather than studying responses under natural conditions has led to what may be considered contradictory findings. It is also not unusual to find it assumed that failure to observe a response (i.e., a change in chewing patterns with anesthesia, occlusal interferences, and so on) is due to the absence of a response rather than to a failure in the method of observation. Thus some responses may exist under natural conditions but have not been observed. Whether a changed anatomical feature of the occlusion causes an alteration of mandibular movement depends on a number of factors involving preprogramming, learning, adaptation or habituation, relationship to function and parafunction, and other central or peripheral influences.
Occlusal Interferences
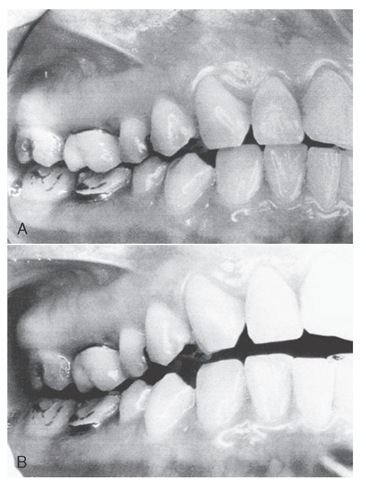
In terms of clinical strategy, an occlusal contact relationship must interfere with something (e.g., function or parafunction) to be considered an occlusal interference (Figure 16-55, A and B). Thus a contact on the nonworking side is not an occlusal interference unless such a contact interferes with ongoing function and parafunction (i.e., prevents contact at some point on the working side).
Figure 16-55 Occlusal interference to function. A, Intercuspal position. B, Right working position of the mandible with interference by first molar restorations. Note absence of canine contact.
In performing an indicated occlusal adjustment in centric relation, the clinician guides the jaw into a position of closure in a retruded contact position. In some individuals, premature occlusal contacts prevent a stable jaw relationship, and during guided rapid cyclical closure by the clinician, reflex jaw movements and muscle hyperactivity may occur to prevent such closure. Training of the patient and proper manipulation of the mandible in the absence of TMJ or muscle dysfunction may eliminate the muscle hyperactivity just long enough to guide the jaw into centric relation and to mark the occlusal interference with articulating paper (see Figure 16-43). During the course of an occlu-sal adjustment to remove occlusal interferences to a stable occlusion in centric relation, a number of responses occur. For example, in some patients during the elimination of interferences, removal of a premature contact results in complete elimination of muscle resistance to guided jaw closure; that is, the clinician may close the jaw rapidly or slowly without any muscle response to prevent the closure. This may occur even with a slide in centric remaining, provided the contacts are bilateral and multiple, and freedom to move smoothly from centric relation to centric occlusion is possible.
Another clinical observation during the occlusal adjustment is that before eliminating a particular interference and before guiding the jaw into contact to determine whether that interference has been eliminated, all resistance and reflex muscle activity to prevent closure into the retruded contact position is gone. It should be kept in mind that during the course of an occlusal adjustment, a new but transient solitary occlusal interference may occur, or an interference may have greater significance for one tooth than another. These observations agree with the results of several studies showing that occlusal relations can lead to avoidance responses that probably serve to protect the teeth, muscles, joints, and periodontium from trauma owing to occlusion. Training the patient to a hinge axis movement in the presence of occlusal interferences requires that no contact or anything even close to contact of the occlusion be made for several up-and-down movements and that the patient relax. Relaxation involves modulation of feedback from peripheral structures (joints, teeth, muscles, periodontium) and inhibitory effects from higher centers.
VERTICAL DIMENSION
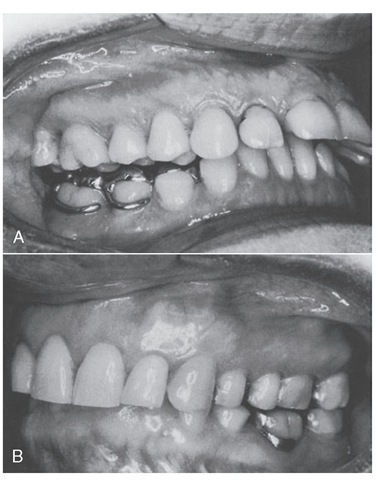
Contact vertical dimension (occlusal vertical dimension) is the vertical component of the intercuspal position/centric occlusion. Although it would be helpful to be able to relate the contact relationship of the teeth to the rest position of the mandible (or the interocclusal space), optimal working length of the jaw elevator muscles, swallowing, speaking, or some other neurobehavioral parameter of function, vertical dimension is usually described in terms of the height of the lower third of the face, mandibular overclosure, or a need to "raise the bite" (increase the height of the teeth with restorations) because of worn-down or intruded posterior teeth (Figure 16-56, A) or impinging overbite (Figure 16- 56, B). At the present time, no acceptable test of a presumed loss of vertical dimension appears available. The neuro-behavioral aspects of the interocclusal space and occlusal vertical dimension are complex and require much further study.
Figure 16-56 Vertical dimension. A, Use of a posterior bilateral onlay splint in an attempt to "raise the bite" and eliminate temporomandibular disorder symptoms. B, An impinging overbite may require comprehensive orthodontics for correction, not an appliance as in A.
It is not possible to determine with scientific assurance that aggressive bruxing and clenching in centric have caused intrusion or wear of the teeth or has been compensated for by eruption of the posterior teeth. Even short-term intrusion or loss of stops on posterior teeth may result in reflex-produced responses from anterior teeth because of premature contacts on anterior teeth. Again, no acceptable tests are available to determine with scientific assurance, even in the presence of dysfunction (e.g., temporomandibular disorder), that correction of a presumed loss of contact vertical dimension will correct the dysfunction.
Oral Motor Behavior
The term oral motor behavior is a convenience of speech by which it is possible to refer with a brief phrase to observable actions involving orofacial structures, including "simple" actions like assumption of mandibular rest position and much more complex movements such as mastication. Human behavior reflects the translation of past, present, and ongoing ideas and learning (including sensations and emotions) into movements and actions. Although many of the responses or actions are common among all persons, the subjective response of a particular individual to a stimulus (including a change in the occlusion) may involve an inner experiential aspect of emotion in which the sensory experience may not fall into the usual acceptable range of pleasant or unpleasant. This aspect of sensation, referred to as affect, is the basis of much suffering and pleasure, including that related to the occlusion and occlusal therapy. In mentalistic terms, feelings of pleasantness and unpleasantness are correlated with "motivation or intention to respond" and with emotion. Even a simple reflex may be considered as a unit of behavior. The advantage of viewing occlusion (in terms of function and parafunction) as human behavior is that the clinician has a better understanding of functional disturbances (e.g., TMJ and muscle disorders) and the recognition that how patients feel and respond to their occlusion is an important aspect of diagnosis and dental treatment.
Motivation
Emotion is a motivational phenomenon that plays a significant role in the determination of behavior. Motivation or drive and emotional states may be the basis for oral motor behavior, which is a fundamental component of ingestive responses, and for other behaviors essential for adaptation and survival. In effect, oral motor behavior can be initiated not only by situations involving cognitive processes but also by emotive processes including homeostatic drives (e.g., hunger) concerned with the internal environment and non-homeostatic drives (e.g., fear) related to adaptation to the external environment. The external environment may begin at the interface between oral sensory receptors and external stimuli involved in oral function and parafunction. However, ideas suggesting a "hard" interface between the internal and external environment are rapidly being reevaluated in terms of functional criteria. It is no longer possible to restrict thinking to a concept of the external environment as being "out there." From a psychophysiological standpoint, an interface between the external and internal worlds may not exist.
Homeostasis
As already indicated, oral motor behavior involves the translation of thought, sensation, and emotion into actions. Implied is the idea that actions or behavior may change because of learning and that some drive or motivation alters existing responses to environmental variables. Although the neural substrate for the translation of innate drives appears to exist and regulatory behavior such as eating has clear value to the immediate survival of an individual, other oral motor behavior may not have clear antecedents in individual or group survival. However, during the development of the nervous system and motor functions, oral motor behavior may be highly dependent on homeostatic drives concerned with ingestive processes. Later oral motor behavior is an expression of the plasticity of the organism over a long period and consists of a whole complex of emotive and cognitive determinants that cannot be related easily to a hypothetical construct of homeostatic needs in the adult organism even in a teleological sense.
Execution of Motor Behavior
Although oral motor behavior is judged on the basis of observable actions, the strategy and tactics of the occlusal aspects of human behavior are based on past dental experiences and the present state of the joints, muscles, periodon-tium, contact relation of the teeth, and central nervous system. The neural mechanisms that underlie the initiation, programming, and execution of motor behavior can be described only briefly here.
Complex behavior may involve neuronal circuits called pattern generators, which, when activated, elicit stereotyped, rhythmic, and/or coordinated movements. The pattern generators for locomotion appear to be in the spinal cord and to be activated by discrete nuclei or regions in the brainstem, and they can be accessed by higher-level structures in the central nervous system. The pattern generators for chewing and swallowing are located in the brainstem medullary-pontine reticular formation. As already mentioned, limbic structures appear to have access to pattern generators.
Chewing is a type of oral motor behavior that demonstrates centrally programmed movement and in part peripherally driven movement. Controlled interaction is more often the case than either purely centrally programmed movement or purely peripherally controlled movement. Pattern generators may be part of the particular programs accessed by higher brain centers to generate complex behavior.
Swallowing
Swallowing involves the coordination of nearly 20 different muscles with motor neurons distributed from mesencephalic to posterior medullary levels. The patterning of muscular contractions is independent of the stimulus necessary to evoke swallowing. The neurons responsible for coordination include a swallowing center, in which neuronal groups fire automatically in a particular sequence when stimulated to achieve the necessary pattern of muscle activity to produce swallowing. "Triggering," or initiation of a central program, involves neurons in the motor cortex that act as command elements and control patterns of neuronal activity as well as receive feedback from the systems controlled. Thus movement may be centrally programmed (drive) and at the same time modulated by peripheral influences.
The cyclical movements of the jaw in mastication reflect past experiences, adaptive behavior, neuronal activity of the mesencephalic rhythm generator and the trigeminal motor nucleus, and the influence of oral reflexes, either conditioned or unconditioned. The pattern generator may be influenced by sensory input from the orofacial area and influences from higher centers in the central nervous system.
Summary
To understand occlusion in its broadest sense, it is necessary to consider, in addition to TMJ articulation, muscles, and teeth, some of the neurobehavioral mechanisms that give meaning to the presence and function of the masticatory system. Although many of the neural mechanisms mediating interaction between occlusion and thoughts, sensations, and emotions are complex and often indeterminate, it is possible to suggest strategies that could account for the variety of responses (physiological and psychological) that occur in function and parafunction.
The "obvious" strategy to compensate for wear of proximal contact areas is mesial migration of the teeth, and the strategy to compensate for wear of the occlusal surfaces is eruption of the teeth. The strategy for regulating the contraction of the jaw elevators to achieve a normal resting position of the mandible with a small interocclusal space is a postural reflex (stretch reflex). The overall strategy for motivation to have access to the muscles of mastication might be to provide a drive for ingestive processes, especially during the early stages of development of the masticatory system and maturation of the nervous system—swallowing in fetal life, suckling in the newborn, and chewing in the young infant.
It appears plausible, at least, that emotion may be important not only as a motivational phenomenon but also as a reflection of what is agreeable or disagreeable about something that is placed in the mouth, including items not considered to be food and perhaps even restorations that interfere with function or parafunction. Demonstration of evidence for and against strategies to explain completely neurobehavioral mechanisms of "occlusion" requires much more space than provided here.
The extensive "education" of persons through the television media, newspapers, and magazines and through professional dental care and instructions to patients not only has produced an awareness of the teeth and mouth but also has coupled these structures to a sense of health and comfort. The affect involved in such a sense of well-being about oral health involves part of the same neurobehavioral substrate underlying innate drives, motivation, and emotional states necessary for biological adaptation and survival of the species. Ingestive processes, which include oral motor responses involved in mastication, are essential for survival. Functional disturbances of the masticatory system may involve psychophysiological mechanisms that are related to the teeth and their functions. Therefore occlusal interferences to function or parafunction may then involve more than simply contact relations of the teeth; they may involve psychophysiological mechanisms of human behavior as well.
No scientific evidence is available for making a specific structure or psychophysiological mechanism the sole cause of TMJ/muscle dysfunction. However, any attempt to negate the role of the teeth in human behavior, including dysfunction, perhaps is made by those who have not had the opportunity to observe the effect on affect, favorable neu-romuscular response, and elimination of discomfort when appropriate occlusal therapy is rendered.
Unfortunately, neuroscientific evidence to separate the subjective from objective clinical observations has not lived up to its full potential. Scientific clinical studies in which true cause-and-effect relationships can be determined are difficult to design, especially when such relationships may be indirect, "on-again, off-again," and significantly influenced by the observer and other factors under natural condi-tions.52 Considerably more appropriate research is needed to establish the role of occlusion and related factors in TMJ/ muscle dysfunction.