Form and Function of the Permanent Dentition
The relationship between the form of the teeth and function is usually discussed in terms of type of food in the diet of humans, jaw movements, and protection of the perio-dontium and stimulation of the gingiva. It is also recognized that the teeth not only contribute to the digestion of food but also are important in speech and personal appearance.
The primary function of the teeth is to prepare food for swallowing and to facilitate digestion. The teeth have their respective forms to facilitate prehension, incision, and trituration of food. The dentition, joints, and muscles in humans have the form and alignment to enable the mastication of both animal and vegetable foods. This type of dentition is referred to as omnivorous.
The shapes of incisal and occlusal surfaces of the teeth are related not only to the function they perform but also to the movements of the mandible required to carry out chewing of a variety of foods. In contrast to the facts regarding many animals, only up-and-down jaw closure is possible because of the interlocking conical form of the teeth, tem-poromandibular joint (TMJ) morphology, and lack of muscles to carry out lateral movements. To understand more completely the form and function of teeth, the protective aspects of form and their functional relationships are considered.
Alignment, Contacts, and Occlusion
When the teeth in the mandibular arch come into contact with those in the maxillary arch in any functional relation, they are said to be in occlusion. The term occlusion is also used to designate the anatomical alignment of the teeth and their relationship to the rest of the masticatory system. Malocclusion is a term usually used to describe deviations in intramaxillary and/or intermaxillary relations of the teeth and/or jaws.
This fact should indicate the complexity of the process of development and eruption of the teeth into a normal occlusion, which means minimally the proper alignment, and arrangement of the teeth within each jaw and the interdigitation of the teeth between the jaws.32 In addition, each tooth (including implants) in the arch should be placed in its most advantageous angle to withstand the forces brought to bear on it.A general restorative principle states that occlusal forces in dental restorations should be directed along the long axis of the teeth (see Figure 4-17). Although this concept seems appropriate, it is not evidence based (i.e., no randomized clinical trial results support the concept). Unfortunately, at this time, no acceptable method of testing the hypothesis is available (i.e., no dynamic clinical biomechanical method, including telemetry, has determined the vector forces generated between teeth during function). However, some evidence suggests that tangential loading (see Figure 4-18) results in reduced chewing forces and that negative feedback from receptors in the periodontium mediate chewing forces. Receptor thresholds for axially directed forces appear to be higher than those for tangentially directed forces and suggest a positive feedback control on axially directed tooth forces. To position dental implants correctly, an intraoral appliance is used to guide the placement of the implant into a position and angulation consistent with angulations of opposing teeth or those suggested in Box 16-1 and Figure 16-20.
The buccal and lingual contours of the teeth have an influence on the way in which food is directed to and away from the gingival tissues. When a tooth is normally positioned, the gingival margin and sulcus have a physiological relationship to the tooth in function. Food impaction, impinging trauma from tough foods, and accumulation of dental plaque may be the consequence of malposed teeth or overcontouring or undercontouring of restorations involving buccolingual surfaces. The exact relationship between the contouring of restorations and gingival health is not clear. Ideas concerning the relationship of faulty buccal contours (undercontouring) to the initiation of gingivitis have been challenged. Plaque control by toothbrushing may be more important than simple deviations of the contour. However, overcontoured and undercontoured restorations should be avoided. Overcontouring of facial and lingual surfaces may inhibit natural cleaning by the tongue, cheeks, and passage of food and may require special toothbrushing methods.
INTERPROXIMAL FORM
Proximal contacts of approximating teeth in the arch protect the soft tissues (gingiva) between the teeth and are referred to as the interproximal spaces (Figures 4-19 and 4-20; see also Figure 5-1). The gingiva, which normally fills this pyramidal-like space and extends from the alveolar bone to and around the proximal contacts of the teeth (see Figure 5-2, B) may not fill these spaces (Figure 4-21). In the absence of correct proximal tooth contacts and marginal ridges, food impaction may occur.
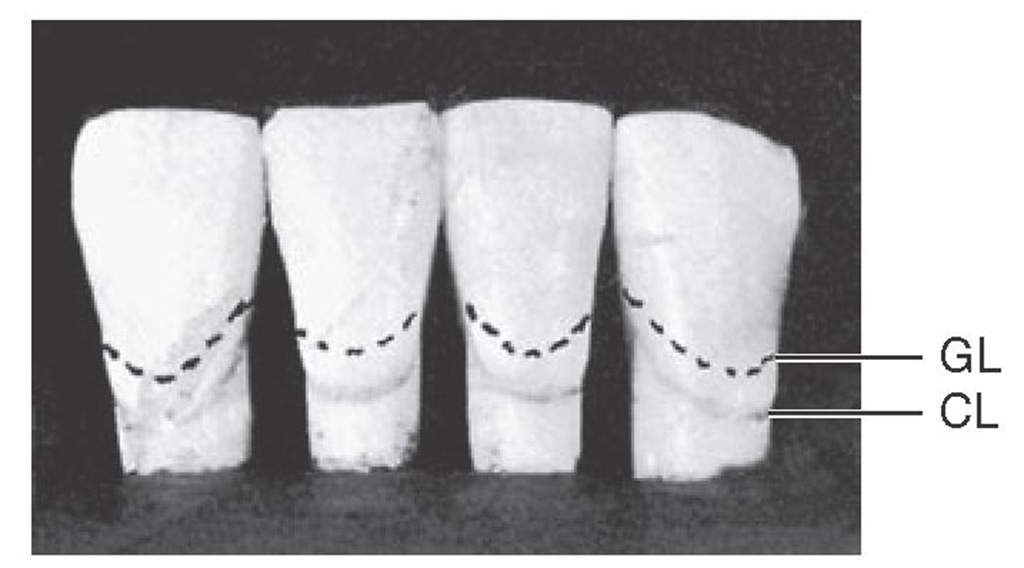
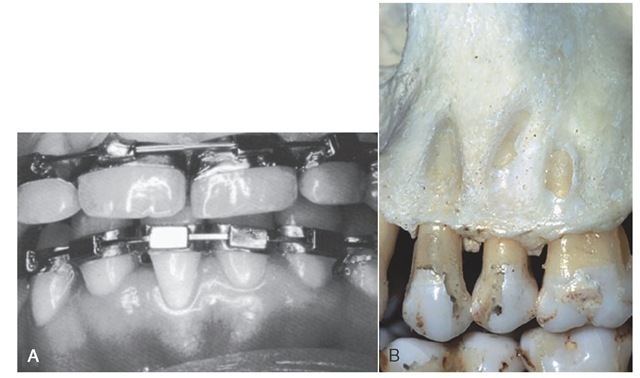
The gingiva within the interproximal space is called the gingival or interdental papilla (see Figure 5-1). Normally, the gingiva covers part of the cervical third of the tooth crowns and fills the interproximal spaces (see Figures 4-21 and 5-1). The gingival line follows the curvature but not necessarily the level of the cervical line.The gingival line and the cervical line must not be thought of as being identical; although they normally follow a similar curvature, they are seldom at the same level on the tooth. The cervical line is a stable anatomical demarcation, whereas the gingival line merely represents the gingival level on the tooth at any one period in the individual’s life, and this level is variable (e.g., gingival recession). Misalignment of the teeth may change the gingival line, which may not be conducive to the health of the tissue (e.g., partial absence of bone over the root of a tooth as in dehiscence [cleft] or fenestration [window]) (see Figure 4-21, B).
Figure 4-19 The mandibular centrals and laterals contact each other at the incisal third. The form of each tooth, plus the location of the contact areas, creates narrow pointed spaces between the teeth that differ from other interproximal spaces in other segments of the arches. GL, Variable gingival line representing the gingival level; CL, cervical line as established by the cementoenamel junction.
Figure 4-20 Contact design and interproximal (sometimes called interdental) spaces illustrated by the mandibular canine and first and second premolars. Note the variation in contact areas in relation to crown length.
Figure 4-21 Influence of malalignment of teeth on form of gingival line and bone. A, Change in gingival line (free gingival margin) of central incisor. B, Absence of bone over root of tooth in labioversion (fenestration).
Even when the teeth are in good alignment, unless the proper relation is kept between the width of each tooth at the cervix and the width at the point of contact with neighboring teeth, the spacing interdentally is changed. This is an important point to observe in clinical examinations and to maintain in approximating restorations (e.g., do not reduce the interproximal space at the expense of the interdental gingival papilla).
When considering the form of the teeth from the mesial and distal aspects, it is possible to observe a curvature on the crowns at the cervical third above the cervical line, labially or buccally and lingually. It is called the cervicoenamel ridge (see Figure 1-19), or simply cervical ridge, with the location added (buccocervical ridge, and so forth). As already indicated, this ridge should not be overcontoured or undercon-toured in full-crown restorations.
ROOT FORM
The length and shape of the root (or roots) of each tooth must be viewed as important; the canine, for instance, because of its position and the work required of it, would be torn out of its socket or at least displaced by forces brought to bear on it if the root were not of extra size and length. Fracture would be imminent if the root were not larger than that of other single-rooted teeth. The root form therefore is associated with the overall form of the tooth and the work it has to do.
The angle at which the incisal and occlusal surfaces of the tooth crowns are placed with respect to the root bases is also important. The mesial view of an anterior tooth will show that the incisal ridge or cusp is centered over the root (see Figure 1-4). The mesial view of an upper first molar, which is a multicusped tooth, demonstrates the same principle. The points on the occlusal surface that are contacted by opposing teeth will prove to be well within the confines of the root base of the crown. The measurement from cusp tip to cusp tip buccolingually is much less than the buccolingual diameter of the root base (see Figure 1-4). Note the flare of the roots for stabilization.
The length and shape of the roots, the angles at which the incisal and occlusal surfaces are placed with respect to the roots, sufficient dimensions for strength, and an efficient design for thorough work with resistance against lines of force suggest their importance to occlusal stability.
OCCLUSAL CURVATURE
When occlusion is considered, the concept of what constitutes normalcy arises.Normal implies a situation that is found commonly in the absence of disease or disorders and that exhibits an associated range of values that reflects the adaptive physiological range of a dynamic biological system, including the masticatory system.31 Therefore one must be careful not to attach rigid biomechanical significance to observations that are not yet evidence based (i.e., verified by appropriately designed clinical trials). It is also important not to reject clinical procedures based on statistically significant differences when the biological significance of the difference cannot be determined.
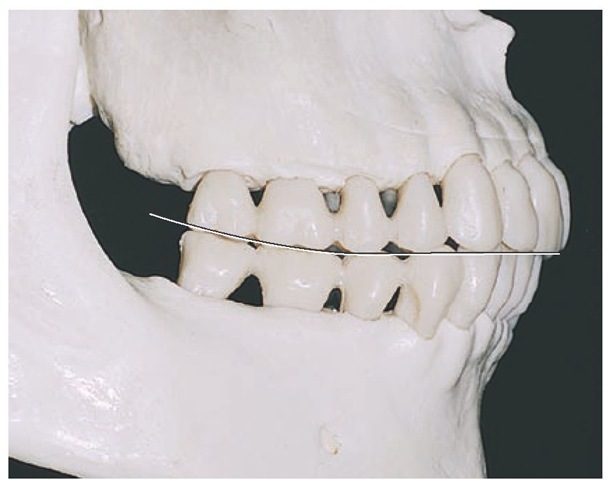
Figure 4-22 Teeth are in the intercuspal position (ICP) or centric occlusion (CO). The curved line is the curve of Spee.
It can be observed that the occlusal and incisal surfaces of all the crowns taken together in either arch do not contact a flat plane. For example, when the teeth are viewed from a point opposite the first molars buccally, a line following the occlusal and incisal surfaces describes a curve. Graf von Spee described this curvature of natural teeth originally in the German literature in 1890, and for that reason, it is called the curve of Spee (Figure 4-22). No acceptable scientific evidence exists that the occlusion should be spherical (i.e., that each cusp and incisal edge touch or conform to a segment of the surface of a sphere). This kind of curvature suggested by the lingual inclination of the mandibular molars is the basis for the curve of Wilson (i.e., the curvature of the mandibular teeth is concave and that of the maxillary teeth convex). A template for these curvatures cannot be used to set teeth in complete dentures or to perform full-mouth oral rehabilitation. The degree of anterior-posterior curvature is related to the amount of anterior guidance that is needed to obtain posterior disclusion of the teeth in lateral and protrusive mandibular movements.