Permanent Dentition
The permanent dentition consisting of 32 teeth is completed from 18 to 25 years of age if the third molar is included.
Apparently there are four or more centers of formation (developmental lobes) for each tooth. The formation of each center proceeds until a coalescence of all of them takes place. During this period of odontogenesis, injury to the developing tooth can lead to anomalous morphological features (e.g., peg-shaped lateral incisor). Although no lines of demarcation are found in the dentin to show this development, signs are found on the surfaces of the crowns and roots; these are called developmental grooves (see Figure 4-12, B). Fractures of the teeth occur most commonly along these grooves (see Figure 13-26 ).
The follicles of the developing incisors and canines are in a position lingual to the deciduous roots (see Figures 2-7 and 2-11; see also Figure 3-4).
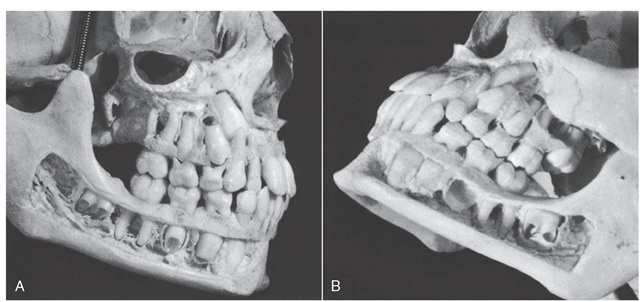
The developing premolars, which eventually take the place of deciduous molars, are within the bifurcation of primary molar roots (Figure 2-13, A and B). The permanent incisors, canines, and premolars are called succedaneous teeth because they take the place of their primary predecessors.
The central incisor is the second permanent tooth to emerge into the oral cavity. Eruption time is quite close to that of the first molar (i.e., tooth emergence occurs between 6 and 7 years) (Table 2-2). As with the first molar, at 6 years 50% of individuals have reached the stage considered to be the age of attainment of the stage or, more specifically, the age of emergence for the central incisor. The mandibular permanent teeth tend to erupt before maxillary teeth. The mandibular central incisor usually erupts before the maxillary central incisor (see Figure 2-12) and may erupt simultaneously with or even before the mandibular first molar. The mandibular lateral incisor may erupt along with the central incisor.
Before the permanent central incisor can come into position, the primary central incisor must be exfoliated. This is brought about by the resorption of the deciduous roots. The permanent tooth in its follicle attempts to move into the position held by its predecessor. Its influence on the primary root evidently causes resorption of the root, which continues until the primary crown has lost its anchorage, becomes loose, and is finally exfoliated. In the meantime, the permanent tooth has moved occlusally so that when the primary tooth is lost, the permanent one is at the point of eruption and in proper position to succeed its predecessor.
Mandibular lateral incisors erupt very soon after the central incisors, often simultaneously. The maxillary central incisors erupt next in chronological order, and maxillary lateral incisors make their appearance about 1 year later (see Table 2-2 and Figures 2-3 and 2-4). The first premolars follow the maxillary laterals in sequence when the child is about 10 years old; the mandibular canines (cuspids) often appear at the same time. The second premolars follow during the next year, and then the maxillary canines follow. Usually, the second molars come in when the individual is about 12 years of age; they are posterior to the first molars and are commonly called 12-year molars.
Figure 2-13 A, View of the right side of the skull of a child of 9 to 10 years of age. Note the amount of resorption of the roots of the primary maxillary molars, the relationship of the developing premolars above them, and the open pulp chambers and the pulp canals in the developing mandibular teeth. The roots of the first permanent molars have been completed. B, Left side. Note the placement of the permanent maxillary canine and second premolar, and the position and stage of development of the maxillary second permanent molar. The bony crypt of the lost mandibular second permanent premolar is in full view. Note the large openings in the roots of the mandibular second permanent molar.
Table 2-2 Chronology of Permanent Teeth*
Il, Central incisor; I2, lateral incisor; C, canine; Pl, first premolar; P2, second premolar; Ml, first molar; M2, second molar; M3, third molar. *See Tables 2-3 and 2-4 in Tooth Formation Standards for detailed presentation of the data.
The maxillary canines occasionally erupt along with the second molars, but in most instances of normal eruption, the canines precede them somewhat.
The third molars do not come in until the age 17 or later. Considerable posterior jaw growth is required after the age of 12 to allow room for these teeth (Figure 2-14). Third molars are subject to many anomalies and variations of form. Insufficient jaw development for their accommodation complicates matters in the majority of cases. Individuals who have properly developed third molars in good alignment are very much in the minority. Third-molar anomalies and variations with the complications brought about by misalignment and subnormal jaw development comprise a subject too vast to be covered here. Figure 2-15 shows an anatomical specimen with a full complement of 32 teeth.
Size of Teeth
The size of teeth is largely genetically determined. However, marked racial differences do exist, as with the Lapps, a population with perhaps the smallest teeth, and the Australian aborigines, with perhaps the largest teeth.22 Gender-size dimorphism differences average about 4% and are the greatest for the maxillary canine and the least for the incisors.23 Often encountered is disharmony between the size of the teeth and bone size.
Dental Pulp
The dental pulp is a connective tissue organ containing a number of structures, among which are arteries, veins, a lymphatic system, and nerves. Its primary function is to form the dentin of the tooth. When the tooth is newly erupted, the dental pulp is large; it becomes progressively smaller as the tooth is completed. The pulp is relatively large in primary teeth and also in young permanent teeth (see Figure 3-9). The teeth of children and young people are more sensitive than the teeth of older people to thermal change and dental operative procedures (heat generation). The opening of the pulp cavity at the apex is constricted and is called the apical foramen. The pulp keeps its tissue-forming function (e.g., to form secondary dentin), especially with the advance of dental caries toward the pulp. The pulp cavity becomes smaller and more constricted with age (see Figure 13-3). The pulp chamber within the crown may become almost obliterated with a secondary deposit (e.g., osteoden-tin). This process is not so extensive in deciduous teeth.
Figure 2-14 Development of the maxillary and mandibular third molars.
Cementoenamel Junction
At the cementoenamel junction (CEJ) (see Figures 1-3 and 1-4), visualized anatomically as the cervical line, the following several types of junctions are found: (1) the enamel overlapping the cementum, (2) an end-to-end approximating junction, (3) the absence of connecting enamel and cementum so that the dentin is an external part of the surface of the root, and (4) an overlapping of the enamel by the cementum. These different junctions have clinical significance in the presence of disease (e.g., gingivitis, recession of the gingiva with exposure of the CEJ, loss of attachment of the supporting periodontal fibers in periodontitis); cervical sensitivity, caries, and erosion; and placement of the margins of dental restorations.
The CEJ is a significant landmark for probing the level of the attachment of fibers to the tooth in the presence of periodontal diseases. Using a periodontal probe (Figure 2-16, A), it is possible to relate the position of the gingival margin and the attachment to the CEJ (see Figure 2-16, B). Probing is done clinically to determine the level of perio-dontal support (i.e., regardless of whether a loss of perio-dontal attachment due to periodontal disease has occurred, as with pathologically deepened gingival crevices [periodontal pockets]).
Figure 2-15 Maxillary (A) and mandibular (B) arches with full complement of 32 teeth.
The clinician should be able to envision the CEJ of each tooth and relate it to areas of risk (see Figures 5-25 and 5-26) (e.g., enamel projection into the bifurcation of the mandibular molar [see Figure 2-16, C]). The enamel extension is apical to its normal CEJ level and is a risk factor for periodontal disease because the periodontal fibers, which are imbedded in cementum to support the tooth, are not in their usual position and do not act as a barrier to the advance of periodontal disease. In effect, the epithelial attachment over the surface of the enamel, which does not have this kind of attachment, may become detached in the narrow and difficult-to-clean bifurcation area because of plaque and calculus. Thus enamel projections into buccal and lingual bifurcations are considered to increase vulnerability to the advance of periodontal disease.24
Thus the location and nature of the CEJ are more than descriptive terms used simply to describe some aspect of tooth morphology; they have some clinical significance. This consideration is also true for the cervical line; it is more than just a line of demarcation between the anatomical crown and the root of a tooth. It may be necessary to determine the nature, location, and pathological changes occurring at the CEJ to make a diagnosis of and to treat, for example, cervical caries, keeping in mind that the CEJ generally lies apical to the epithelial attachment and gingival margin in young adults (see Figures 5-2 and 5-27).
Figure 2-16 A, Periodontal probe divided into 3-mm segments. B, Probe at the level of attachment (LA). Probe indicates a pathologically deepened crevice of 6 mm and a loss of attachment of 3+ mm. C, Enamel projection into the bifurcation of a mandibular molar. CEJ, Cementoenamel junction; FGM, free gingival margin.
Figure 2-17 Shown in this radiograph are 6-year molars in position, roots of primary teeth being resorbed, and formation of succedaneous teeth.
Dental Age
Dental age is generally based on the formation or eruption of the teeth. The latter is usually based on the time that the teeth emerge through the mucous membrane or gingiva, which is, in effect, a single event for each tooth. However, the formation of teeth can be viewed as being continuous throughout the juvenile years. When the last tooth has been completed, the skeleton is approaching complete maturation.14 Later attrition and wear may be used to estimate chronological age,25 but the estimation of adult age at best is only on the order of ±5 years.26 Estimation of juvenile age is more precise than that of adult age.
Chronologies of prenatal tooth formation are based generally on dissected fetal material (see Figures 2-3 and 2-7); postnatal development chronologies are most often based on radiological data (Figures 2-17 and 2-18),27 but not always. Thus chronologies based on any single method are not usually feasible.
Figure 2-18 Panoramic radiograph of a child about 7 years of age. This type of examination is of great value in registering an overall record of development.
The dentition may be considered to be the single best physiological indicator of chronological age in juveniles.14 A knowledge of dental age has practical clinical applications; however, it is recognized that the coverage of these applications here must be brief. When indicated, references to a more detailed coverage are provided. Values for predicting age from stages of the formation of permanent mandibular teeth are considered in the section Tooth Formation Standards in this topic.
Dental age has been assessed on the basis of the number of teeth at each chronological age7 or on stages of the formation of crowns and roots of the teeth.14 Dental age during the mixed dentition period (transition from primary to permanent dentition) may be assessed on the basis of which teeth have erupted, the amount of resorption of the roots of primary teeth, and the amount of development of the permanent teeth.28
Dental age can reflect an assessment of physiological age comparable to age based on skeletal development, weight, or height.29 When the teeth are forming, the crowns and roots of the teeth appear to be the tissues least affected by environmental influences (nutrition, endocrinopathies, etc.); however, when a substance such as the antibiotic tetracycline (Figure 2-19, A) is ingested by the mother during certain times of the development of the dentitions, significant discoloration from yellow to brown to bluish violet and from part (cervical) to all of the enamel may occur.30,31
The benefits of fluoride for the control of dental caries are well established. However, its widespread use has resulted in an increasing prevalence of fluorosis (see Figure 2-19, B) in both nonfluoridated and optimally fluoridated popula-tions.32 Parents should be advised about the best early use of fluoride to reduce the prevalence of clinically noticeable fluorosis. Children under age 6 should use only a pea-sized amount of fluoride toothpaste; parents should consult their dentists concerning the use of fluoride toothpaste by children under age 2 years.33
Dental development may be based also on the emergence (eruption) of the teeth; however, because caries, tooth loss, and severe malnutrition may influence the emergence of teeth through the gingiva,11,12 chronologies of the eruption of teeth are less satisfactory for dental age assessment than those based on tooth formation. In addition, tooth formation may be divided appropriately into a number of stages that cover continuously the development of teeth34,35 in contrast to the single episode of tooth eruption. The stages of development are considered in the section Tooth Formation Standards in this topic.
Figure 2-19 A, Tetracycline staining. B, Enamel fluorosis.
The importance of the emergence of the teeth to the development of oral motor behavior is often overlooked, undoubtedly partly as a result of the paucity of information available. However, the appearance of the teeth in the mouth at a strategic time in the maturation of the infant’s nervous system and its interface with the external environment must have a profound effect on the neurobehavioral mechanisms underlying the infant’s development and learning of feeding behavior, particularly the acquisition of masticatory skills.
Tooth Formation Standards
Events in the formation of human dentition are based primarily on data from studies of dissected prenatal anatomic material and from radiographic imaging of the teeth of the same subjects over time (longitudinal data) or of different subjects of different ages seen once (cross-sectional data). From these kinds of studies, both descriptive information and chronological data may be obtained. To assemble a complete description or chronology of human tooth formation, it would seem necessary to use data based on more than one source and methodology. However, it is not easy to define ideal tooth formation standards from studies that examine different variables and use many different statistical methods. Subjects surveyed in most studies of dental development are essentially of European derivation, and population differences can only be established by studies that share methodology and information on tooth formation in populations of nonwhite/non-European ancestry.14
The age of emergence of teeth has been established for a number of population groups, but much less is known about chronologies of tooth formation.
![tmp182-68_thumb[1] tmp182-68_thumb[1]](http://what-when-how.com/wp-content/uploads/2012/05/tmp18268_thumb1_thumb.jpg)
![tmp182-69_thumb[1] tmp182-69_thumb[1]](http://what-when-how.com/wp-content/uploads/2012/05/tmp18269_thumb1_thumb.jpg)
![tmp182-70_thumb[1] tmp182-70_thumb[1]](http://what-when-how.com/wp-content/uploads/2012/05/tmp18270_thumb1_thumb.jpg)
![tmp182-71_thumb[1] tmp182-71_thumb[1]](http://what-when-how.com/wp-content/uploads/2012/05/tmp18271_thumb1_thumb.jpg)
![tmp182-72_thumb[1] tmp182-72_thumb[1]](http://what-when-how.com/wp-content/uploads/2012/05/tmp18272_thumb1_thumb.jpg)
![tmp182-73_thumb[1] tmp182-73_thumb[1]](http://what-when-how.com/wp-content/uploads/2012/05/tmp18273_thumb1_thumb.jpg)
![tmp182-74_thumb[1] tmp182-74_thumb[1]](http://what-when-how.com/wp-content/uploads/2012/05/tmp18274_thumb1_thumb.jpg)
![tmp182-75_thumb[1] tmp182-75_thumb[1]](http://what-when-how.com/wp-content/uploads/2012/05/tmp18275_thumb1_thumb.jpg)
![tmp182-76_thumb[1] tmp182-76_thumb[1]](http://what-when-how.com/wp-content/uploads/2012/05/tmp18276_thumb1_thumb.jpg)






