Cardiac resynchronization therapy trials in patients with moderate to severe heart failure
The Multicenter InSync Randomized Clinical Evaluation (MIRACLE) trial involved implanting a CRT only device (with biventricular pacing only, no Defibrillator component). Patients were randomized if they had an LVEF < 35% and NYHA functional class III or IV heart failure despite optimal medical therapy and QRS duration of > 130 milliseconds (msec). a total of 453 patients were randomized after successful implantation of a CRT device to CRT ON (228 patients) and CRT OFF (225 patients) status for a period of 6 months (Abraham et al. 2002). The primary endpoint included the 6 minute walk test, quality of life score and NYHA class. A total of 453 patients were enrolled in the study. Patients assigned to CRT ON had 13% improvement in the 6-minute walk and in the quality of life score. The secondary endpoints also improved in the CRT ON arm including improvement in LVEF as well as peak oxygen consumption (VO2). The protocol specified safety variables that included an analysis of death or worsening heart failure. There was no difference in overall mortality (HR 0.73, 95% CI 0.34 to 1.54, p=0.40) but there was a decrease in hospitalization (HR 0.50, 95% CI 0.28 to 0.88, p= 0.02). The study did not specify mortality as a primary end point and was not powered enough to show differences in mortality.
The Multicenter Insync ICD randomized Clinical Evaluation (MIRACLE ICD) trial had a similar design to the MIRACLE study. Patients were included if they had LVEF < 35%, NYHA class III to IV despite optimal medical therapy and QRS duration of > 130 milliseconds and were at high risk of death from ventricular arrhythmias (Young et al. 2003). Almost two thirds of patients had an ischemic etiology and at least 60% were on beta blockers. All patients received a CRT-D device (total of 369 patients) of whom 182 had CRT OFF (controls) and 187 had CRT ON. At 6 months follow up, all patients with the CRT ON showed an improvement in the NYHA class (p=0.007) and the quality of life score (p=0.02). There was no difference in 6-minute walk distance (p=0.36) compared to the control group. Of the secondary endpoints, There was an improvement in the peak VO2 (p=0.04) and a trend towards reductions in the LV end systolic and end diastolic dimensions (p=0.06 for both) compared to the control group. The study did not show any difference in mortality (p=0.96) or hospitalization (p=0.69) between the two groups. Similar the to MIRACLE study, the MIRACLE ICD study had short follow up and was not powered enough to detect difference in mortality.
The CONTACT CD Biventricular Pacing study enrolled 490 patients with LVEF <35%, QRS > 120 msec and NYHA class II to IV despite optimal medical therapy and conventional indications for ICD implantation. Patients were assigned to CRT ON (245 patients) and CRT OFF (245 patients) for up to 6 months (Higgins et al. 2003). The primary endpoint was progression of heart failure, defined as all cause mortality, hospitalization for HF and ventricular tachycardia or ventricular fibrillation requiring device intervention. Secondary endpoints included peak oxygen consumption (VO2), 6-minute walk, NYHA class, quality of life as well as echocardiographic analysis. Patients with CRT ON had a 15% reduction in the composite HF progression but this was not statistically significant (p=0.35). However, patients with NYHA class III and IV had an improvement in the peak VO2 (p=0.003), 6-minute walk (p=0.03), NYHA class (p=0.0006) and QOL (0.02). Patients who had NYHA class I or II didn’t show any improvement in any of the secondary parameters. One important finding in CONTACT CD trial is that patients with CRT ON had significant reductions in LV internal diameter in diastole (LVIDd) (p<0.001) LV internal diameter in systole (LVIDs) (p<0.001), and LVEF (p=0.02). Even patients with NYHA II had significant improvement in the LV dimensions with CRT ON. The study was not adequately powered to detect a statistical difference in the primary endpoint of composite HF progression. This was due to the fact that the observed event rates were half the expected while designing the trial.
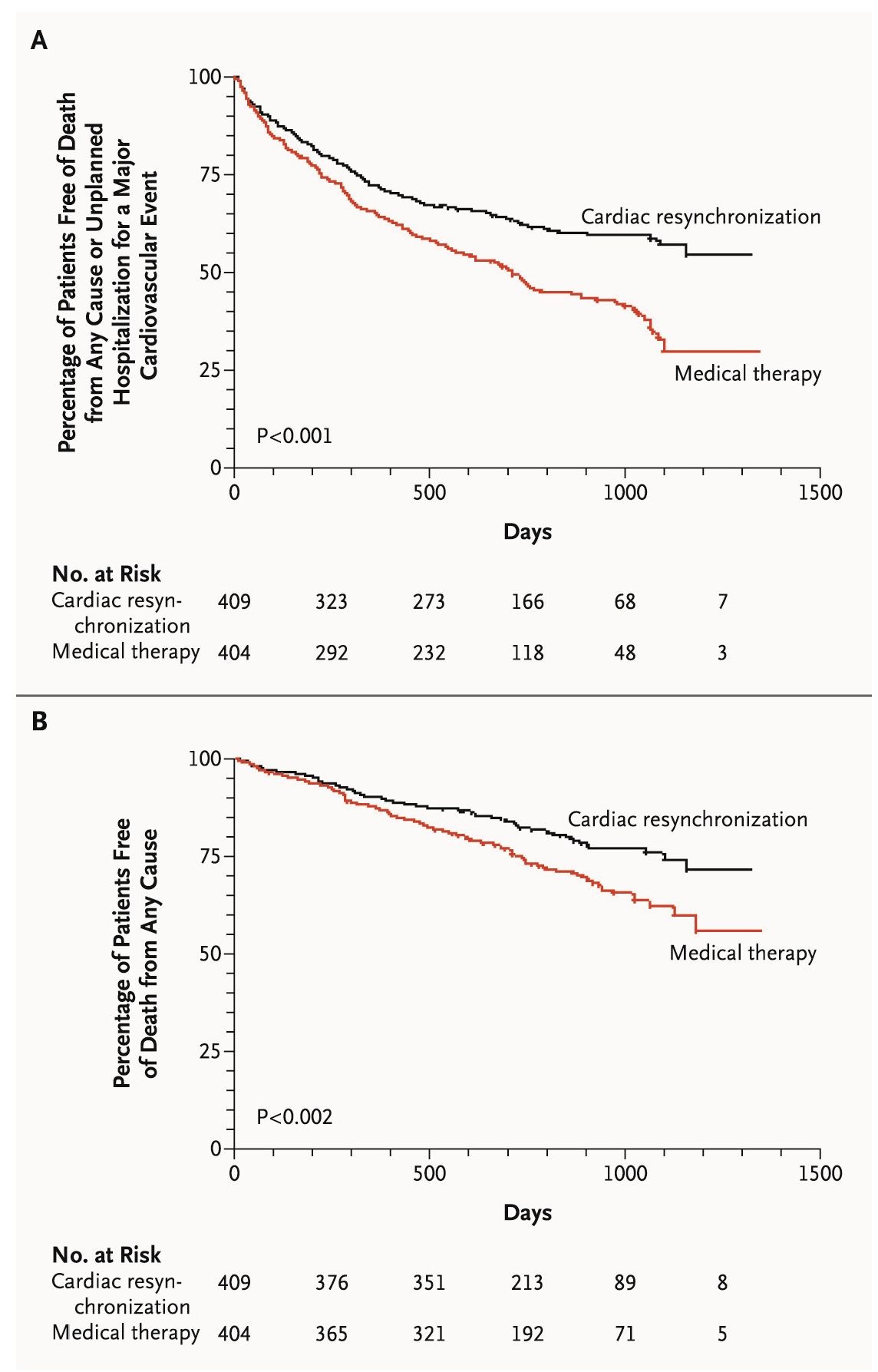
The Comparison of Medical Therapy, Pacing and Defibrillation on Heart Failure Study (COMPANION) enrolled 1520 patients with LVEF< 35%, NYHA class III or IV heart failure despite optimal medical therapy and QRS duration of > 120 msec in a 1:2:2 fashion to medical therapy versus biventricular pacing alone (CRT only) versus biventricular pacing with defibrillation (CRT-D) (Bristow et al. 2004). Almost 59% of the patients had ischemic cardiomyopathy and 82% were NYHA class III. The primary endpoint was death or hospitalization for any cause while the secondary endpoints included death from any cause. As compared to the medical therapy group, patients with CRT only (Biventricular pacemaker only) decreased the risk of death or hospitalization from any cause (HR 0.81, p=0.014) as did CRT-D group (biventricular defibrillator group) (HR 0.80, p-0.01). CRT only decreased the risk of death by 24% (p=0.059) while CRT-D decreased the risk of death by 36% (p=0.003). COMPANION was the first trial to show that CRT improves the quality of life, symptoms as well as decrease the risk of death or hospitalization for heart failure. The Cardiac Resynchronization-Heart Failure Study (CARE HF) randomized 813 patients with LVEF < 35%, NYHA class III to IV heart failure despite optimal medical therapy and QRS duration > 120 msec (patients with QRS between 120 to 149 msec had to have two of the three echocardiographic parameters of dys-synchrony: an aortic pre-ejection delay of > 140 msec, an interventricular mechanical delay of > 40 msec or delayed activation of the posterolateral wall of the LV (Cleland et al. 2005). Patients assigned to the CRT group received biventricular pacemaker (no defibrillators). The primary endpoint was the composite of death or unplanned hospitalization for a major cardiovascular event. Secondary endpoint was death from any cause. Other secondary endpoints included quality of life, improvement in NYHA class and echocardiographic parameters (mainly ventricular function, mitral regurgitation). After a mean follow up of 29.4 months, patients treated with CRT (total of 409 patients) had less death or hospitalization for cardiovascular event (HR 0.63, 95% CI 0.51 to 0.77, p< 0.001) compared to patients with medical therapy only (404 patients). CRT also improved survival (HR 0.64, 95% CI 0.48 to 0.85, p< 0.002) (Figure 3). Patients with CRT had improvement in NYHA class, better QOL, and showed smaller area of mitral regurgitation and an improvement in the LVEF at 3 and 18 months post CRT. CARE HF was the first CRT only trial to show that biventricular pacing alone can improve survival. The lack of mortality benefit from CRT only arm in COMPANION might be due to the fact that patients in COMPANION trial were sicker, with over 55% having ischemic cardiomyopathy with mean LVEF of 22% while patients in CARE HF had a mean LVEF of 25% and only a third of them had ischemic cardiomyopathy. The added benefits of CRT on survival will be examined later by the RAFT study.
The Cardiac Resynchronization Therapy in Patients with Heart Failure and Narrow QRS (RethinQ) study randomized 172 patients with history of NYHA class III heart failure, LVEF <35% despite optimal medical therapy and QRS duration of <130 msec with evidence of mechanical dys-synchrony on echocardiography (defined as septal to lateral or septal to inferior wall delay >65 msec as measured by tissue doppler or septal to posterior wall delay >130 msec as measured by M Mode echocardiography (Beshai et al. 2007). Primary outcome was the improvement of peak oxygen consumption of > 1 ml per kilogram of body weight per minute during cardiopulmonary exercise testing.
Fig. 3. Kaplan-Meier Estimates of the Time to the Primary End point of death or unplanned hospitalization for a major cardiovascular event (Panel A) and Death from any cause (Panel B).
The secondary outcomes were improvements in the 6 minute walk test, NYHA class and quality of life. All patients had a CRT device implantation and were assigned to CRT ON (n=76) or no CRT (n=80). After follow up of 6 months, there was no difference in the primary endpoint between patients with CRT and patients with no CRT (46% vs 44%, p=0.63). Patients in the CRT group with a QRS > 120 msec had significant improved in peak oxygen consumption at 6 months follow up (0.02) but patients in the CRT group with QRS <120 msec didn’t have improvement in peak oxygen consumption at 6 months (p=0.45). There was no improvement in the quality of life measures (as measured by Minnesota living with Heart failure questionnaire) and in the 6-minute walk test in both groups of patients regardless of the QRS duration. Patients with CRT on had an improvement in the NYHA class at 6 months compared to patients with no CRT regardless of the QRS duration (p=0.006).
Cardiac resynchronization therapy trials in patients with mild heart failure
The Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction Study (REVERSE) trial was the first CRT trial to include patients with NYHA II and asymptomatic NYHA class I patients with LV dysfunction. A total of 610 patients underwent CRT device implantation and were randomized to CRT ON (419 patients) and CRT OFF (191 patients). Inclusion criteria included LVEF <40%, NYHA functional class I or II heart failure with a QRS 120 msec (Linde et al. 2008). Mean follow up was for 12 months. The primary end point was the heart failure (HF) clinical composite response (which included heart failure hospitalization, NYHA class and global assessment score). Secondary endpoints included LV end-systolic volume index and hospitalization for worsening HF. There was no difference between the two groups in the HF clinical composite score (which compared only the percent worsened) (p = 0.10). Patients assigned to CRT-ON experienced a greater improvement in LV end-systolic volume index (-18.4 ± 29.5 ml/m2 vs. -1.3 ± 23.4 ml/m2, p < 0.0001) and had a 53% relative risk reduction in time to first HF hospitalization (p=0.03). There was no difference between the two groups in the 6- minute walk test and in the quality of life scores. The improvement in LV end systolic volume index was similar in patients with NYHA I and NYHA II. The rate of LV lead implantation related complications was 10%. These complications were mostly due to LV lead dislodgement or diaphragmatic stimulation.
The Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization therapy (MADIT-CRT) randomized 1820 patients with LVEF <30%, NYHA class I or II HF and QRS duration of > 130 msec in a 3:2 design to cardiac resynchronization therapy with defibrillation capacity (CRT-D) (1089 patients) and to ICD only group (731 patients). The primary endpoint was death from any cause or hospitalization for heart failure (Moss et al. 2009). Secondary endpoints included death from any cause and heart failure hospitalization alone. Follow up was for 4.5 years. Patients who received CRT-D had lower risk of death or hospitalization for heart failure (HR 0.66, 95% CI of 0.52 to 0.84, p=0.001) compared to the ICD only group. There was no difference in death from any cause between the two groups (HR 1.00, 95% CI of 0.69-1.44, p=0.99). The rate of hospitalization was significantly lower in the CRT-D group compared to the ICD only group (HR 0.59, 95% CI of 0.47 to 0.74, p<0.001). Patients with ischemic and non-ischemic cardiomyopathy benefited similarly from CRT. Subanalysis of MADIT CRT showed that female patients (n=453, 25%) were more likely to have non-ischemic cardiomyopathy and left bundle branch block (LBBB) compared to male patients. Female patients were more likely to have reverse remodeling by echocardiography and had a 69% relative risk reduction of death or heart failure (HR of 0.31, p<0.001) (Arshad et al.). Patients with QRS duration > 150 msec had greater benefit from CRT (HR 0.48, 95% CI 0.37 to 0.64) compared to patients with QRS duration < 150 msec (HR 1.06, 95% CI 0.74 to 1.52, p=0.001 for interaction). Patients assigned to the CRT-D arm had significant reduction in LV end diastolic volume index (-26.2 versus -7.4 mL/m2), LV end systolic volume index (-28.7 versus -9.1 mL/m2 ) as well as improvement in LVEF (11% versus 3%) compared to the ICD only group. After adjusting for baseline variables, for every 10% reduction in the LV end diastolic volume index, there was a 40% reduction in the risk of death or heart failure hospitalization (Solomon et al.). Furthermore MADIT CRT measured echocardiographic response as a decrease in LV end systolic volume > 25%. Using this definition, 529 patients assigned to the CRT-D arm responded to CRT and were less likely to have ventricular tachyarrhythmia (VT or VF) and inappropriate shocks. Analysis of the data showed that for every 10% reduction in LV end systolic volume, there is a 20% decrease in the risk of ventricular tachyarrhythmias (p<0.001) even after adjusting for other clinical risk factors including age, QRS duration, left bundle branch block, and blood urea nitrogen (BUN) (Barsheshet et al.).
The Resynchronization-Defibrillation for Ambulatory Heart Failure Trial (RAFT) randomized 1798 patients with LVEF <30%, NYHA II to III heart failure and QRS duration of >120 msec or a paced QRS duration of > 200 msec to either ICD alone or Biventricular defibrillator (CRT-D) (Tang et al.). Mean follow up was for 40 months and the primary endpoint was death or hospitalization for heart failure while secondary endpoints included death from any cause, death from cardiovascular cause and heart failure hospitalization. Most of the patient had NYHA class II (80%) and had ischemic etiology (64%). Patients with CRT-D had less death and heart failure hospitalization compared to the ICD group (HR 0.75, 95% CI of 0.64 to 0.87, p <0.001). CRT-D also improved survival compared to ICD alone (HR 0.75, 95% CI 0.62-0.91, p=0.003) (Figure 4). There was less heart failure hospitalizations with CRT-D group compared to ICD only group (HR 0.68, 95% CI of 0.56 to 0.83, p<0.001). There was no difference in the primary and secondary endpoints in patients with ischemic and non-ischemic cardiomyopathy. Patients with wider QRS (>150 milliseconds) had better survival than patients with QRS < 150 msec. However, patients with CRT-D had more 30 days adverse events compared to the ICD alone group (p<0.001), these were mostly device related complications.
These trails established CRT as an important therapy for patients with heart failure, LVEF < 35% and NYHA class III to IV. The only measure of dys-synchrony that stood the test of time is the QRS duration. Even though there is disagreement in the literature in the measurement of "response". At least two thirds of patients with CRT show clinical improvement in their functional status. CRT has been proven to improve survival independently as shown in the CARE HF trial, and it also improves survival above and beyond ICD therapy as shown in the RAFT trial. The guidelines for implantation for CRT in patients with systolic heart failure are listed in Table 5. These guidelines were written in 2008, and do not reflect the recent evidence of the benefits of CRT in milder forms of heart failure that was found in the REVERSE, MADIT CRT and RAFT trials.
Fig. 4. Kaplan Meier Estimates of Death or Hospitalization for Heart Failure (Panel A) and Death from Any Cause (Panel B).
|
Class I (General agreement of benefit of CRT) |
|
|
1. |
CRT with or without an ICD is indicated for the treatment of for patients are in sinus rhythm who have LVEF < 35%, a QRS duration > 120 milliseconds, NYHA functional Class III or ambulatory Class IV heart failure symptoms with optimal recommended medical therapy. |
|
Class IIa (Weight of evidence is in favor of CRT) |
|
|
1. |
CRT with or without an ICD is indicated for patients in sinus rhythm who have LVEF < 35%, a QRS duration > 120 msec, NYHA functional class III or ambulatory class IV heart failure symptoms with optimal recommended medical therapy. |
|
2. |
CRT is reasonable for patients with LVEF < 35%, QRS duration >120 milliseconds, NYHA functional Class III or ambulatory Class IV heart failure symptoms with optimal recommended medical therapy and who have frequent dependence on ventricular pacing. |
|
Class IIb (Efficacy of CRT is less well established) |
|
|
1. |
CRT may be considered for patients with LVEF < 35% with NYHA functional Class I or II symptoms who are receiving optimal recommended medical therapy and who are undergoing implantation of a permanent pacemaker and/or ICD with anticipated frequent ventricular pacing. |
|
Class III (General agreement that CRT is less effective and might be harmful) |
|
|
1. |
CRT is not indicated for asymptomatic patients with reduced LVEF in the absence of other indications for pacing. |
|
2. |
CRT is not indicated for patients whose functional status and life expectancy are limited predominantly by chronic non-cardiac conditions. |
Table 5. Recommendations for cardiac resynchronization therapy based on the ACC/AHA/HRS 2008 Guidelines for Device Based Therapy. CRT: Cardiac Resynchronization Therapy. ICD: Implantable Cardioverter Defibrillator. NYHA: New York Heart Association