Cardiovascular disease (CVD)
The most common form of cardiovascular disease is called atherosclerosis, a disease of the arteries that can strike at any age, although it is not a serious threat until our fifth or sixth decades. This disease is caused by an excess of low-density lipoprotein (LDL) in the blood, which leads to the buildup of fatty deposits (plaques) in the arteries. These deposits reduce the flexibility of the arteries, thus increasing blood pressure; they can also impede or block the flow of blood. The most common and deadliest form of atherosclerosis affects the coronary arteries, the vessels that carry blood to the heart. If coronary arteries become blocked or otherwise damaged, the cardiomyocytes (heart muscle cells) die from lack of oxygen. In serious cases, this can lead to a massive heart attack and death of the patient. In milder cases, damage to the heart is minimal, but coronary circulation is insufficient to allow the patient a normal lifestyle.
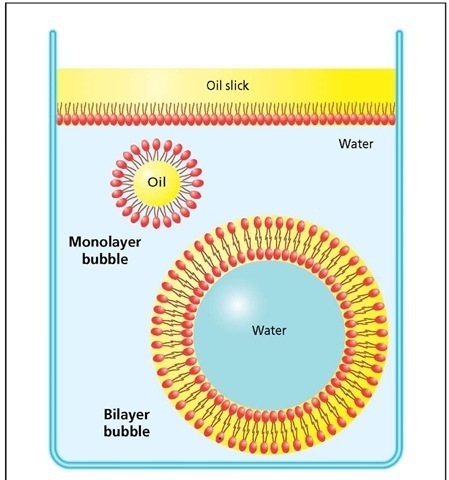
To fully appreciate the onset and complications of this disease, one needs to take a brief journey back in time, when life first appeared on earth 3.5 billion years ago. The connection between CVD and the origin of life may seem tenuous, but the events of those long-gone days have, in a sense, come back to haunt us. Life on Earth began when single cells appeared in the oceans, very close to shore where the concentration of dissolved nutrients was at its highest level. Among those nutrients was a fatty compound known as phospholipid. The first cells were microscopic phospholipid bubbles that contained a tiny drop of ocean water filled with nutrients and other useful molecules; they wrapped the phospholipid around themselves the way people wrap themselves in warm blankets or raincoats. Phospholipids not only protected the cells from the external world, but they made it possible for the cells to regulate their internal environment. As cells evolved, they improved the functional properties of their phospholipid "blanket" by adding cholesterol to it. The functional properties of phospho-lipids mixed with cholesterol are so important and so fundamental that to this day all cells are surrounded by a phospholipid membrane that contains cholesterol.
Phospholipid bubbles. Phospholipid molecules have a hydrophilic head-end (red ovals) and two hydrophobic tails that do not mix with water and will avoid being surrounded by it. In an oil slick, the hydrophobic tails mix with the oil, while the heads stay close to the water. In turbulence, phospholipids form two kinds of bubbles: a monolayer that can only capture a drop of oil and a bilayer that can capture a drop of water. The bilayer allows the hydrophobic tails to associate with themselves, while the heads associate with water on both the inside and outside surfaces of the bubble.
During the single-celled period of life on Earth, which spanned more than a billion years, the only downside to this arrangement was the necessity of finding, or synthesizing, enough phosphorous, lipid, and cholesterol for repairs, or to make new membranes when the cells divided. But then, about two billion years ago, multicel-lular creatures began to appear, and many of them, like birds and mammals, came to depend on an aqueous circulatory system to supply the various tissues and organs with nutrients. Since all of the cells in an animal’s body require cholesterol and lipids (or fats) for their membranes, these materials had to be shipped to them by way of the circulatory system. Cholesterol and fats are not water soluble, so animals had to devise a special system in order to transport these compounds in the blood. The system they developed came in the form of two particles: LDL (mentioned above) and high-density lipoprotein (HDL), both of which can be transported in an aqueous environment.
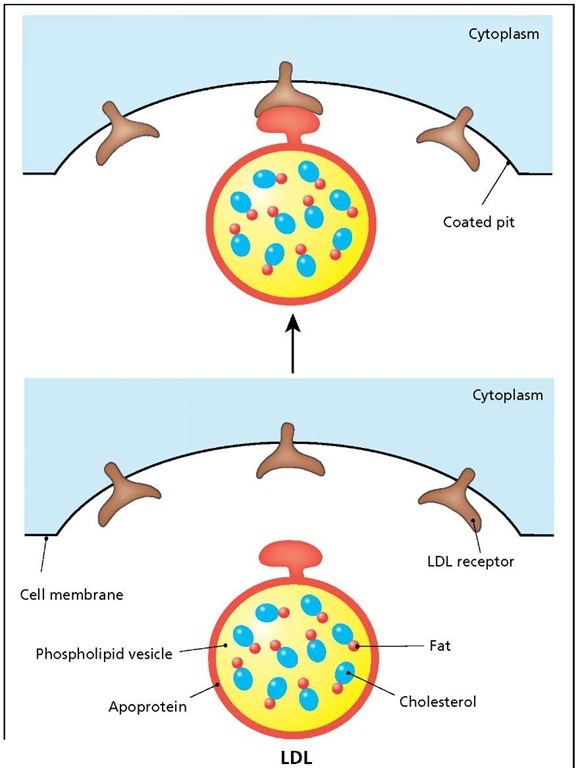
In mammals, lipids and cholesterol are absorbed by the cells in the gut and sent to the liver as large lipoprotein complexes. The liver processes these complexes to produce LDL and HDL, which are then released into the blood. LDL is the main source of fats and cholesterol for all of the tissues in the body. This particle is essentially a monolayer phospholipid bubble containing cholesterol and fat (the two are linked together by a chemical bond). The vesicle is stabilized by apoprotein, which contains a recognition site for the LDL receptor. All cells have LDL receptors, located in special regions of the cell membrane known as coated-pits. The binding of LDL to the receptor activates endocytosis, a process by which the cell ingests and utilizes the LDL. HDL has a structure similar to that of LDL, but it is a smaller vesicle with a higher concentration of fat and cholesterol. HDL’s main job is that of a cholesterol regulator; it collects excess cholesterol, secreted by the cells, and transports it back to the liver.
Structure and transport of low-density lipoprotein (LDL). LDL is a phospholipid vesicle (bubble) that transports cholesterol (combined with fat) from the liver to all the cells of the body. The vesicle is encased in apoprotein, which contains a recognition site for the LDL receptor. Binding of the apoprotein to the LDL receptor triggers the ingestion of the vesicle contents by a process known as receptor-mediated endocytosis.
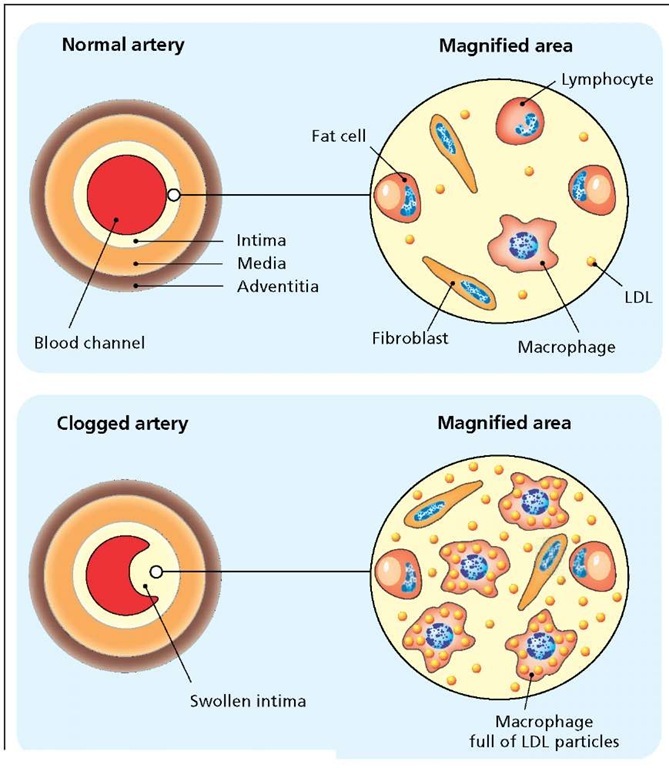
Normal and clogged coronary arteries. A normal coronary artery (shown in cross section) is a tri-layered tube consisting of the adventitia, media, and intima. The intima, covered in a thin layer of endothelium on the blood channel side, is a connective tissue consisting of fibroblasts, fat cells, and cells of the immune system (macrophages and lymphocytes). Excess LDL is taken up by the endothelium and collects in the intima. Oxidation of the LDL triggers an immune response that draws great numbers of macrophages and other immune cells into the area. Subsequent inflammation and faulty repair of the area leads to the formation of a swollen intima (plaque) that partially or completely blocks the artery.
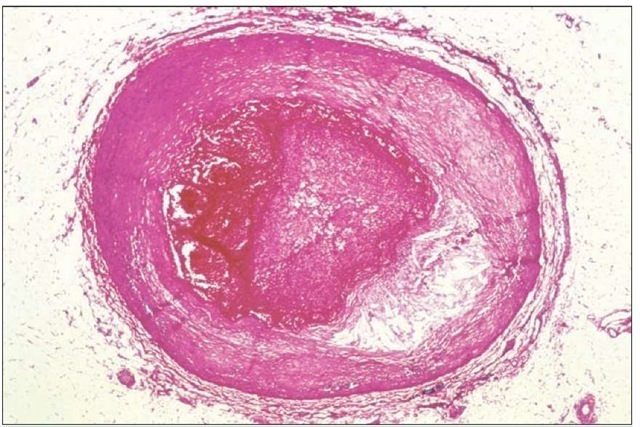
Degeneration of the arterial wall and narrowing of the lumen in the coronary artery. The artery is almost completely clogged in this image.
This system worked well for humans until the advent of the modern lifestyle, characterized by high-fat diets and lack of exercise. When plasma levels of LDL are low (less than 60 mg per 100 ml of blood), all of the circulating LDL is taken up by cells and utilized. But when the plasma levels exceed 60 mg per ml, LDL tends to collect in the intima, or innermost lining of the coronary arteries. An unfortunate property of fats is that they tend to oxidize, or go rancid, just like butter left out on the counter for too long a time. The oxidation of the LDL fat is interpreted by the immune system as an attack by a foreign body.
White blood cells, macrophages in particular, converge on the coronary plaque and begin ingesting as much of the LDL as they can, so much so that under the microscope the interior of these cells look as though they are full of a yellow foam. In the meantime, other white blood cells such as T lymphocytes release a variety of signaling molecules to coordinate the immune attack. The immediate response of this attack is the initiation of inflammation: The plaque and surrounding tissue becomes hot, red, and swollen, just like a cut finger or any other wound on the skin or in the body. Cells located at the intima-media boundary respond to the inflammation by migrating up to the top of the plaque in a misguided attempt to "heal" the wound. This cap of cells isolates the plaque from the circulatory system, but it increases the overall size of the deposit, thus obstructing the artery even more. But the plaque rarely grows large enough to completely block the artery; pathologists have shown that of all the fatal heart attacks so far studied only 15 percent were caused by such a plaque. The remaining 85 percent were caused when the plaque ruptures, which leads to the formation of a large blood clot that completely blocks the artery.
Many treatments are available for cardiovascular disease, including surgical intervention, angioplasty, pharmaceuticals, diet, and exercise. The last three therapies are aimed at reducing plasma levels of LDL and promoting an increase in the amount of HDL. Plasma levels of LDL can be decreased with low-fat diets, regular exercise, and by not smoking cigarettes. Drugs, such as lovastatin, block the synthesis of cholesterol in the liver and have been used successfully to reduce plaque formation. Regular exercise and a glass of red wine a day are also known to increase plasma levels of HDL, which can reduce the rate of plaque formation substantially. But despite the success of these therapies, it is clear that while the onset of CVD is age-related it is mainly the result of lifestyle and not an inevitable consequence of age. A combination of adequate exercise and a healthy diet begun at an early age is the best treatment.