Drug-Related Pemphigus
Both pemphigus vulgaris and pemphigus foliaceus can be either induced or triggered (i.e., latent disease unmasked) by certain drugs. Pemphigus that continues after a patient stops using a drug is referred to as triggered, whereas lesions that clear soon after withdrawal are referred to as induced. Although drug-related pemphigus is uncommon, its possibility must be excluded in all patients with newly diagnosed disease. The clinical, histo-logic,10 and immunofluorescence abnormalities11 of drug-induced pemphigus are similar to those of the idiopathic variety. However, pemphigus caused by drugs containing a sulfhydryl radical (thiol drugs) is clinically distinct from pemphigus caused by nonthiol drugs. The presence or absence of a sulfhydryl radical appears to influence both the type of pemphigus that is expressed and the prognosis of the drug-induced condition. Thiol drugs are more likely to induce pemphigus foliaceus, which is more likely to regress spontaneously when the drug is discontinued [see 2:VI Cutaneous Adverse Drug Reactions]. Nonthiol drugs are more likely to trigger pemphigus vulgaris, which can persist even after the drug is stopped. The most commonly implicated agents are thiol drugs such as penicillamine and captopril. Other responsible drugs include sulfur-containing drugs such as penicillins and cephalosporins. These undergo metabolic changes to form thiol groups and are termed masked thiol drugs. Nonthiol drugs that contain an amide group (e.g., dipyrone and enalapril) can provoke a disease that is indistinguishable from spontaneously occurring pemphigus vulgaris.11
Endemic Pemphigus
Epidemiologic features of fogo selvagem in rural areas of Brazil suggest that the production of pathologic antibodies to desmoglein 1 is linked to exposure to one or more environmental antigens.
Paraneoplastic Mixed Bullous Disease
Paraneoplastic pemphigus is an autoimmune disease of the skin and oral mucosa that develops in patients with an underlying neoplasm. It is characterized by large, tense bullae. Unfortunately, standard treatments for autoimmune blistering diseases fail in most cases. Paraneoplastic pemphigus shares clinical features of both pemphigus and severe erythema multiforme.
Hailey-Hailey Disease
Familial benign chronic pemphigus, or Hailey-Hailey disease, is an autosomal dominant disorder marked by multiple vesicles on inflammatory bases in skin subject to friction or pressure, such as intertriginous areas. In addition to pharmacologic treatment (see below), therapy includes keeping involved areas dry and free of friction.
Histologic and immunologic findings
The diagnosis should always be confirmed by histopathologic examination and immunofluorescence studies.13 Biopsies for pemphigus and all other bullous diseases should be performed at the edge of a lesion, so as to include clinically uninvolved adjacent skin. Acantholysis (the separation of keratinocytes from each other) is the fundamental abnormality in all forms of pemphigus.
All forms of pemphigus are associated with circulating and tissue-fixed intercellular (IC) autoantibodies that react against cell-surface keratinocyte antigens. The detection of these antibodies is very helpful in establishing the diagnosis, because they rarely appear in other conditions. Circulating IC autoanti-bodies are detected by indirect immunofluorescence assays on serum, and tissue-fixed IC autoantibodies are detected by direct immunofluorescence on skin biopsies. In both cases, they cause a lacelike pattern of fluorescence within the epidermis. Low titers of IC autoantibodies may also be present in burns, fungal infections, and allergic drug reactions. Antibodies against ABO blood group antigens, which are present in approximately 5% of the normal population, are the most common cause of false positive tests for IC autoantibodies. Tissue-fixed IC au-toantibodies are present in lesions and adjacent normal skin in approximately 90% of patients with pemphigus and are more sensitive and specific for the diagnosis of pemphigus than are circulating IC autoantibodies. The most common au-toantibodies are IgG, but IgM and IgA (with or without C3) may also be deposited.
Treatment
Initial Therapy
Initial therapy is determined by the extent and rate of progression of lesions. Localized, slowly progressive disease can be treated with intralesional injections of corticosteroids (triamcin-olone acetonide, 10 to 20 mg/ml) or topical application of high-potency corticosteroids. New lesions that continue to appear in increasing numbers can be controlled in some cases with low-dose systemic corticosteroids (prednisone, 20 mg/day). Patients with extensive or rapidly progressive disease are treated with moderately high doses of corticosteroids (prednisone, 70 to 90 mg/day). This dose is rapidly escalated every 4 to 14 days in 50% increments until disease activity is controlled, as evidenced by an absence of new lesions and the disappearance of skin pain or itching. If the disease remains active despite high doses of cor-ticosteroids (e.g., 120 to 160 mg/day of prednisone), one of the following approaches should be considered for rapid control:
1. Plasmapheresis, normally performed three times a week for removal of 1 to 2 L of plasma per procedure.14
2. Intravenous immunoglobulin (IVIg), usually given at a dosage of 400 mg/kg/day for 5 days or in higher doses for 3 days.15 The procedure may need to be repeated every 2 to 3 weeks for several cycles. It is very expensive. The use of IVIg for the treatment of skin diseases has recently been re-viewed.16 With both IVIg and plasmapheresis it is important to concurrently administer an immunosuppressive agent such as cyclophosphamide or azathioprine to minimize rebound in the level of pemphigus antibodies,14 and it is also important to monitor the level of these antibodies to ensure that the patient is responding to treatment.
3. Pulse therapy with megadoses of intravenous methylpred-nisolone, given at a dosage of 1 g/day for 5 days.17
No comparative studies have yet evaluated the relative effectiveness of these procedures. On the basis of such limited experience, IVIg may be preferred because it has fewer side effects than the other procedures and is associated with a significantly higher response rate. Once disease activity is controlled, the patient is maintained on the type and dose of medications required to establish control until approximately 80% of lesions are healed. Therapy should not be tapered while new lesions are appearing.
Rituximab, an anti-CD20 chimeric monoclonal antibody, is approved for use in non-Hodgkin lymphoma. However, there is a case report of partial remission from recalcitrant, life-threatening pemphigus vulgaris after treatment with rituximab.18
Adjuvant Therapy
The role of adjuvants in the treatment of pemphigus remains controversial. Because of a lack of controlled studies, it is not known whether the potential benefits of adjuvants outweigh the additional toxicities.5 Indications for adjuvant therapy include the presence of relative contraindications to systemic cortico-steroids, development of serious corticosteroid side effects, and repeated flares of disease activity that make it undesirable to reduce corticosteroid doses.7 Because they require 4 to 6 weeks to become effective, adjuvants are not used to control active, rapidly progressive disease.
Adjuvant treatments for pemphigus include a variety of cytotoxic and immunosuppressive agents (e.g., cyclophosphamide, azathi-oprine, cyclosporine, methotrexate, and mycophenolate mofetil19); dapsone; anti-inflammatory agents (e.g., gold); antimalarials; and certain antibiotics (e.g., tetracycline and minocycline).
Bullous Pemphigoid
Pathogenesis
The immediate cause of bullous pemphigoid (BP) appears to be an autoantibody response to the 180 kd (BP180) and 230 kd (BP230) basement membrane zone antigens.20 Passive transfer of these antibodies into animals can cause lesions of the disease21; anti-BP180 autoantibodies have been found to be a poor prognostic factor in a study of 94 elderly patients.22
Clinical features
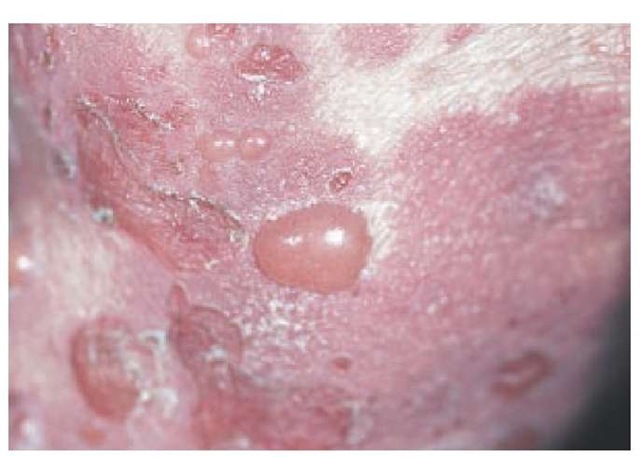
BP is a nonscarring, subepidermal blistering disease that is characterized by recurrent crops of large, tense blisters arising from urticarial bases. Lesions normally appear on the torso and flexures, particularly on the inner thighs. Blisters can range in size from a few millimeters to several centimeters [see Figure 3]. They are usually filled with a clear fluid, but they can be hemorrhagic.
Figure 3 Tense bullae characteristically occur in bullous pemphigoid.
Erosions are much less common than in pemphigus, and the Nikolsky sign is negative. A characteristic feature is that multiple bullae usually arise from large (palm-sized or larger), irregular, urticarial plaques. This is in contrast to the bullae of erythema multiforme (see below); in erythema multiforme, a single bulla arises from the center of a smaller (coin-sized) urticarial base.
In acute flares of BP, bullae may arise from normal-appearing skin. Oral lesions occur in 10% to 25% of patients; ocular involvement, however, is rare. Without treatment, the disease may become very extensive.
BP is a sporadic disease that occurs mainly in the elderly but can occur at any age and in any race. It has been reported in a 2-month-old infant.23 Precipitating factors include trauma, burns, ionizing radiation, ultraviolet light, and certain drugs. In a case-control study of 116 incident cases, neuroleptics and diuretics— particularly aldosterone antagonists—were more commonly used by patients who developed BP than by control subjects.24 There is still controversy as to whether BP is associated with an increased incidence of cancer25; however, correlations between flare in disease activity and recurrence of underlying cancer suggest such an association in individual patients.
BP is characterized by spontaneous remissions followed by flares in disease activity that can persist for years. Even without therapy, BP is often self-limited, resolving after a period of many months to years. The disease is nonetheless serious, particularly in older patients who have been treated with high doses of oral corticosteroids.26 Mortality is low in younger persons but is significant in the elderly. In one study of patients older than 68 years, nearly a third died of the disease or complications (mainly sepsis and cardiovascular disease) within 1 year.22
Histologic and immunologic findings
The earliest lesion of BP is a blister arising in the lamina luci-da, between the basal membrane of keratinocytes and the lamina densa. This is associated with loss of anchoring filaments and hemidesmosomes. Histologically, there is a superficial inflammatory cell infiltrate and a subepidermal blister without necrotic keratinocytes. The infiltrate consists of lymphocytes and histio-cytes and is particularly rich in eosinophils. There is no scarring.
Approximately 70% to 80% of patients with active BP have circulating antibodies to one or more basement membrane zone antigens. On direct immunofluorescence, the antibodies are deposited in a thin linear pattern; and on immune electron microscopy, they are present in the lamina lucida. By contrast, the antibodies to basement membrane zone antigens that are present in the skin of patients with systemic lupus erythemato-sus are deposited in a granular pattern.
Two less common subepidermal blistering diseases that are closely related to BP are cicatricial mucous membrane pem-phigoid and herpes gestationis [see Table 1 ]. The differential diagnosis also includes dermatitis herpetiformis and acquired epi-dermolysis bullosa (see below). Scar formation in mucous membrane pemphigoid and acquired epidemolysis bullosa can lead to major disability.27
Treatment
Treatment of BP is generally similar to that of pemphigus.28 The differences are as follows: (1) BP normally, but not invariably, responds to lower doses of systemic corticosteroids (alone or combined with other oral or topical agents), with most patients improving on prednisone at a dosage of 80 mg/day or less; (2) in an open prospective study of 18 cases, low-dose metho-trexate was shown to be effective for maintenance of clinical remission induced by initial short-term use of potent topical steroids29; and (3) BP is more likely to respond to dapsone30 or to the combination of tetracycline and niacinamide.31,32 Considering that the prognosis of untreated BP is better than that of pemphigus, side effects of treatment are of greater concern. Two small studies of severe ocular mucous membrane pem-phigoid suggest that this condition responds more favorably to treatment with cyclophosphamide combined with pred-nisone, whereas dapsone suppresses some cases of mild to moderate disease.27
Dermatitis Herpetiformis
Dermatitis herpetiformis (DH) is a rare vesiculobullous disease characterized by intensely pruritic, small vesicles that are grouped in small clusters and typically appear on the extensor aspects of the extremities and on the buttocks, scalp, and back.
Figure 4 Dermatitis herpetiformis, an extremely pruritic eruption, commonly presents as excoriated, grouped papulovesicles, often in a symmetrical distribution.
The condition is believed to be an immune-mediated disorder and is associated with abnormal granular deposits of IgA at the basement membrane zone and with asymptomatic, gluten-sensitive, spruelike enteropathy. The disease is chronic, with periods of exacerbation and remission. Lesions may clear if patients follow a strict gluten-free diet. Linear IgA dermatosis [see Table 1] is an uncommon subepidermal blistering disease that may clinically resemble DH or erythema multiforme (see below).
Pathogenesis
The cause of DH is unknown. It may be related to gluten-sensitive celiac disease; there is a strong association between the two conditions, and they share a similar genetic basis (both are associated with HLA-B8 and HLA-DR3). DH is thought to result from an abnormal IgA immune response to an unidentified antigen (possibly found in gluten) that contacts the gut. Skin lesions may result from deposition of immune complexes against this antigen in skin.
Clinical features
Skin lesions of DH are polymorphic. They usually begin as small, very pruritic urticarial papules or vesicles that are grouped in a herpetiform pattern [see Figure 4]. Actual vesicles or other primary lesions are rarely seen because they are excoriated by patients’ scratching. The distribution of lesions is characteristic: they occur most commonly on the elbows, knees, buttocks, scapular area, and scalp. Sometimes, lesions are scattered over the entire body. The lesions tend to appear suddenly and symmetrically, sometimes after ingestion of large amounts of gluten. Lesions heal, leaving hyperpigmentation; scarring may result from scratching or secondary infection. Involvement of mucous membranes is rare.
The disease is twice as common in men as in women. It predominantly affects persons between the ages of 20 and 50 years. There may be an associated patchy duodenal and jejunal atrophy that resembles the gluten-sensitive enteropathy of adult celi-ac disease.33,34 The enteropathy is usually asymptomatic and, like celiac disease, responds to gluten restriction. Because celiac disease is associated with gastrointestinal lymphoma, there is concern that the same may be true for DH. However, although lym-phomas of the small intestine have been reported in DH,35 the association appears to be rare.
Histologic and immunologic findings
Two characteristic laboratory features of DH are used for diagnosis. First, the disease is characterized histologically by accumulations of neutrophils and eosinophils in microabscesses at the tips of dermal papillae. In more severe cases, edema appears and can progress to subepidermal blisters appearing just below the lamina densa. Secondly, granular deposits of IgA are found at the basement membrane zone in almost all patients. These are often associated with granular deposits of C3 and, occasionally, of IgG and IgM. When found alone, IgA is one of the most sensitive and specific diagnostic markers for DH. When IgA is found with deposits of IgG, IgM, or C3, immune complex vasculitis and systemic lupus erythematosus are added to the differential diagnosis. Although basement membrane zone deposits of IgA alone also occur in linear IgA disease,36 the deposits in that condition are linear rather than granular. There are no circulating antibodies to normal skin components in DH.
Treatment
DH responds rapidly and dramatically to sulfones. Dapsone at a dosage of 100 to 200 mg/day is most commonly used for treatment. Glucose-6-phosphate dehydrogenase (G6PD) deficiency must be excluded before starting therapy, because lack of this enzyme can result in severe drug-induced anemia. Sul-fapyridine at a dosage of 1 to 3 g/day in divided doses (or sul-famethoxypyridazine) can be used in patients who cannot tolerate dapsone. Doses of these drugs are gradually reduced to the lowest amount that will suppress pruritus and development of new lesions. As indicated, patients also respond to a gluten-free diet; however, such diets are difficult to follow. Nevertheless, even a partial decrease in gluten intake will result in a decreased requirement for sulfones and should therefore be encouraged.
Erythema Multiforme
Erythema multiforme is an acute, recurrent, self-limiting disease that affects all age groups and races. It is characterized by the sudden eruption of crops of lesions, which represent a cell-mediated hypersensitivity reaction of the skin and mucous membranes to a variety of precipitating factors, including infectious agents and drugs [see Table 3].37 Recent or recurrent infection with herpes simplex virus is a principal risk factor for erythema multiforme.
![tmp4339_thumb[2] tmp4339_thumb[2]](http://what-when-how.com/wp-content/uploads/2012/04/tmp4339_thumb2_thumb.jpg)
