Treatment and Prevention
The choice of antibiotics depends on the organisms isolated from cultures of blood or abscess material. Until this information is available, the choice of drugs should be guided by the same principles as those that apply to the treatment of peritonitis. Although the use of antibiotics is essential, especially because of the risk of bacteremia, such therapy alone will not eradicate intra-abdominal abscesses and is therefore secondary to prompt, effective abscess drainage.
Until the mid-1970s, surgical drainage was mandatory for the treatment of intra-abdominal abscesses. However, treatment changed dramatically within just a few years of the introduction of percutaneous abscess drainage under ultrasonographic or CT guidance. Ultrasonography may be used to guide drainage of large or superficial collections, but CT is preferable for smaller or deeper abscesses.40 Many studies have demonstrated that percutaneous abscess drainage is safe and effective for a broad range of intra-abdominal collections; success rates range from 47% to 92%, with most studies reporting better than 80% success, similar to the success rate for surgical drainage.41 Failure of treatment is more common in immunosuppressed patients and in those with poorly defined phlegmons, multilocular abscesses, thick hematomas or organized infections, or abscesses with associated fistulous tracts.
Radiographic features alone cannot indicate which abscesses will respond to percutaneous drainage. Hence, it seems reasonable to institute percutaneous drainage in all patients who have a safe access route, provided that skilled personnel are available and that the patient does not otherwise require surgical intervention. Surgical drainage may then be used in patients with recurrences, failures, or complications. A surgeon should be involved in the decision regarding the method of drainage, because the surgeon will be called if the initial approach is not successful. Even in the case of abscesses that usually require surgical intervention.
A number of effective preventive strategies are available to reduce the likelihood of both wound infections (incisional surgical site infections) and intra-abdominal abscesses (organ/space surgical site infections) after abdominal operations.42 These include the appropriate use of prophylactic antibiotics,43 maintenance of normothermia in the operating room,44,45 provision of high levels of inspired oxygen,45,46 adequate fluid resuscitation during the operation,47 and maintenance of euglycemia in the perioperative period.48-50
Intraperitoneal abscesses
Intraperitoneal abscesses may form in either of two ways: (1) from diffuse peritonitis in which loculations of pus develop in anatomically dependent areas such as the pelvis, paracolic gutters, and subphrenic areas or (2) by spread of infection from a localized inflammatory process to contiguous peritoneum. About one third of intra-abdominal abscesses are intraperito-neal, and almost one half of intraperitoneal abscesses occur in the right lower quadrant.
Subphrenic Abscesses
About 60% of subphrenic abscesses develop after operations involving the duodenum and stomach, biliary tract, or topic; 20% to 40% develop after rupture of a hollow viscus.A variable percentage of subphrenic abscesses develop after penetrating or blunt (closed) abdominal trauma, and less than 5% develop without predisposing circumstances. Diagnosis of subphrenic abscesses is sometimes delayed because of their location in the intrathoracic portion of the peritoneal cavity, which is not amenable to examination.
Clinical features The manifestations of a subphrenic abscess range from a severe acute illness to an insidious chronic process characterized by intermittent fever, weight loss, anemia, and nonspecific symptoms. The chronic syndrome is most often observed in patients who have previously received antibiotics; in the past, such an abscess could smolder subclinically for prolonged periods before diagnosis. This is currently uncommon. In any patient with fever of undetermined origin who has had an abdominal operation—even if the operation was performed many months earlier—a chronic intra-abdominal abscess must be suspected and a CT scan should be done.
Spiking fever, abdominal pain and tenderness (most often at the lower costal margin), and weight loss are common manifestations. Features of an intrathoracic process, such as shoulder pain, chest pain, cough, dyspnea, rales, and pleural effusion, are more commonly observed than features of an intra-abdominal condition. Leukocytosis is common. Rarely, patients will have a prolonged, obscure febrile illness complicated by the sudden development of an empyema when the subphrenic abscess ruptures through the diaphragm. Although pleural fluid is present in about 80% of patients with a subphrenic abscess, it is usually a sympathetic transudate. A pleural effusion that develops after an abdominal operation is more commonly caused by inflammation below the diaphragm than inflammation above it.
Diagnosis CT scanning and ultrasonography are the best radiologic techniques for establishing the diagnosis. The plain x-ray findings in patients with subphrenic abscess include pleural effusion, limitation of diaphragmatic movement, elevation of a hemidiaphragm, and lower-lobe pneumonia or atelectasis.
Retroperitoneal abscesses
Pyogenic infections of the retroperitoneum present like other intra-abdominal infections. Indeed, many retroperitoneal abscesses arise from disorders of the abdominal viscera; more than two thirds of patients with retroperitoneal abscesses also have underlying debilitating conditions, including malignancies, corticosteroid use, alcoholism, and diabetes. More than 80% of these infections are polymicrobial, involving aerobic and anaerobic enteric organisms.51 CT scanning is the key to diagnosis of retroperitoneal abscesses. The same is true for primary psoas abscesses, which are often caused by S. aureus,52 and for perinephric abscesses, which usually originate in the urinary tract.53 As with other abscesses, successful management requires prompt percutaneous or surgical drainage and the administration of appropriate antibiotics.
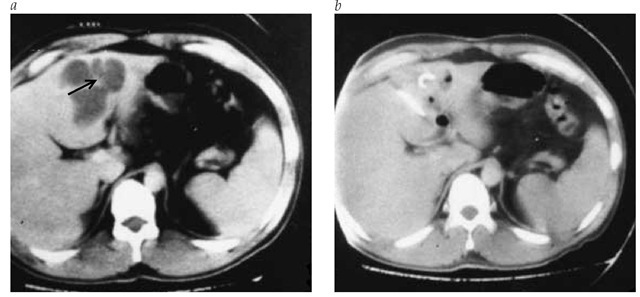
Figure 1 CT scan (a) shows multilobular liver abscess (arrow). Four days after percutaneous abscess drainage, CT scan (b) shows resolution of the abscess cavity.
Pancreatic Infections
Most pancreatic infections occur as a complication of pancreatitis, which can result from alcoholism (38%), gallstones (11%), surgical trauma (16%), or other factors (35%). Pancreatic infections have been divided into infected pancreatic and peripan-creatic necrosis and pancreatic abscesses.55 Infected pancreatic necrosis tends to occur during the first 3 weeks after the onset of acute necrotizing pancreatitis and is poorly localized within the retroperitoneum. Source control is difficult, and morbidity and mortality can be high. Infected necrosis often requires open operative debridement, although there are promising reports of combined percutaneous drainage and laparoscopically assisted debridement. Pancreatic abscess refers to a more localized infectious process. It can occur either in or adjacent to the pancreas and tends to occur more than 3 weeks after the acute onset of disease. An infected pseudocyst is also a pancreatic abscess. Pancreatic abscesses can often be managed percutaneously but are still likely to require additional source control.
Pancreatic infections are often polymicrobial, typically containing three or four species of bacteria. Most are enteric organisms, including E. coli, enterococci, Klebsiella species, and anaerobes such as Bacteroides, Peptococcus, Fusobacterium, and Clostrid-ium species. Nonenteric organisms, including staphylococci, P. aeruginosa, and, less often, Candida species, may be involved. Bacteremia occurs in about 26% of cases. Recent reports demonstrate a shift in the usual microbial flora of infected pancreatitis, with an increase in gram-positive cocci and fungi (e.g., Candida species), probably secondary to the increasingly common use of prophylactic antibiotics for long periods in patients with necro-tizing pancreatitis.
Clinical features The initial presentation of noninfected acute necrotizing pancreatitis involves fever, leukocytosis, and abdominal pain and tenderness. The clinical features do not al low the differentiation between infected and uninfected patients. Most infections occur after at least 1 week of disease.
Diagnosis The most accurate method for determining whether an area of pancreatic or peripancreatic necrosis is infected is to perform CT scan-guided fine-needle aspiration for Gram stain and culture. This step is indicated if a patient’s clinical condition deteriorates after initial stabilization or improvement.59
Treatment Source control is mandatory. It can often be accomplished by open surgical debridement, sometimes aided by percutaneous drainage, laparoscopic techniques, or both. The outcome is improved when intervention occurs later in the course of the disease. Antibiotic therapy is the same as for other intra-abdominal infections.
Visceral abscesses
Liver Abscesses
Epidemiology and etiology Pyogenic liver abscesses occur in several settings, including biliary tract infection, direct extension from a contiguous site of infection, portal bacteremia from intra-abdominal septic foci, and nonpenetrating trauma.60-62 Liver abscesses may occur as a result of systemic bacteremia or as complications of abdominal surgery or penetrating abdominal trauma. They may also occur as complications of hepatocellular carcinoma,63 chronic granulomatous disease,64,65 or percutaneous transhepatic biliary drainage procedures in patients with cancer and obstructive jaundice. Pyogenic abscesses may be single or multiple.
Like other intra-abdominal abscesses, pyogenic liver abscesses principally involve enteric bacteria; two thirds of these abscesses have polymicrobial origins, and at least one third involve anaerobes. S. aureus may be the causative organism in patients with bacteremia and in children. Klebsiella species are often responsible for gas-forming liver abscesses, which typically occur in patients with diabetes.66 Blood cultures are positive in about half of patients with a pyogenic liver abscess, and metastatic infections may occur.
Clinical features Fever is the most common symptom and is present in nearly 90% of patients. Chills and weight loss occur in about half of cases. Because abdominal pain, abdominal tenderness, or hepatomegaly is present in only half of cases, many of these patients present with fever of undetermined origin. Leukocytosis is present in most cases. Jaundice is infrequent, but the serum alkaline phosphatase level is elevated in almost all patients. Rupture of a liver abscess, although uncommon, is often accompanied by diffuse abdominal pain and septic shock.
Diagnosis CT scanning is the most accurate diagnostic technique [see Figure 1], yielding positive results in up to 95% of confirmed cases; ultrasonography is also helpful, yielding positive results in up to 80% of confirmed cases. The initial clue to the diagnosis may come from plain x-rays, which may show an elevated right hemidiaphragm, a right pleural effusion, or an air-fluid level.
The major differential diagnosis is amebic liver abscess [see 7:XXXIVProtozoan Infections]. Amebic abscesses are more likely to be solitary and confined to the right lobe of the liver; a history of travel or diarrhea may suggest the diagnosis. Stool ova and parasite examination revealing Entamoeba histolytica is highly suggestive, but results are often negative in patients with hepatic amebiasis. However, most patients with amebic liver abscesses have positive amebic serologies. It is important to note that E. histolytica has been reclassified into two morphologically similar but genetically distinct species: E. histolytica, the pathogenic protozoan that causes amebic dysentery and hepatic abscess, and E. dispar, a nonpathogenic commensal protozoan of humans. Specific enzyme-linked immunosorbent assay-based serologic testing to distinguish E. dispar colonization from E. histolytica infection is recommended before treating amebiasis.68,69 Less often, hepatic cysts or neoplasms may be confused with liver abscesses.
Treatment Whereas surgery was formerly the mainstay of therapy, percutaneous drainage should now be the initial drainage procedure in most patients with pyogenic liver abscesses. Antibiotics with broad coverage of enteric organisms and staphylococci should be administered intravenously until specific pathogens have been isolated from the abscess or the bloodstream.70 Mortality depends largely on the underlying disease and is highest in patients with cancer.71 Surgical therapy is required for ruptured abscesses, but the mortality is high, approaching 44%.67
Splenic Abscesses
Splenic abscesses are uncommon.Unlike other intra-ab-dominal abscesses, they are often bacteremic in origin, especially in patients with endocarditis. In other patients, hemoglo-binopathy, vasculitis with splenic infarction, trauma, and im-munosuppression may be predisposing factors. Fever and chills and left upper quadrant pain are common. If the upper pole of the spleen is affected, diaphragmatic and pleural and pulmonary symptoms may predominate, but peritoneal symptoms are more common if the lower pole is the site of infection. Responsible organisms include S. aureus, streptococci, Salmonella species, and enteric bacteria; fungi are important causes in immunocompromised patients. CT scans and ultrasonography are the most useful radiographic studies. Appropriate antimicrobial therapy is essential. Although splenectomy has often been required for effective management in the past, evidence now indicates that percutaneous drainage or even antibiotics alone may suffice in selected cases.73 More experience is needed before the optimal management of these uncommon infections can be determined.