Definition
Peptic ulcers are holes in the inner lining of the gastrointestinal (GI) tract that are attributed to exposure of the mucosa to gastric acid and pepsin. Peptic ulcers extend through the mu-cosa and the muscularis mucosae, a thin layer of smooth muscle separating the mucosa from the deeper submucosa, muscularis propria, and serosa. Most peptic ulcers are round or oval, but some are linear, triangular, or irregular in shape. Ulcers have depth when viewed through an endoscope. Typically, only a single ulcer is present. An erosion is a focal loss of superficial epithelial cells and glands, without extension through the muscu-laris mucosae. On endoscopy, erosions appear as breaks in the mucosal lining without depth. At the other extreme, a peptic ulcer may burr itself entirely through the wall of the GI tract, thus connecting the GI lumen with the peritoneal cavity (perforated ulcer), a solid organ such as the pancreas (penetrating ulcer), or another hollow organ such as the intestine or bile duct (fistuliz-ing ulcer).
Epidemiology
In the United States, peptic ulcer disease affects 10% of men and 4% of women at some time in their lives. The incidence is influenced by age (older persons are more susceptible than younger persons) and gender (males are more susceptible than females). Because ulcer disease is often recurrent, its prevalence exceeds its incidence. Eradication of Helicobacter pylori from the stomach markedly reduces recurrence of ulcer disease. With the widespread use of treatment regimens for H. pylori, the prevalence of peptic ulcer is decreasing in the United States. Reinfection with H. pylori remains an uncommon event in the United States (approximately one reinfection per 100 patients a year).
Pathogenesis and Etiologic Factors
The normal stomach and duodenum are able to resist autodi-gestion by acid-pepsin. However, high rates of acid-pepsin secretion or impaired mucosal resistance factors, such as prosta-glandin deficiency, can predispose to duodenal ulcer formation (typically in the most proximal part of the duodenum, the bulb) or to gastric ulcer formation (typically in the most distal part of the stomach, the antrum).
On rare occasions, peptic ulcers occur in the second, third, or fourth portion of the duodenum (postbulbar ulcer) or even in the proximal jejunum. Ordinarily, alkaline secretions from the duodenum, biliary tract, and pancreas neutralize gastric acid in the duodenum, but high rates of gastric acid secretion (e.g., in Zollinger-Ellison syndrome) can overwhelm these endogenous alkaline secretions and lead to postbulbar or jejunal ulcerations.
In patients with pathologic amounts of gastroesophageal reflux of acid-pepsin and in many patients with gastric acid hy-persecretion, erosions and ulcers may develop in the lower esophagus [see 4:I Esophageal Disorders]. Peptic ulcers may also occur where acid and pepsin are secreted heterotopically, such as in a congenital ileal (Meckel) diverticulum.
Regardless of location and etiology, chronic peptic ulcers are similar pathologically. In addition to the focal loss of mucosal epithelial cells, these ulcers have four characteristic layers at their base: fibrinoid necrosis, exudate, granulation tissue, and a fibrous scar, the deepest layer. A layer of granulation tissue and fibrosis may be absent in acute ulcers that occur in settings of serious trauma or severe surgical or medical illnesses [see Acute Stress Ulcers, below].
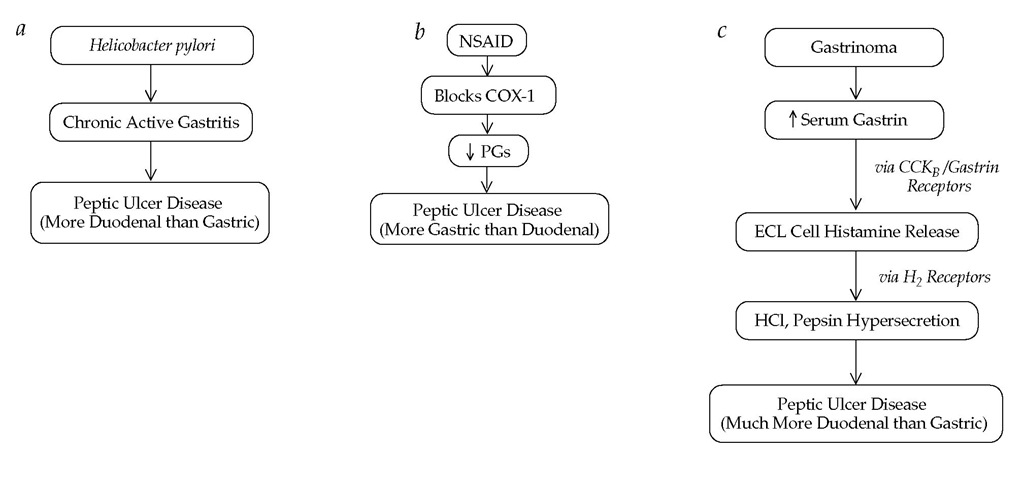
Why a peptic ulcer is such a focal lesion is unclear. Although peptic ulcers require the presence of acid-pepsin, acid-pepsin alone is only rarely sufficient to produce an ulcer—such as in Zollinger-Ellison syndrome, in which marked gastric hyper-secretion is present. In the majority of patients, there must be another predisposing factor, such as H. pylori infection of the stom-ach,1,2 use of nonsteroidal anti-inflammatory drugs (NSAIDs), or stress [see Figure 1].
H. PYLORI ulcers
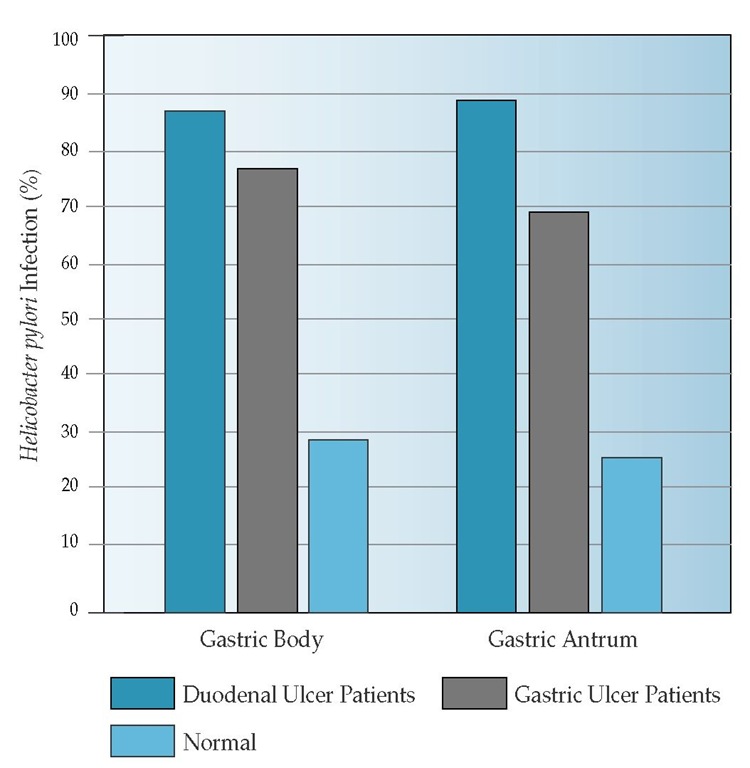
The prevalence of H. pylori infection of the stomach is much higher in duodenal ulcer patients and, to a somewhat lesser extent, in gastric ulcer patients than in age-matched control subjects [see Figure 2].3 In addition, cure of H. pylori infection with antimicrobial therapy markedly reduces recurrences of duodenal and gastric ulcers.4,5 The correlation of H. pylori infection with peptic ulcers is not consistent, however. Duodenal ulcers develop in some infected persons and gastric ulcers in others, but most infected persons experience no ulcers at all. Patients with duodenal ulcers tend more often to be infected with cagA-posi-tive strains than do H. pylori-infected patients without ulcer,6 but how this is mediated is not clear.
The etiologic mechanism linking H. pylori infection with ulcer development is not yet absolutely established, for the following reasons: (1) voluntary ingestion of H. pylori led to gastric H. pylori infection and to gastritis but not to ulcers; (2) duodenal or gastric ulcers develop in only 10% to 20% of individuals with H. pylori gastritis, implying that only certain persons with additional genetic, anatomic, physiologic, or environmental risk factors are predisposed to ulcers or that only certain H. pylori strains are ulcerogenic; (3) H. pylori induces diffuse inflammation in the stomach, yet the strongest link between H. pylori and peptic ulcer is with focal duodenal bulbar ulcer; and (4) gastric H. pylori infection is as common in women as in men, yet duodenal ulcer is two to three times less common in women. Currently, H. pylori can be considered the most important risk factor for duodenal and gastric ulcers, but it is clear that the mere presence of H. pylori in the stomach is not sufficient to cause peptic ulcers [see Figure 1a].
Nsaid ulcers
The ulcerogenicity of NSAIDs has been established experimentally by exposing animals, human volunteers, and patients to these drugs. Experimental studies have been corroborated by numerous case-control studies and autopsy studies. Unlike H. pylori-related peptic ulcers, which more often occur in the duodenal bulb, NSAID ulcers typically occur in the stomach. A gastric or duodenal ulcer associated with NSAID use is classified as a peptic ulcer, and it usually heals with potent acid antisecretory therapy, even if NSAID use is continued. NSAIDs can also cause ulcers in the jejunum, ileum, or colon, areas where there is little or no acid-pepsin. These ulcers are not actually peptic ulcers.
Figure 1 Etiopathogenesis of peptic ulcers. (a) Helicobacter pylori induces a diffuse, chronic, active superficial gastritis, usually throughout the stomach. Exactly how this infectious gastritis results in peptic ulcer disease is unknown. (b) Nonselective nonsteroidal anti-inflammatory drugs (NSAIDs) block cyclooxygenase-1 (COX-1) to reduce the amount of gastroduodenal prostaglandins (PGs) synthesized from their precursor, arachidonic acid. COX-2 selective NSAIDs produce a lesser reduction in prostaglandins and are associated with fewer peptic ulcers than nonselective COX-1-or COX-2-inhibiting NSAIDs. (c) Gastrinoma cells in the pancreas or duodenum secrete large amounts of gastrin into the circulation. Elevated serum gastrin levels promote the release of histamine by acting on receptors for cholecystokininB (CCKB) and for gastrin, which are located on gastric enterochromaffin-like (ECL) cells. Histamine acts on H2 receptors on parietal and chief cells to augment hydrochloric acid (HCl) and pepsin secretion.
Although the pathogenesis of NSAID ulcers is multifactorial, by far the most important mechanism appears to be inhibition of cyclooxygenase-1 (COX-1), the rate-limiting enzyme in GI prostaglandin synthesis [see Figure 1b]. Prostaglandins normally protect the GI mucosa from damage by maintaining mucosal blood flow and increasing mucosal secretion of mucus and bicarbonate. Blockade of COX-1 activity by NSAIDs reduces prostaglandin synthesis and thus lowers GI mucosal blood flow and secretion of mucus and bicarbonate. Evidence continues to accumulate that in NSAID users, H. pylori gastritis produces about a twofold increase in the risk of gastroduodenal ulcer for-mation.7 Moreover, clinically symptomatic peptic ulcers occur much less commonly if H. pylori gastritis is treated before the start of long-term NSAID therapy.8 Clinically diagnosed peptic ulcers will develop in approximately 2% to 4% of persons taking NSAIDs per year of exposure. The extent to which the damaging effects of NSAIDs on the stomach are topical rather than systemic is unclear. Many NSAIDs, such as aspirin, are acidic and thus nonionized in the acidic stomach, where they can be absorbed and initiate gastric mucosal damage. However, NSAIDs (e.g., ketorolac) given by parenteral injection and aspirin given transdermally are ulcerogenic, as are so-called NSAID prodrugs, such as sulindac and nabumetone (neither drug inhibits gastric prostaglandins until it is metabolized to its active form after GI absorption). Evidence suggests that acute mucosal damage by NSAIDs (i.e., hemorrhages and erosions, but seldom ulcers) is mainly caused by the topical damaging effects of NSAIDs. Chronic ulcer formation, often with complications such as bleeding and perforation, is mainly the result of the systemic effect of NSAIDs on prostaglandin synthesis by the GI mucosa.
Epidemiologic studies suggest that NSAIDs vary in their ability to cause ulcers,9 but this issue is complicated by the difficulty of comparing equipotent doses of NSAIDs. All prescription or over-the-counter NSAIDs should be considered ulcerogenic, with the risk of ulcer dependent on dosages and other patient-related factors, particularly advanced age and previous ulcer history. Even low doses of aspirin used for prophylaxis of cardiovascular disease (75 to 325 mg/day) are ulcerogenic.10 Neither buffering of aspirin nor enteric coating appears to reduce the incidence of clinically detected ulcer formation.11 Nonacety-lated salicylates such as salicylsalicylic acid (salsalate) do not block COX-1 and are not ulcerogenic. Epidemiologic studies indicate that the greatest risk of NSAID ulcers is early in the course of treatment (between day 7 and day 30 after initiation), with the risk decreasing thereafter.
Most NSAIDs, including aspirin, block both COX-1 and COX-2. Unlike COX-1, COX-2 is induced and expressed at inflammatory sites but not in the normal GI tract.12 Selective COX-2 inhibitors (coxibs) such as celecoxib and valdecoxib are analgesic and anti-inflammatory but seem to cause less GI ulcer formation than currently available cyclooxygenase inhibitors when used in recommended doses.13,14 Whether routine use of coxibs in place of nonselective NSAIDs will be cost-effective remains to be demonstrated.
Figure 2 Prevalence of H. pylori infection in either the gastric body or the gastric antrum, as assessed by endoscopic biopsy and mucosal histology. Normal control subjects were matched by age and sex to patients with duodenal ulcers and to patients with gastric ulcers. None of the ulcer patients were receiving aspirin or NSAIDs.
Corticosteroids, which block COX-2 but not COX-1,12 are not ulcerogenic when used alone, although they impair healing of preexisting ulcers. When corticosteroids are used in combination with NSAIDs, the risk of ulcer formation is much greater than when NSAIDs are used alone.
Ulcers in gastrinoma or other hypersecretory states
A gastrinoma is an endocrine tumor of the pancreas or duodenum (usually malignant) consisting of gastrin (G) cells. Gas-trinoma causes less than 1% of all peptic ulcers. Peptic ulcers develop in 95% of patients with gastrinoma (Zollinger-Ellison syndrome); ulcers occur most commonly in the duodenal bulb but are also seen in the postbulbar duodenum, jejunum, lower esophagus, and stomach. Multiple ulcers are present in up to 25% of cases of Zollinger-Ellison syndrome.
Patients with a gastrinoma have high circulating levels of gas-trin [see Figure 1c], which acts on receptors for cholecystokininB (CCKB) and gastrin located on enterochromaffin-like (ECL) cells within the mucosa of the gastric body. ECL cells then release his-tamine, which acts on H2 receptors present on the membrane of neighboring parietal cells to stimulate (via an adenylate cy-clase-cyclic adenosine monophosphate [cAMP]-mediated pathway) the secretion of hydrochloric acid by a unique proton pump, the H+,K+-ATPase pump. Of less physiologic importance, gastrin also acts directly on CCKB/gastrin receptors on parietal cells, increasing cytosol calcium levels in the parietal cells.
Hypergastrinemia in Zollinger-Ellison syndrome results in a continuous high rate of secretion of hydrochloric acid and pepsin, even under basal (fasting) conditions. These secretions overwhelm the buffering and neutralizing capacity of food and upper digestive secretions, as well as mucosal defense factors. Peptic ulceration results, and in many cases, diarrhea (with or without malabsorption) occurs.
Approximately 20% to 30% of patients with gastrinomas have features suggesting a multiple endocrine neoplasia type I (MEN I) syndrome, such as hypercalcemia secondary to hyper-parathyroidism, a pituitary adenoma, or both. MEN I is inherited as an autosomal dominant disorder.
Some patients with duodenal ulcer have marked acid hyper-secretion but normal serum gastrin levels. A few of these patients have hyperhistaminemia caused by systemic mastocytosis or chronic basophilic leukemia. However, the majority of patients have no known reason for the acid hypersecretion (idio-pathic basal acid hypersecretion), although some are infected with H. pylori. Eradication of H. pylori in these individuals may reduce basal acid hypersecretion.
Idiopathic ulcers
In the United States, up to 20% of cases of chronic gastric and duodenal ulcers occur in patients who have no evidence of H. pylori infection, deny taking NSAIDs, and have normal serum gastrin concentrations. These ulcers are referred to as idiopathic peptic ulcers. Some patients with this disorder may be taking NSAIDs surreptitiously or are unaware that they are taking these drugs. In others, emotional stress, perhaps associated with gastric acid hypersecretion, may be a contributing factor.15 Cigarette smoking is also a risk factor for peptic ulcers.
Acute stress ulcers
Acute gastroduodenal erosions and ulcers are very common in patients with serious medical and surgical conditions.16 Such conditions include severe head injury (Cushing ulcers); burn injury (Curling ulcers); major surgical procedures; and life-threatening illnesses such as septic shock, respiratory failure requiring mechanical ventilation, hepatic failure, renal failure, and multi-organ failure. Unlike peptic ulcers, stress ulcers are typically asymptomatic, rarely causing dyspepsia or epigastric pain. Approximately 10% to 25% of patients with acute stress ulcers experience painless upper GI bleeding of variable severity. Bleeding may manifest itself in the intensive care unit as a dark (so-called coffee-ground) or bloody nasogastric aspirate, as a declining hematocrit, as an increasing transfusion requirement, or as unexplained hypotension.
The pathogenesis of stress ulcers is not well understood. The common denominator seems to be tissue hypoxia and acidosis, precipitated by mucosal vasoconstriction and ischemia. Systemic hypoxia, metabolic acidosis, anemia, and reduced cardiac output often are contributing factors. Once mucosal hypoxia develops, mucosal defense factors are impaired and the cells lining the stomach and duodenum become vulnerable to damage by acid-pepsin. Acute stress ulcers have become less common because of the routine use of effective prophylactic medications in patients at high risk for this condition (see below).
Cameron ulcers
Linear gastric erosions that occur in a hiatus hernia are known as Cameron ulcers.16 The erosions are thought to be related either to traumatic injury of the stomach by the surrounding diaphragm or to mucosal ischemia at the point where the stomach herniates through the diaphragm. Like acute stress ulcers, Cameron ulcers tend to present as bleeding without dyspepsia. Both acute and chronic GI blood loss are possible outcomes of Cameron ulcers.
Diagnosis
Clinical manifestations
Peptic ulcers produce a variety of symptoms but none specific for the disease. Also, symptoms of duodenal ulcer are indistinguishable from those of gastric ulcer. Patients with uncomplicated ulcers typically experience mild to moderate abdominal pain, usually in the epigastrium. However, the pain may be localized to the left or right upper quadrant of the abdomen, to the lower chest (subxiphoid or substernal), the midabdomen, or the back. The pain is often gnawing or burning. It may occur in the middle of the night; rarely, it occurs upon first awakening in the morning. Discomfort is typically relieved by food or an antacid.
Severe pain or a rapid increase in pain suggests an ulcer complication (e.g., perforation or penetration) or another diagnosis (e.g., acute pancreatitis). Associated dyspeptic symptoms include nausea, bloating, heartburn, and belching. Although vomiting may occur with uncomplicated peptic ulcers and may temporarily relieve pain, repeated vomiting suggests an ulcer complication (e.g., gastric outlet obstruction) or another diagnosis (e.g., intestinal obstruction).
Peptic ulcers are the most common cause of acute upper GI bleeding. Therefore, hematemesis, melena, or both, even in a patient with no history of ulcer and no dyspeptic symptoms, should suggest the possibility of a bleeding peptic ulcer. Patients who develop ulcers while taking prescription or over-the-counter NSAIDs or low (cardiovascular) doses of aspirin often have no history of ulcerlike pain. Other patients with bleeding ulcers will have experienced dyspeptic symptoms for the preceding days or weeks, only to have these symptoms wane when bleeding ensues.
In addition to a review of the patient’s symptoms and ulcer risk factors (particularly NSAID use and smoking), a family history should be obtained. A family history of ulcer can usually be attributed to within-family infection by H. pylori, to NSAID use, or to smoking. However, a family history of ulcer, hyperpara-thyroidism, kidney stones, or endocrine tumor should alert the physician to the possibility of gastrinoma (Zollinger-Ellison syndrome), with or without autosomal dominant MEN I syndrome.
Physical examination findings
In uncomplicated peptic ulcer disease, the examination is generally normal. The presence of epigastric tenderness does not distinguish dyspepsia caused by peptic ulcer from other types of dyspepsia.
Patients who have complicated ulcers often have tachycardia and hypotension, which are exaggerated when the patient assumes an upright position. These findings may indicate a bleeding ulcer, a perforated ulcer with peritonitis, or an obstructing ulcer with protracted vomiting and volume depletion. Pulse and blood pressure measurements may give misleading information about the extent of volume contraction if the patient has preexisting hypertension, has cardiovascular disease, or is receiving medication that can affect these parameters (e.g., a beta-adrenergic blocker or a calcium channel blocker). Fever and tachypnea suggest ulcer perforation with peritonitis.
Special attention should be given to the patient’s mental status, skin and mucous membranes, heart and lungs, and, of course, abdomen and rectum. Involuntary guarding, rigidity, rebound tenderness, and a paucity or absence of bowel sounds suggests ulcer perforation with peritonitis. These findings may be less prominent or even absent in the very young, the elderly, and patients on corticosteroids or analgesics. Abdominal disten-tion suggests gastric outlet obstruction or ileus. In a patient who has not eaten in 6 hours, a splashing sound over the stomach when the body is shaken (succussion) suggests gastric outlet obstruction or delayed gastric emptying caused by ileus. Melena or a positive fecal occult blood test suggests ulcer bleeding. Hematochezia or maroon-colored stool may be present if bleeding is voluminous and intestinal transit is rapid. Detection of melena, hematochezia, or maroon-colored stool should prompt placement of a nasogastric tube to obtain an aspirate of gastric contents. If this aspirate is grossly bloody, the diagnosis of upper GI bleeding is confirmed and the likelihood of a bleeding ulcer is increased.
Laboratory studies
Laboratory results are normal in most patients with uncomplicated ulcer. A complete blood count should be done if blood loss or ulcer perforation is suspected; and serum electrolytes, blood urea nitrogen (BUN), and serum creatinine should be measured if the patient has poor oral intake, nausea, or vomiting. An elevated serum calcium level suggests the possibility of hyperparathyroidism and MEN I with Zollinger-Ellison syndrome, but the pretest probability of this condition is too low in patients presenting with ulcerlike symptoms to recommend routine measurement of serum calcium. If the patient has a strong family history of ulcer disease or of renal stones or has a personal history of renal stones, measurement of serum calcium is warranted, as is measurement of fasting serum gastrin once ulcer disease is confirmed and other causes of ulcer are excluded. If the calcium level is elevated, a serum parathyroid hormone measurement should be ordered.
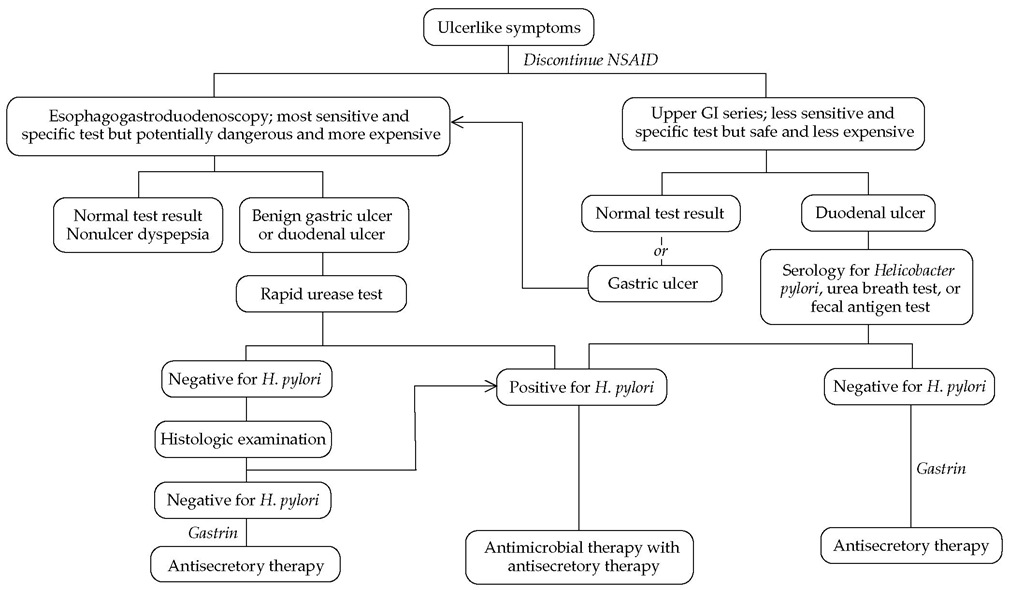
Figure 3 Approach to a patient with new and undiagnosed ulcerlike symptoms refractory to a trial of antisecretory therapy with an H2 receptor blocker or a proton pump inhibitor at customary doses or a patient with recurrent ulcerlike symptoms when the antisecretory therapy is stopped.
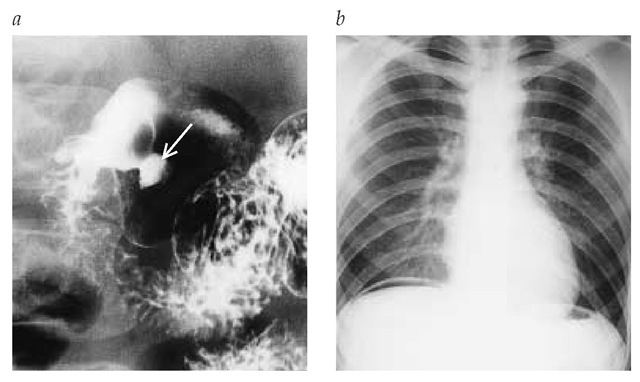
Figure 4 (a) Upper GI series in which double contrast (barium and air) is used, showing rounded collection of barium in an ulcer (arrow) in the duodenal bulb of a patient presenting with dyspepsia (uncomplicated duodenal ulcer). (b) Upright chest x-ray showing air beneath the right hemidiaphragm (pneumoperitoneum) of a patient presenting with an acute abdomen caused by a perforated duodenal ulcer.
Patients with complicated ulcers often have significant laboratory abnormalities, but these abnormalities are not specific for ulcer disease. Patients with bleeding ulcers have anemia and may have leukocytosis. The red cell indices (e.g., mean corpuscular volume) are typically normal. In the first several hours after an acute ulcer bleed, the hemoglobin concentration will not completely reflect the severity of the blood loss until compensatory hemodilution occurs or until intravenous fluids such as isotonic saline are administered. Thus, the pulse rate and blood pressure in the supine and upright positions are better initial indicators of extent of blood loss than are red cell counts. Patients with bleeding ulcers typically have azotemia, with ratios of BUN to serum creatinine concentrations exceeding 20:1, resulting from digestion and intestinal absorption of nitrogenous blood components in concert with reduced renal perfusion.
In patients with perforated ulcers and peritonitis, exudation of plasma into the peritoneal cavity (so-called third space) may result in an increased hemoglobin concentration from hemocon-centration. The presence of leukocytosis, elevated band forms, or leukopenia should raise suspicion of intra-abdominal sepsis. Lactic acidosis with an increased anion gap may ensue as a consequence of a sepsis syndrome or hypovolemia.
Patients with gastric outlet obstruction typically exhibit a hy-pokalemic, hypochloremic metabolic alkalosis. If volume loss is extreme, a coexistent metabolic lactic acidosis with an increased anion gap may be present, which may cause an elevated serum bicarbonate level to drop toward normal or even to low levels. Likewise, mild to moderate hyponatremia often develops in patients with vomiting from gastric outlet obstruction. Prerenal azotemia and a BUN-serum creatinine ratio greater than 20:1 are typical.