Cardiac Abnormalities
Clinically significant involvement of heart muscle is unusual and is probably associated with a poor prognosis. Cardiac abnormalities may take many forms, ranging from rhythm or conduction disturbances to myocardial inflammation or fibro-sis. Cardiac muscle abnormalities may be detected by radionu-clide scanning studies. However, many histologic and electrical abnormalities are not clinically significant.31 Therefore, evaluation beyond routine diagnostic studies is rarely indicated.
Calcinosis
Soft tissue calcification is seen most commonly in children. Deposits may be deep along fascial planes or in superficial dermal areas, sometimes with ulceration through the skin. Treatments have been based on largely anecdotal reports; no systematic studies have been carried out.32 Agents that have been found to be of use in some cases include probenecid, diltiazem, and warfarin. Some patients show spontaneous regression of calcinosis without specific treatment.
Vascular Abnormalities
Raynaud phenomenon is most commonly observed in patients whose myositis is associated with another rheumatic disease (e.g., scleroderma). Clinically significant vasculitis is unusual in adults, although dermatomyositis patients may show vascular changes on histologic examination.
Laboratory tests
Muscle Biopsy
Histologic confirmation of muscle inflammation is required in many, but not all, cases of inflammatory muscle disease. Patients with the characteristic skin rash of dermatomyositis and with elevated serum muscle enzyme levels may be treated without a muscle biopsy, because these two indicators can be used to follow the course of disease. In the absence of a skin rash or elevations in muscle enzyme levels, diagnosis is more difficult; in most patients, a biopsy is needed to confirm the presence of muscle inflammation. Two types of biopsy approaches are used: open surgical and closed needle. The closed-needle approach offers the advantages of decreased morbidity and of lower cost because an operating room is not required. Tissue samples obtained with the closed-needle approach can provide sufficient diagnostic information for interpretation by the muscle pathologist. However, the quality of the specimen obtained is dependent on the skill and experience of the operator. In the absence of such a resource or in special cases in which it is desirable to obtain extra tissue, the open surgical approach is preferable. Imaging studies such as MRI or CT can be used to determine the optimal site for biopsy.
All biopsy specimens require immediate handling by an experienced surgical team working closely with the pathology laboratory to ensure optimal results. Light microscopic analysis is sufficiently informative for most purposes. Because the treatment of polymyositis and that of dermatomyositis are the same, immunophenotyping of cellular infiltrates to distinguish between these two disorders is not indicated for routine diagnostic specimens. Electron microscopy may be required to demonstrate the inclusion bodies that define IBM. Examination of the biopsy specimen by a specialist in neuromuscular pathology may be helpful, because many pathologists do not see these diseases on a regular basis.
Muscle Enzymes
Most patients with inflammatory myopathy have increased muscle enzyme levels at some point during the course of active myositis.33 The presence of intracellular muscle enzymes in the serum most likely reflects damage to muscle cell membranes. The most commonly used muscle enzyme measurement is the creatine kinase (CK) level. The CK level may rise to many times normal. The MB isozyme of CK may be elevated because of the presence of this isoform in regenerating skeletal muscle. Measurement of CK may be confounded by the presence of naturally occurring inhibitors of this enzyme. Furthermore, racial and gender variations exist for normal levels of CK, with black males generally showing the highest values.34 Aldolase is another muscle enzyme that may be measured in the serum and may have less variability. However, aldolase is present in tissues other than muscle, and therefore, it is not specific for muscle damage. MRI studies have shown that active muscle inflammation may exist in patients with persistently normal CK serum levels.35 Reasons for this discordance are not known, but the findings suggest that treatment strategies should be focused on the clinical status of the patient rather than on the muscle enzyme levels.36
Autoantibodies
Autoantibodies to nuclear and cytoplasmic antigens are found in as many as 90% of patients with an inflammatory my-opathy. These antibodies are often useful in differentiating inflammatory myopathies from diseases that are not autoimmune disorders. Some of these autoantibodies are nonspecific and are seen in several autoimmune disorders. Other autoantibodies are relatively specific for the inflammatory myositis syndromes in general or for specific diagnostic categories. About 25% of patients with inflammatory myositis test positive for antinuclear antibody; in patients with overlapping rheumatic disease syndromes, the percentage is higher. The antinuclear antibody test is generally not helpful in establishing a diagnosis of myositis or one of its subsets. Autoantibodies that are in large part directed against cytoplasmic ribonucleoproteins have been designated as myositis-specific autoantibodies (MSA). Approximately 30% of patients with myositis have one or more of these autoanti-bodies. They are thus relatively specific but not sensitive to the presence of myositis, and as such, these autoantibodies cannot be used to screen for the presence of disease.
Three groups of patients can be defined by the MSA specificities. These subgroups differ in clinical presentation and prognosis.37 The first group is defined by the presence of antibodies directed against aminoacyl-tRNA synthetases. The presentation in the first group is generally characterized by an acute onset of muscle disease, with a high incidence of associated interstitial lung disease. Patients in this group may also have arthritis and a hyperkeratotic rash on the hands, known as mechanic’s hands. A majority of patients in this group test positive for HLA-DR3. Responses to treatment are variable, and mortality is significant. The second group includes patients with antibodies to the signal recognition particle (SRP). This protein complex facilitates translocation of newly synthesized polypeptides across the endoplasmic reticulum. Patients with anti-SRP have an abrupt onset of muscle weakness and may have associated involvement of cardiac muscle. The majority of patients in this group are African-American women. Responses to treatment are not good, and the prognosis is poor. In one series, the 5-year mortality for anti-SRP patients was 75%. A third group is identified by antibodies to Mi-2, which is a nuclear protein with unknown function. The majority of these patients have the dermatomyositis clinical syndrome with the so- called shawl-sign pattern of rash on the trunk and with cuticu-lar overgrowth. Responses to treatment are generally good, and mortality is lower than that in the other groups. Most of these clinical associations, which were originally described in North American patients, have been confirmed in a large group of European patients.38 Preliminary reports suggest that antibodies to a novel 155 kd protein may also be useful in identifying patients with amyopathic dermatomyositis.39
Electromyography
In most patients, electromyography reveals low-amplitude, polyphasic motor unit potentials, indicating a lack of synchronous contracture in muscle fibers within motor units. This finding correlates with the usually inhomogeneous distribution of muscle degeneration shown by histopathologic examination. Fibrillations and insertional irritability are evidence of membrane abnormalities. These findings are characteristic of, but not specific for, myositis.
Imaging and spectroscopy techniques
Conventional radiographs have little value in evaluating skeletal muscle. However, other techniques, including ultra-sonography, CT, and MRI, can enhance diagnostic approaches to many myopathies.40 Of these modalities, MRI has been the most useful in the evaluation and longitudinal management of inflammatory muscle syndromes. However, it may not be the method of choice in all circumstances, and in some of these cases, the alternative modalities of ultrasonography and CT can provide helpful information. Advantages of these three techniques are that they are noninvasive and offer the possibility of examining a volume of muscle larger than that which can be obtained by biopsy. In patients for whom biopsy may be a difficult or traumatic experience, such as young children, imaging may provide sufficient information to proceed with treatment.
Magnetic Resonance Imaging
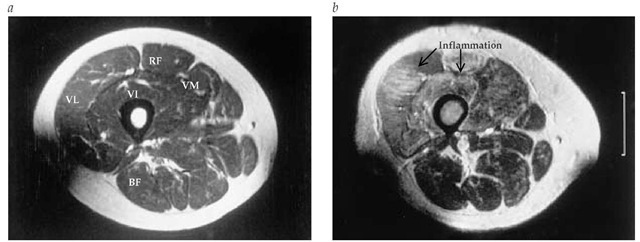
MRI is a very accurate method for muscle imaging that has been very useful in the diagnosis and management of patients with inflammatory muscle diseases of many kinds. Full assessment requires both T1- and T2-weighted images. The T1 image is most useful for outlining muscle anatomy because it detects changes in muscle mass caused by atrophy or fat infiltration. Inflammation is readily detected on the T2-weighted image, where the abnormal areas appear as brightness against the usually dark background of normal muscle [see Figure 3]. Studies using MRI have clearly demonstrated the patchy nature of the muscle inflammation, perhaps explaining why some patients with significant weakness have normal biopsy results. In dermatomyositis, inflammation in the thigh muscles is seen in predominantly anterior muscle compartments, and muscle mass is generally preserved. In patients with polymyositis and inclusion body myositis, extensive fat infiltration and muscle atrophy, which can include all muscle groups, are more likely to be seen. Longitudinal MRI studies can be used to document the effectiveness of immunosuppressive therapy. Patients may be studied in the usual body coil, which allows for visualization of both legs.41 Other studies have utilized a knee coil positioned over the anterior quadriceps, which provides a greater level of detail.35 As in all MRI studies, patients must be very carefully questioned for the presence of any indwelling metals before being placed in the magnet.
Ultrasonography
Ultrasonography is a readily available and relatively inexpensive technique that has been used to examine a wide variety of muscle disorders.42,43 Inflammation within muscle tissues appears on ultrasonography as areas of decreased echogenici-ty. In addition, blood-flow changes can be measured with related techniques such as color Doppler imaging. Ultrasonography may be useful in guiding the choice of site for needle or open muscle biopsy.
Computed Tomography
CT is not useful for the detection of inflammatory muscle changes. However, areas of atrophy or fat infiltration cause decreased muscle density, which is easily detected by CT. Soft tissue calcifications such as those seen in juvenile dermatomyosi-tis are best visualized with CT. Sometimes, these calcifications are in deep areas that cannot be readily appreciated on physical examination.
Figure 3 Magnetic resonance images of thigh muscles in a patient with dermatomyositis. The ^-weighted image (a) shows uniform density in all muscle groups, identified as VL, vastus lateralis; VI, vastus intermedius; VM, vastus medialis; RF, rectus femoris; and BF, biceps femoris. The T2-weighted image (b) illustrates inflammation in muscles of the quadriceps group, shown as areas of brightness or increased signal intensity.
Magnetic Resonance Spectroscopy
Spectroscopy is primarily a research tool. However, studies have shown the utility of this noninvasive approach for evaluating muscle function, and applications in the clinic may become available in the near future.35,44 In patients with dermato-myositis, loss of high-energy phosphate compounds needed for efficient muscle contraction has been documented with P-31 magnetic resonance spectroscopy.44 Longitudinal studies have documented that correction of these metabolic abnormalities may lag behind improvement in muscle inflammation.
Evaluation for underlying malignancy
Patients with dermatomyositis and polymyositis are at increased risk for an underlying malignancy. The magnitude of this risk is difficult to determine and varies greatly between reports. One study in a population-based cohort estimated the relative risk of cancer as 1.8 in males and 1.7 in females.45 A more recent study from Scotland has indicated that the relative risk may be as high as 7.7 in patients with dermatomyositis, with a greater risk in females than in males.46 In general, the risk is greater in patients with dermatomyositis than in patients with polymyositis and in all patients who are older than 40 years. There is general agreement that routine screening for malignancies should include chest radiography, mammogra-phy (in women), examination of stool for occult blood, complete gynecologic examination, and assessment for prostate-specific antigen (in men). Abnormalities seen on these screening tests may suggest the need for additional studies such as endoscopy, colonoscopy, and tissue biopsy. The most difficult malignancies to detect are those arising in the ovary. Uterine transvaginal ultrasonography or CT of the pelvis should be done in women older than 40 years, but some occult ovarian malignancies escape detection even with these tests. Some investigators advocate lower gastrointestinal studies to detect colon cancer in patients older than 65 years.12 Other, more extensive screening tests for occult malignancies are generally not recommended.
Differential Diagnosis
Diagnosis of dermatomyositis is aided by the presence of the characteristic rash. However, because the rash has features of SLE, this diagnosis may be confused with SLE, especially when the antinuclear antibody test is positive. Patients with poly-myositis may be difficult to distinguish from patients with other myopathic disorders [see Table 2]. These other disorders include metabolic myopathies, endocrine dysfunction, drug-induced disorders, infections, and miscellaneous syndromes such as sar-coidosis. Some types of dystrophies should also be considered in patients who have muscle weakness and elevated muscle enzyme levels. Myalgia syndromes, such as polymyalgia rheu-matica, in which stiffness is a predominant complaint, may confuse the diagnosis in some patients. Fibromyalgia, which is associated with a primary symptom of fatigue rather than muscle weakness, is characterized by the presence of discrete tender points that are not usually present in myositis patients.
Treatment
Guidelines for treatment of the idiopathic inflammatory my-opathies are not well established for several reasons. The diseases are uncommon, making it difficult to accumulate sufficient numbers of patients to carry out randomized, controlled trials. In addition, some forms of these diseases have a slow, prolonged course, requiring long periods of observation. Finally, there is as yet no uniformly accepted classification scheme for these disorders; thus, comparisons of therapies administered to different groups of patients at different times and places may not be valid. As examples, in the past, polymyositis and dermatomyositis have been included in the same category, and IBM may not have been recognized. It is now clear that different forms of these diseases vary in prognosis and in response to therapy.
Table 2 Differential Diagnosis of Inflammatory Myositis
|
Cause |
Effect |
|
Metabolic myopathies |
Myophosphorylase deficiency (McArdle disease) |
|
Myoadenylate deaminase deficiency |
|
|
Carnitine palmitoyltransferase deficiency |
|
|
Glycogen storage disease |
|
|
Periodic paralysis |
|
|
Hypokalemia, hypomagnesemia |
|
|
Endocrine disorders |
Cushing syndrome |
|
Thyroid dysfunction |
|
|
Drug-induced disorders |
Ethanol toxicity |
|
Penicillamine toxicity |
|
|
Lipid-lowering drug (statin) toxicity |
|
|
Zidovudine toxicity |
|
|
Infections |
Viral: HIV, coxsackievirus, adenovirus, influenza virus, echovirus |
|
Other rheumatic disorders |
Systemic lupus erythematosus (rash) |
|
Polymyalgia rheumatica |
|
|
Miscellaneous disorders |
Sarcoidosis, eosinophilia |
Drug therapy
A table showing drugs for the treatment of inflammatory muscle diseases is provided [see Table 3].
Glucocorticoids
Corticosteroids are the mainstay of initial therapy. Most patients with documented muscle inflammation should be started on these drugs at relatively high levels (1 mg/kg/day), given in divided doses. A standard approach has been to maintain this dosage for up to 3 months or until clinical improvement occurs. After this initial period of high-dose therapy, the dose can be consolidated into a single morning dose and then tapered, with the total daily dose being reduced by 20% to 25% each month and a maintenance dose of 5 to 10 mg daily being achieved in about 6 to 8 months. The addition of second-line drugs to the prednisone regimen is now recommended within 3 months after initiation of treatment. Older patients with co-morbid conditions such as diabetes and osteoporosis are especially at risk from side effects of steroids. Side effects may include a cushingoid appearance, compression fractures, avascu-lar necrosis, cataracts, and infections. One study has suggested that the side effects of corticosteroid therapy contribute significantly to the morbidity of polymyositis and dermatomyositis.47 For these reasons, any patient with severe muscle weakness, limited functional status, or underlying conditions that make steroids a high risk (e.g., diabetes mellitus or osteoporosis) should be started on second-line immunosuppressive drugs at the outset.
Table 3 Drugs for the Treatment of Inflammatory Muscle Diseases
|
Drug |
Dose |
Efficacy Rating |
Comments |
|
Prednisone |
5-60 mg/day |
Highly effective for initial treatment |
Side effect: cushingoid syndrome Avoid prolonged use at high doses; taper to 10 mg/day or less |
|
Methotrexate |
15-25 mg/wk |
Effective, steroid-sparing |
Side effects: liver abnormalities, pneumonitis Supplement with folate |
|
Azathioprine |
100-150 mg/day |
Effective, steroid-sparing |
Side effect: bone marrow suppression Can be combined with methotrexate |
|
Hydroxychloroquine |
200 mg b.i.d. |
Effective for skin manifestations |
Side effect: retinal toxicity Can be combined with other agents |
|
Cyclophosphamide |
100-150 mg daily or as intravenous pulses every 6 wk |
Possibly effective for lung involvement |
Side effects: bone marrow suppression, hemorrhagic cystitis |
|
Cyclosporine |
3 mg/kg/day |
Use after other immuno-suppressants |
Side effects: hypertension, renal dysfunction |
|
Intravenous immunoglobulin |
1 g/kg/day, 2 consecutive days monthly |
Use in patients in whom other regimens have failed |
High cost and limited supply |
Methotrexate and Azathioprine
The most commonly used second-line agents for the treatment of inflammatory myopathy are methotrexate and aza-thioprine. Methotrexate may be given orally or subcutaneously at an initial dosage of 7.5 to 10 mg weekly and then increased gradually to 25 mg weekly. As the dosage of methotrexate is increased, the dosage of prednisone is usually tapered. In general, methotrexate is well tolerated by patients with inflammatory myopathy, but there have been reports of toxicities similar to those seen in patients with rheumatoid arthritis who have taken methotrexate. Regular monitoring of liver function is necessary. Measurement of enzymes other than aminotrans-ferases is required to prevent interference by the ongoing muscle inflammation. y-Glutamyltranspeptidase is a liver-specific alternative. Methotrexate may be useful in the treatment of interstitial lung disease associated with myositis, but because this drug may in rare cases cause pulmonary toxicity, it is relatively contraindicated in patients with significant lung problems.
Azathioprine has been shown to be effective in patients with myositis in a prospective, controlled, double-blind trial, but treatment for at least 6 months may be required for improvement to occur. Azathioprine therapy should be initiated at a dosage of 50 to 100 mg/day, and the dosage should be increased gradually to a maximum of 150 to 200 mg/day. Side effects include bone marrow suppression and development of infections and, possibly, malignancies. Azathioprine and methotrexate have similar efficacy in these disorders, and the choice of which to use may depend on tolerability or comorbid conditions. Patients with myositis in whom therapy with glucocorticoids and either methotrexate or azathioprine has failed may respond to a combination of methotrexate and azathioprine.48,49
Other Immunosuppressive Agents
Cyclophosphamide has been given both as intravenous pulse therapy and by daily oral administration. Some data suggest that it may be useful in adults with the antisynthetase syndrome and in children with vasculitis-related complications of der-matomyositis. Cyclophosphamide may be useful in the treatment of the complication of interstitial lung disease.30 Other drugs that may be of value in patients in whom other therapies have failed include cyclosporine, FK506 (tacrolimus), chlorambucil, and mycophenolate mofetil.50-52 The adenine analogue fludarabine has also shown some benefit in one study of refractory patients.53
Intravenous Immune Globulin
Intravenous immune globulin appears to benefit some patients with either polymyositis or dermatomyositis. A controlled trial of immune globulin in dermatomyositis patients demonstrated efficacy when given at a dosage of 1 g/kg/day for 2 days, repeated monthly for 3 months.54 The combination of intravenous immune globulin and cyclosporine may be of value.55 One controlled study suggested that intravenous immune globulin may be of benefit in IBM,56 but studies by another group failed to show clinical improvements.57 Treatment with intravenous immune globulin is limited by the restricted supply and very high cost and should be reserved for severe cases not responding to other therapies.
Skin protection
The rash of dermatomyositis is usually photosensitive. Therefore, attention to protection from the sun is very important, and patients should be advised to avoid sun exposure as much as possible. Sunscreen preparations, sun-protective clothing, and tinting of windows are often effective. Some dermatologists recommend use of |-carotene, 25 to 30 mg, taken twice daily initially and then increasing to no more than five times a day. Antimalarials may be of benefit, and one report suggests the use of topical tacrolimus.58
Physical therapy
Physical therapy plays an important role in the rehabilitation of patients with myositis. During the phase of active inflammatory disease, passive range-of-motion exercises are necessary to prevent contractures. Once the inflammatory compo-nent of the disease is controlled, active resistive exercises are useful in regaining muscle strength.