Disorders of Hyperpigmentation
Melasma
Definition
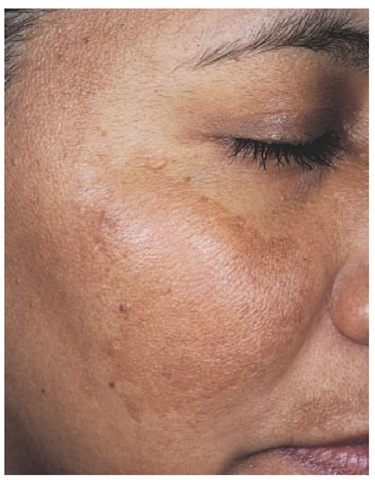
Melasma is a common acquired symmetrical hypermelanosis characterized by irregular light-brown to gray-brown macules involving the face. There is a predilection for the cheeks, forehead, upper lips, nose, and chin [see Figure 1]. Lesions may occasionally occur in other sun-exposed areas, including the forearms and back.1-3
Epidemiology
Melasma is most commonly observed in females. Men constitute only 10% of the cases but usually demonstrate the same clin-icopathologic features as women do. The condition affects all racial and ethnic groups but is most prevalent in persons with darker complexions (skin types IV through VI). It is also more common in geographic areas with intense ultraviolet radiation (sunlight), such as tropical and subtropical regions.
Etiology and Pathogenesis
Although the precise cause of melasma is unknown, multiple factors have been implicated in the etiology and pathogenesis of this condition. These factors include genetic influences, intense ultraviolet radiation exposure, pregnancy, oral contraceptive use, hormone replacement therapy, cosmetics, and phototoxic and antiseizure medications.
Endocrinologic studies of patients with melasma have shown varying results. Although a detailed study of nine women with melasma showed significantly increased levels of luteinizing hormone (LH) and low levels of estradiol, suggesting a role for subclinical mild ovarian dysfunction, a study of 26 women found no difference in LH, follicle-stimulating hormone (FSH), and a-melanocyte-stimulating hormone (a-MSH) levels between patients with melasma and control subjects.3 Another study reported increased expression of a-MSH in the affected skin areas of 10 women with melasma. a-MSH stimulates tyrosinase and melanin synthesis.
Clinically, the light-brown patches are commonly evident on the malar prominences, forehead, chin, nose, and upper lip. The patches may have a malar, centrofacial, or mandibular distribution. Histologically, an epidermal, epidermal-dermal, or dermal pattern of increased pigmentation occurs. Histologic studies document an increase in epidermal pigmentation, increased numbers of melanocytes, and increased activity of melanogenic enzymes.5 A Wood-light examination enhances the epidermal pattern of pigment deposition. Such epidermal lesions are most amenable to treatment.
The differential diagnosis of melasma includes other conditions that cause facial hyperpigmentation, such as postinflam-matory hyperpigmentation, drug-induced hyperpigmentation, lichen planus actinicus, and photosensitivity disorders.
Treatment
Current treatments for melasma include broad-spectrum sunscreens, 2% (over the counter) and 4% (prescription) hydro-quinone formulations, azelaic acid, kojic acid formulations, a-hydroxyacid products, retinoic acid, retinol, superficial chemical peels, and microdermabrasion.1,6-9 A triple-combination product containing 4% hydroquinone, 0.01% fluocinolone, and 0.05% retinoic acid has enhanced efficacy. This product was previously compounded by pharmacists, but it is now available as a commercial preparation (Tri-Luma cream, Galderma Laboratories) that has been approved by the Food and Drug Administration for treatment of melasma. Because the combination contains a fluorinated steroid, treatment should be limited to 8 weeks. Laser therapy offers minimal long-term success and, instead, may worsen the condition. Intense pulsed light therapy may offer some improvement in patients with melasma.10,11
Although all of these therapies reduce the severity of melas-ma, none are curative. Hence, it is essential for patients to rigidly adhere to a regimen of daily sun protection (e.g., using sunscreen or wearing protective clothing) to control the progression of melasma.
Postinflammatory hyperpigmentation
Definition
Postinflammatory hyperpigmentation is characterized by an acquired increase in cutaneous pigmentation secondary to an inflammatory process [see Figure 2 ]. Excess pigment deposition may occur in the epidermis or in both the epidermis and the dermis.
Figure 1 Melasma is characterized by hyperpigmentation of the cheek, forehead, and upper lip.
Epidemiology
All racial and ethnic groups are susceptible to postinflammatory hyperpigmentation, but the incidence of the condition is higher in persons with darker complexions. In a diagnostic survey of 2,000 African-American patients seeking dermatologic care, the third most common diagnosis was pigmentary disorders, of which postinflammatory hyperpigmentation was the most prevalent.
Etiology and Pathogenesis
Pigmentary changes may be a result of production of inflammatory mediators and altered cytokine production.12,13 Such changes may lead to an increase in the number and size of epidermal melanocytes. In addition, hyperpigmentation may be a consequence of pigmentary incontinence, with deposition of pigment in the upper dermis. Postinflammatory hyperpigmen-tation may be a sequela of conditions such as acne, allergic reactions, drug eruptions, papulosquamous disorders, eczematoid disorders, and vesiculobullous disorders.
Diagnosis
Clinically, postinflammatory pigmentary changes may be localized, circumscribed, or generalized. Lesions range in color from brown to black to ashen gray and usually follow the distribution of the primary dermatosis.
Treatment
Therapies for postinflammatory hyperpigmentation include over-the-counter and prescription hydroquinone preparations. Higher concentrations are indicated for moderate to severe involvement. Other treatments include azelaic acid, kojic acid, retinoic acid [see Melasma, above], and adapalene.
Frug-induced hyperpigmentation
Medications are a common cause of cutaneous hyperpigmen-tation. Lesions may be localized or generalized. Medications can also cause hyperpigmentation of the oral mucosa and nails. There may be some improvement upon withdrawal of the offending agent; however, drug-induced hyperpigmentation can persist for many years.
Medications causing drug-induced hyperpigmentation include oral contraceptives, hormone replacement therapies, antibiotics, antidepressants, antiviral agents, antimalarials, antihy-pertensives, and chemotherapeutic agents. Such medications include progesterone, estrogen, zidovudine (AZT), minocycline, tetracycline, bleomycin, hydrochlorothiazide, hydantoin, amio-darone, chlorpromazine, quinacrine, hydroxychloroquine, chloroquine, imipramine, amitriptyline, diltiazem, citalopram, hydroxyurea, doxorubicin, busulfan, daunorubicin, cisplatin, cy-clophosphamide, thiotepa, vinblastine, and vincristine.
Heavy-metal preparations can also cause hyperpigmentation. These preparations include arsenic, gold, silver, mercury, and bismuth.
Treatment with the Q-switched alexandrite laser has proven to be an effective treatment for drug-induced pigmentation.
Erythema dyschromicum perstans
Definition
Erythema dyschromicum perstans (EDP, or ashy dermatosis) is an acquired benign condition characterized by slate-gray to violaceous macules. It was first described in 1957.
Figure 2 Postinflammatory hyperpigmentation of the face may be secondary to acne vulgaris.
Epidemiology
EDP is reported most commonly in dark-skinned persons. However, cases have been reported globally and in all skin types. The disease appears to have a relatively equal frequency in men and women. It has also been reported in children.
Etiology and Pathogenesis
The precise cause of EDP is unknown. Studies suggest that pollutants, pesticides, hair dyes, chemicals, and drug exposure may play a role in the pathogenesis.23-28 Findings in light microscopic, ultrastructural, and immunofluorescent studies of EDP have been similar to those in studies of lichen planus, leading some investigators to postulate that EDP may be a variant of lichen planus. Other studies suggest that EDP is a distinct entity. Expression of intercellular adhesion molecule-I (ICAM-I) and major histocompatibility complex (MHC) class II molecules (HLA-DR) has been reported.29 These findings suggest that aberrant cell-mediated immunity may be involved in the pathogenesis of EDP.
Diagnosis
Clinically, the macules of EDP are ashen and may have an erythematous, slightly raised border during the early stages of the disease. Erythematous macules have also been described during the early stages. Areas of erythema eventually resolve, leaving slate-gray areas of pigmentation. The lesions are usually symmetrically distributed and vary in size from small macules to very large patches. Common sites of involvement include the face, neck, trunk, and upper extremities. Mucous membranes, palms, soles, and nails are usually spared. Light microscopic findings are slight epidermal atrophic changes, spongiosis, lym-phocytic exocytosis, and basal vacuolopathy in the epidermis, as well as lymphohistiocytic, lichenoid dermal infiltrates. In later stages, the lesions lack the epidermal changes and show increased deposition of dermal pigment.
Postinflammatory hyperpigmentation, idiopathic eruptive macular pigmentation, pityriasis rosea, lichen planus, fixed drug eruption, Addison disease, pinta, syphilis, macular amy-loidosis, hemochromatosis, and argyria must be distinguished from EDP.
Treatment
Therapies for EDP have been minimally effective. They include sunscreens, hydroquinone, topical corticosteroids, systemic steroids, griseofulvin, clofazamine, antibiotics, and antimalarials.30
Lentigines
Definition
A lentigo is a well-circumscribed, brown to brown-black mac-ule, usually less than 1 cm in size, that appears at birth or in early childhood. Lentigines occur in all skin types and may be found on any cutaneous surface, including the palms, soles, and mucous membranes. They do not darken with sun exposure. Lentigines can be localized and must be distinguished from freckles (ephelides). Clinical differentiating features include the later appearance of freckles (at 4 to 6 years of age) and their predominance on sun-exposed skin and increased frequency in redheads and fair-skinned persons. Freckles also tend to fade in winter and with advancing age.
Epidemiology
Multiple lentigines have been reported in 18.5% of black new-borns and 0.04% of white newborns. Solar lentigines have been reported in 90% of whites older than 60 years.
Diagnosis
Several types of lentigines are recognized, including lentigo simplex, solar lentigines, nevus spilus, lentigines induced by psoralens plus ultraviolet A (PUVA), generalized lentiginosis, and syndrome-related lentiginosis.
Lentigo simplex lesions may occur as solitary localized mac-ules or may be numerous and widespread. They often occur during the first decade of life and can be found on any cutaneous surface.
Solar (senile) lentigines, or so-called liver spots, are brown macules that appear late in adult life on chronically sun-exposed skin. These lesions are present in 90% of whites older than 70 years and occur in response to solar exposure. Solar lentigines correlate with the tendency to freckle and with two or more sunburns after 20 years of age.
Nevus spilus, or speckled lentiginous nevus, is a congenital brown patch on which dotted brown macules develop during childhood. Histologically, the brown patch has features of a lentigo, whereas the dotted brown macules most often reveal features of junctional nevi. Zosteriform patterns have also been described. Generalized lentiginosis is characterized by innumerable lentigines unassociated with other abnormalities.
Syndromes characterized by multiple lentiginosis include multiple lentigines (LEOPARD [multiple lentigines, electrocardiograph-ic conduction abnormalities, ocular hypertelorism, pulmonary stenosis, abnormal genitalia, retardation of growth, sensorineural deafness]) syndrome, Moynahan syndrome, centrofacial lentiginosis, Carney complex, Laugier-Hunziker disease, Peutz-Jeghers syndrome, and Bannayan-Ruvalcaba-Riley syndrome.31,32
The histopathology of lentiginosis shows elongated rete ridges, increased numbers of basal melanocytes, and increased basal melanization. In contrast, freckles result from hypermelaniza-tion of basal melanocytes without a concomitant increase in number.
Lentigo must be distinguished from other flat, pigmented lesions, including freckles, junctional nevi, postinflammatory hy-perpigmentation, and pigmented actinic keratoses.
Treatment
The treatment of lentigines includes hydroquinone-containing bleaching agents, cryotherapy, Q-switched neodymium:yttrium-aluminum-garnet (Nd:YAG) laser, and intense pulsed light.
Confluent and reticulated papillomatosis of gougerot and carteaud
Definition
The eruption of confluent and reticulated papillomatosis was initially described by Gougerot and Carteaud in 1927 and 1932. The condition consists of 2 to 5 mm hyperpigmented papules that have a predilection for the sternal area and midline of the back and neck.
Epidemiology
Confluent and reticulated papillomatosis occurs in equal frequency in men and women and shows no racial or ethnic predilections. The disease usually begins during the third decade of life.
Etiology and Pathogenesis
The precise cause of confluent and reticulated papillomatosis is unknown. Abnormal host response to Pityrosporum orbiculare (Malassezia furfur; the fungus that causes tinea versicolor), abnormal response to colonization by follicular bacteria, and genetically determined defects of keratinization have been suggested.35,36 The disease has been associated with Cushing syndrome, diabetes, hypopigmentation, and thyroid disorders.
Diagnosis
Patients present with 2 to 5 mm hyperpigmented, slightly ver-rucoid papules that have a predilection for the back, scapula, and inframammary areas. The papules become confluent near the midline and possess a reticulated pattern near the periphery. The lesions do not form a true scale but, rather, a mealy deposit that can be easily removed with the fingertips.
Histologically, studies show hyperkeratosis, decreased granular cell layers, papillomatosis, absence of sweat glands, and fragmentation of elastic fibers. Electron microscopic studies have shown increased numbers of transitional cells between the stratum granulosum and stratum corneum. This finding suggests premature keratinization. In addition, increased expression of keratin 16 has been reported, suggesting abnormal proliferation, differentiation, or both.36
Other conditions that simulate confluent and reticulated pa-pillomatosis are tinea versicolor and acanthosis nigricans.
Treatment
Minocycline is reportedly beneficial.37 Other treatments that have shown some efficacy include selenium sulfide shampoo, salicylic acid, urea, vitamin A, corticosteroids, calcipotriol, tetra-cycline, erythromycin, doxycycline, retinoids, and PUVA.