Definition
Malabsorption refers to the impaired intestinal absorption of nutrients. It can result from congenital defects in the transport of nutrients or from acquired defects in the absorptive surface of the intestinal epithelium. Maldigestion, another factor in nutrient absorption, refers to the impaired digestion of nutrients within the intestinal lumen. Although these two processes are patho-physiologically distinct, they are interdependent; and in clinical practice, malabsorption has come to signify derangements in both processes.
Overview of Diseases Producing Malabsorption
Malabsorption is clinically defined as impaired absorption of fat (steatorrhea), because measuring fat absorption is the best indicator of the normality of the overall process of nutrient absorption. Under certain conditions, however, fat absorption may be normal but other substances may be poorly absorbed, such as iron, calcium, bile salts, or, in certain hereditary conditions, specific amino acids, disaccharides, or monosaccharides.
Etiology
Generally, there are three possible causes of fat malabsorp-tion: small bowel disease, liver or biliary tract disease, and pancreatic exocrine insufficiency [see Table 1].
Small Bowel Disease
Small bowel disease can result in moderate amounts of fat in the stool (7 to 30 g/day on a diet containing 100 g of fat). Patients with small bowel disease may leak protein (protein-losing en-teropathy) through a diseased intestinal mucosa, which results in a reduced serum albumin concentration. Deficiencies of fat-soluble vitamins (i.e., vitamins A, D, E, and K) may be present in small bowel disease. Patients may malabsorb vitamin B12 because of a very diseased or previously resected (usually over 60 cm) terminal ileum. Folic acid may also be malabsorbed, and hypocalcemia and hypomagnesemia may also be present.
Liver or Biliary Tract Disease
Patients with liver or biliary tract disease usually have only small increases in fat in the stool (7 to 15 g/day) and may also malabsorb fat-soluble vitamins. The association of cholestatic liver disease, especially primary biliary cirrhosis, with osteoporosis is well known. Osteoporosis may be the presenting symptom of the liver disease. Vitamin K deficiency, as shown by a prolonged prothrombin time, may also occur. Administration of vitamin K corrects the clotting defect in cases where the extent of the liver disease is not severe enough to impede clotting factor synthesis.
Pancreatic Exocrine Insufficiency
Patients with pancreatic exocrine insufficiency may have up to 80 g of fat/day in the stool. That they absorb fat at all is the result of the action of gastric lipases. Gastric lipase is present in the chief cells of the human stomach1 and is thought to account for any lipid absorbed in the setting of chronic pancreatitis as exemplified by cystic fibrosis. Indeed, in cystic fibrosis, an increase in gastric lipase has been reported.2
Clinical manifestations
The symptoms of malabsorption are protean. In the most obvious case, the patient complains of weight loss despite a good appetite. In these cases, there is a clear change in the quality of the stool and usually an increase in stool number. The consistency of the stool softens, and in the presence of excess fat, the stool becomes more malodorous and is difficult to flush down the toilet. Oil drops or a lipid sheen may appear on the water. Excess gas in the stool causes the stool to float.
Depending on other dietary constituents that are malab-sorbed, patients may experience a distended abdomen, borbo-rygmi, abdominal cramps (lactose intolerance), easy bruising (vitamin K deficiency), osteopenia or tetany (vitamin D deficiency and calcium malabsorption), iron deficiency, or night blindness (vitamin A deficiency). The most challenging cases are those in which the question of malabsorption is not raised because of lack of change in the quality of the stools.
The diarrhea of malabsorption is classified as an osmotic diarrhea and usually stops during fasting. In fat malabsorption, the diarrhea is caused not only by the excessive osmotically active particles but also by fatty acids, which stimulate cyclic adenosine monophosphate (cAMP)-dependent Cl secretion.
Table 1 Causes of Malabsorptive Syndromes
|
Diseases of the small intestine |
Gluten-sensitive enteropathy |
|
Tropical sprue |
|
|
Collagenous sprue |
|
|
Eosinophilic enteritis |
|
|
Radiation enteritis |
|
|
Amyloidosis |
|
|
Mastocytosis |
|
|
Abetalipoproteinemia |
|
|
Whipple disease |
|
|
Intestinal lymphangiectasia |
|
|
Immunoproliferative small intestinal |
|
|
disease |
|
|
Ischemic bowel disease |
|
|
Giardia lamblia infection |
|
|
AIDS |
|
|
Short bowel syndrome |
|
|
Ileal resection |
|
|
Ileitis (e.g., Crohn disease) |
|
|
Diseases of the liver and biliary tract |
Cirrhosis/parenchymal liver disease |
|
Intrahepatic cholestasis syndrome |
|
|
Cholestasis due to extrahepatic |
|
|
obstruction |
|
|
Diseases of the pancreas |
Chronic pancreatitis |
|
Cystic fibrosis |
|
|
Cancer |
|
|
Combined or multiple defects in digestion and absorption |
Hyperthyroidism |
|
Diabetes mellitus |
|
|
Carcinoid syndrome |
|
|
Zollinger-Ellison syndrome |
|
|
Postgastrectomy (Billroth II type) |
Table 2 Tests of Digestive-Absorptive Function
|
|
Characteristics |
Clinical Use |
|
Fecal fat analysis Qualitative Quantitative |
Simple microscopic study for increase in fat globules Chemical analysis for fat excretion during a 72 hr period by titration with NaOH; most sensitive test for malassimilation of fat; normal is < 6 g/day; does not distinguish between small intestine, pancreatic, or luminal abnormalities |
A good screening test for moderate increase in stool fat, but quantitative fecal fat analysis is preferable The most important test to identify maldigestion or malabsorption; indicated in all patients suspected of having malassimilation |
|
Xylose absorption |
As a pentose not requiring luminal or intestinal surface digestion, xylose allows assessment of small intestine function; normally, > 4 g/5 hr is excreted in urine after ingestion of 25 g; plasma xylose should be 10-20 mg/dl/1.73 m2 of body surface area at 60-75 min |
Indicated whenever quantitative fecal fat is abnormal; not as sensitive as fat analysis but localizes the abnormality to the small intestine |
|
Small intestine x-ray |
Allows analysis of continuity of small intestine and identification of diverticula or alteration of mucosa; diseased pancreas may impinge on duodenum |
Indicated when quantitative fecal fat excretion is increased |
|
Small intestine peroral biopsy |
Permits direct histologic examination of mucosa; characteristic alterations occur in several diseases producing malabsorption |
Indicated when fecal fat excretion is increased, particularly if the xylose test or small intestine x-ray is abnormal; a portion of biopsy may be assayed for disaccharidases |
|
Bile acid breath test |
In small intestine bacterial overgrowth or ileal disease that produces malabsorption, 14C-glycocholic acid (5 ^Ci) will be deconjugated, metabolized, and excreted via the lungs as 14CO2 |
Indicated in patients with documented steatorrhea caused by suspected bacterial overgrowth or ileal dysfunction |
|
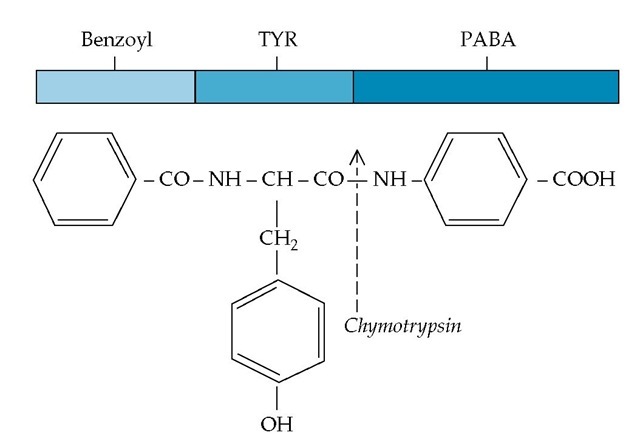
Bentiromide test |
The peptide bond in this nonabsorbable arylamine is cleaved specifically by intraluminal chymotrypsin to yield PABA, which is then readily absorbed and excreted by the intestine |
Indicated when fecal fat excretion is increased; less sensitive than quantitative fat analysis but, when positive, establishes insufficiency of intraduodenal pancreatic digestive enzyme levels Not available in U. S. |
Specific physical findings of various diseases may accompany the malabsorptive state and assist in making the diagnosis. For example, the skin changes of scleroderma or dermatitis herpeti-formis may be present. Signs of diabetic neuropathy may be disclosed. Although thyrotoxicosis may be associated with excessive fat in the stool, patients with thyrotoxicosis usually eat gluttonously but absorb a normal percentage of dietary fat eaten (95%) and therefore do not malabsorb in the true sense.
Tests for suspected malabsorption
The tests for malabsorption involve determining whether there is excessive fecal fat excretion [see Table 2]. Protein is produced in large quantities by the digestive tract, especially the pancreas, making creatorrhea difficult to interpret. Malabsorbed carbohydrate delivered to the colon may be metabolized by colonic bacteria to short-chain fatty acids, which are in part absorbed by the colon. Thus, the quantitative measurement of carbohydrate absorption is inaccurate, although a fall in stool pH occurs, which is indicative of excessive amounts of the short-chain fatty acids that are excreted under these conditions.
Measurement of Fecal Fat
Fecal fat can be measured qualitatively and quantitatively. The qualitative measurement of fecal fat using Sudan III staining has been shown to be surprisingly accurate,4 especially if clinically significant amounts of fat are being excreted. One group reported that counting and measuring the size of fat globules present in the stool significantly improved the sensitivity and specificity of the Sudan assay.4 As with many qualitative tests, however, accuracy varies with test performance and interpretation, making the skill of the observer crucial to success.
The quantitative measurement of fecal fat is the benchmark by which all other tests are ranked. It is important to remember that the test cannot be performed unless the patient is able to eat at least 80 g, preferably 100 g, of fat a day.
Xylose Absorption Test
The absorptive surface area of the intestine is measured by the ability of the patient to absorb xylose, a sugar. Unlike glucose, xylose is not actively absorbed by the intestine but is absorbed by the slower process of passive diffusion. In the xylose absorption test, 25 g of xylose is given by mouth and the urine is collected for 5 hours. The normal urinary excretion of xylose is greater than 4 g over 5 hours. For an adequate urinary flow to be ensured, the patient should drink 500 ml of water after drinking the xylose. This intake should result in a urine volume of at least 300 ml during the collection period. Xylose excretion can be falsely low in patients with reduced renal function or in patients with ascites in which the xylose is diluted in the ascitic fluid. To avoid falsely low results, it is advisable to measure the concentration of xylose in blood [see Table 2]. Malabsorbed xylose reaches the colon and can be metabolized by the resident bacteria to hydrogen. Hydrogen may be quantitated in the breath; this test is reported to be as accurate as the measurement of xylose in the serum or urine.
Imaging Studies
A plain film or ultrasonogram of the abdomen is usually not helpful in most cases of malabsorption. However, 30% of cases of chronic pancreatitis have visible calcifications on an abdominal plain film. Detection of pancreatic calcification can be increased if computed tomography or ultrasonography is used. CT or ultrasonography also can identify dilatated pancreatic ducts, another characteristic sign of chronic pancreatitis. Endo-scopic retrograde pancreatography (ERP) can also be helpful when ductular changes indicative of chronic pancreatitis are seen [see 4:V Diseases of the Pancreas].
Radiographic studies of the small intestine after oral ingestion of barium can aid in the diagnosis of several abnormalities. The
Figure 1 Cleavage of the bentiromide molecule by the intraduodenal enzyme chymotrypsin yields two fragments, benzoyl-tyrosine and aminobenzoic acid (PABA). Bentiromide is composed of benzoyl (light blue), tyrosine (TYR) (blue), and PABA (dark blue). The released PABA is absorbed across the intestine and excreted in significant quantities in the urine. Absence of chymotrypsin, as a result of pancreatic disease or duct obstruction, will result in failure of release, absorption, and urinary excretion of PABA.
Small Bowel Biopsy
An experienced pathologist can be helpful in supporting the diagnoses of gluten-sensitive enteropathy (with or without dermatitis herpetiformis), hypogammaglobulinemic sprue, tropical sprue, Whipple disease, Mycobacterium avium complex disease, stasis syndrome, amyloidosis, and intestinal lymphangiectasia.