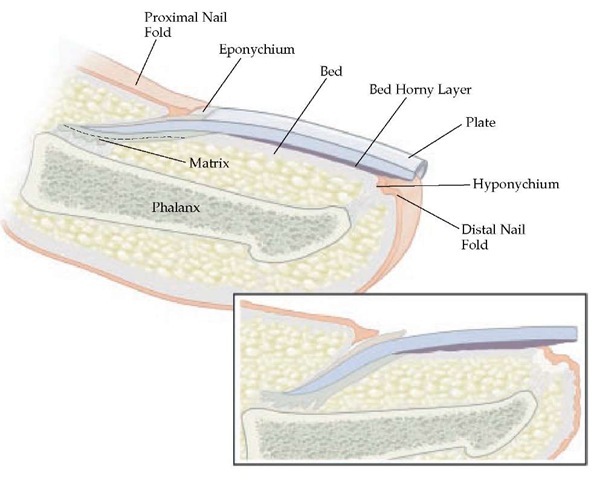
The human nail is a complex unit composed of five major modified cutaneous structures: the nail matrix, nail bed, nail plate, nail folds, and cuticle (eponychium).1 These components are structurally supported by specialized mesenchyme, which provides a ligamentlike function, anchoring the soft tissue structures of the nail to the underlying phalangeal bone. The primary function of the human nail is to provide protection for the distal digits. Nails also assist in performance of fine touch and digital dexterity. For many individuals, nails serve as an important aesthetic symbol of optimal appearance, enhanced self-image, or individuality; several cosmetic techniques are available to modify the appearance of the nail plate. The basic anatomic components of the nail unit are diagrammed [see Figure 1].
Nail Structure, Function, and Pathophysiology
Nail matrix
The nail matrix is the dynamic, germinative portion of the nail unit that produces the nail plate.2-4 The lunula is the visible portion of the nail matrix, appearing under the proximal nail plate as a gray-white half moon projecting just distal to the proximal nail-fold cuticle. That lunula decreases with age in approximately 20 % of persons.5
Nails are usually devoid of pigmentation because of the relatively sparse number of melanocytes present in matrix epithe-lium.1,2 Because nail-matrix or nail-bed melanocytes tend to be more numerous in blacks, Asians, and Hispanics, persons of these racial backgrounds may present more commonly with diffuse or banded nail-plate or nail-bed hyperpigmentation.
Pathophysiology Affecting the Nail Matrix
Because of the diagonal orientation of the ventral nail matrix, the proximal portion of the nail matrix produces the superior portion of the nail plate.6 As a result, disorders of the proximal matrix produce surface abnormalities of the nail plate. A characteristic example is nail-plate pitting secondary to psoriasis. Diseases of the distal nail matrix result in abnormalities of the undersurface of the nail plate, changes that are visible at the free edge of the nail, or both. Permanent damage to the matrix as the result of trauma, surgical intervention, or disease may result in permanent nail-plate dystrophy.
Nail bed
The nail bed is a layer of epithelium lying between the lunula and the hyponychium (the distal epithelium at the free edge of the nail). The surface epithelium of the nail bed is longitudinally ridged, with small superficially oriented vessels coursing along the same axis, interdigitating with a complementary array of ridges on the undersurface of the nail plate.3 This anatomic feature explains the longitudinal linearity of splinter hemorrhages, which are foci of extravasation wedged between the bed and the plate. As outgrowth of the nail plate occurs, splinter hemorrhages progress distally.
Pathophysiology Affecting the Nail Bed
The epidermis of the nail bed is thin and minimally kera-tinized, without a granular layer. If there is prolonged loss of nail plate as a result of disease or surgical intervention, in creased nail-bed keratinization with development of a granular layer prevents the firm attachment of the ingrowing nail plate to the underlying nail bed. Melanocytes are more sparsely distributed in nail-bed epithelium than in the nail matrix [see Nail Matrix, above]. The dermal layer of the nail bed is very thin and is supported by very sparse subcutaneous tissue; it is firmly attached to the underlying bony phalanx.
Figure 1 Longitudinal section of the fingernail. Major components of the nail include the nail matrix, nail plate, eponychium, hyponychium, nail bed, and the proximal and lateral nail folds.
Nail plate
The nail plate, which is composed of densely compacted keratinized epithelial cells, is produced by the matrix and progesses distally toward the free edge of the nail as newly formed plate slowly pushes forward in a distal direction. Formation and outgrowth of the nail plate is a continual process. A fully formed nail plate extends from below the proximal nail-fold cuticle to beyond the hyponychium and extends laterally below the cuticle of the lateral nail folds. Nail-plate abnormalities frequently occur secondary to changes or disorders affecting function of the nail matrix; infections such as onychomyco-sis; or trauma.
Age-Related Nail-Plate Findings
The growth rate of an adult fingernail plate is approximately 3 mm/mo, with marked variability among individuals.2 Toe-nail plate growth occurs at one third to one half the rate of fingernail growth. A general rule is that adult fingernails take approximately 6 months to grow out fully; adult toenails, 12 to 18 months. Nail-plate growth is faster in children, peaking between 10 and 14 years of age; there is a slowly progressive decline after the second decade of life.2 Linear nail-plate growth decreases by 50 % over a lifetime, with periods of slow decline alternating with periods of rapid decline in approximate 7-year increments.7 Nail-plate growth increases during pregnancy and decreases during lactation, after use of chemotherapeutic agents, and in conditions characterized by limb paralysis, persistently diminished circulation, or malnutrition.2,3,8 Yellow nail syndrome is characterized by very slow or absent growth of nail plate; it usually affects both fingernails and toenails and is seen in association with several underlying conditions, such as lymphedema, respiratory disorders (e.g., bronchiectasis and pleural effusions), and nephrotic syndrome.9
Constitutional age-related findings in the nail plate include changes in nail color and luster, longitudinal ridging, changes in convexity, and brittle nails.8,10 Nail plates, especially of toe-nails, often develop a yellow or gray color with a dull, opaque appearance. Longitudinal ridging may affect some or all nails and may present as slightly indented grooves or projection ridges or as beading. Over time, the surface of the nail plate may become flattened (platyonychia) or spooned (koilonych-ia). Temporary koilonychia, especially of the toenails, is also seen in infants.6
Pathophysiology Affecting the Nail Plate
Brittle nails is a common complaint; its incidence is 20% in the overall population (27% in female patients) and increases with advancing age.10 When nail water content falls below 16%, nail plates become brittle; when the water content rises above 25%, nail plates become soft. The most common cause of brittle nails is dehydration, which can be caused or exacerbated by external factors such as use of nail-polish remover or exposure to dry climate. Onychoschizia, which presents as a layered, superficial splitting of the nail plate, may increase in incidence with age. This condition is seen much more frequently in female patients. It is likely related to recurrent exposures to water or irritants, such as during nail-care procedures.
Fingernails demonstrate a tendency to become thinner and more fragile over time. Toenails usually become thicker and harder. Onychogryphosis is a marked thickening, usually of the large toenail, resulting in a compacted mass of heaped-up dystrophic nail plate.8 Contributing factors appear to be advanced age, poor nail care, chronic trauma, decreased peripheral circulation, and neuropathy. Poor-fitting shoewear causes long-term exposure to lateral pressure and friction, resulting in gryphotic changes (marked thickening or heaping of nail plate), usually of the first and fifth toenails.
Nail folds
The nail folds are the cutaneous soft tissue that houses the nail unit, invaginating proximally and laterally to encompass the emerging nail plate. The proximal nail fold, with the exception of the lunula, covers the underlying matrix and is devoid of sebaceous glands and dermatoglyphic skin markings.11 The term paronychia describes inflammation of the nail folds. Paronychia may be acute or chronic and may occur secondary to a variety of conditions, including contact dermatitis, psoriasis, bacterial infection, and fungal infection.12,13 The cuticle (eponychium) is a thin, keratinized membrane of modified stratum corneum that extends from the distal portion of the nail fold, reflecting onto the nail-plate surface. Intact cuticle serves as a seal that protects the space between the nail folds and the nail plate from exposure to external irritants, allergens, and pathogens. Loss of cuticle allows for exposure and trapping of these deleterious external agents, providing an environment in which either inflammatory or infectious paronych-ia can develop.
Nail Findings Associated with Disease States
Several nail findings have been associated with both underlying systemic and dermatologic conditions. The following is a review of selected, recognized associations. Diagnosis is based on proper evaluation of clinical findings; treatment is based on a confirmed etiology or the recognition of an underlying systemic association.
Special care must be taken when performing biopsy of the nail bed or matrix to avoid trauma to the tissue specimen and surrounding structures upon specimen removal. The most appropriate plane of dissection during nail-bed or nail-matrix biopsy is subdermal. The sampled tissue should be manipulated very gently throughout the biopsy procedure to avoid crush artifact, which may interfere significantly with histopathologic evaluation. It is also important to carefully dissect along the un-dersurface of the specimen, ensuring nontraumatic separation of the biopsy tissue from its underlying firm attachment to bone.
Splinter hemorrhages
Splinter hemorrhages may be secondary to trauma, high altitude, primary dermatoses (i.e., psoriasis), or several underlying conditions (e.g., arterial emboli, collagen vascular disease, or thromboangiitis obliterans). The simultaneous appearance of splinter hemorrhages in several nails should raise suspicion of a possible underlying systemic disorder, especially in female patients.
Koilonychia
Koilonychia may be found in association with other conditions, including congenital conditions, iron deficiency anemia, cardiac disease, endocrinopathy, occupational exposures, and trauma.
Transverse nail-plate depressions (beau lines)
Beau lines present as well-delineated, transverse depressions in the nail plate. They are believed to occur secondary to temporary growth arrest of the nail matrix. The grooves become evident weeks after the occurrence of an abrupt, stressful event, such as an acute febrile illness. The width of the groove reflects the duration of interrupted nail-matrix function. When limited to one or a few digits, Beau lines may be associated with trauma, carpal tunnel syndrome, or Raynaud disease, or they may occur subsequent to tourniquet application during hand surgery.15 Approximately 1 to 2 months after birth, infants may demonstrate physiologic Beau lines, which mark the transition from intrauterine to extrauterine life.16 Multiple transverse grooves (stepladder appearance) may be seen in as-sociation with repeated cycles of chemotherapy, or they may be related to zinc deficiency. Multiple Beau lines should not be confused with the multiple transverse depressions that are stacked longitudinally along the central nail plate (washboard nails), resulting from the obsessive habit of repeatedly pushing back the cuticle or picking at the proximal nailfold margin (habit-tic deformity) [see Figure 2].15,17 There is no specific treatment for Beau lines. They grow out over time after resolution of the growth-arrest period.
Figure 2 Stacking of transverse linear grooves traversing the entire length of the central nail plate, resulting from the repeated picking of the proximal nail fold margin (habit-tic deformity). Note the marked hypertrophy of the lunula, which is typical of this disorder.
Figure 3 Colonization of the closed space between the nail bed and nail plate with Pseudomonas aeruginosa, causing a green nail. Moisture trapped in the onycholytic space provides an optimal environment for proliferation of this bacterium.
Onycholysis
Onycholyis is defined as the separation of the nail plate from the nail bed. In most cases, onycholysis begins distally; it is often related to acute or chronic trauma that produces a lever effect, lifting the nail plate upward and away from its bed. Other causes of onycholysis are chemical exposure (allergic or irritant dermatitis), onychomycosis, and primary der-matoses (e.g., psoriasis or lichen planus).13 Associations with underlying systemic disease (e.g., thyroid disease) have been sporadically reported but are less commonly encountered in clinical practice. When moisture accumulates under ony-cholytic nail plate, bacterial proliferation may occur. This can cause a green discoloration of the nail plate as a result of a pigment produced by certain organisms (e.g., Pseudomonas aeruginosa) [see Figure 3].
Treatment requires avoidance of precipating factors for ony-cholysis, debridement of separated nail plate, and the twice-daily topical application of diluted acetic acid solution (consisting of equal parts white vinegar and water), gentamicin, or the combination of polymyxin B and bacitracin.18
Leukonychia
Leukonychia, a white discoloration of the nail plate or subun-gual tissue, has multiple presentations. Small 1 to 3 mm white spots (punctate leukonychia) or irregular transverse streaks (leukonychia variegata) of the nail plate are the most common varieties.15 These two presentations are generally secondary to repeated microtrauma to the matrix, growing out distally with outgrowth of the nail plate. Mee lines specifically refer to transverse 1 to 2 mm white bands, which usually are demonstrated at the same site in multiple nails and reported in association with arsenic intoxication, Hodgkin disease, sickle cell anemia, renal failure, and cardiac insufficiency. Leukonychia is also associated with systemic infection and chemotherapy.19-21
Half-and-half nails (Lindsay nails) present as a diffuse, dull whitening of the proximal nail bed that obscures the lunula and as a distal region of pink or reddish-brown discoloration that occupies from 20% to 60% of the nail length.15,22 The most commonly reported association with half-and-half nails is chronic renal failure. When the distal brown band of discoloration constitutes less than 20% of the total nail length, the anomaly is known as Terry nails, which occurs in association with chronic congestive heart failure, hepatic cirrhosis, type 2 (non-insulin-dependent) diabetes mellitus, and advanced age. In both half-and-half nails and Terry nails, the proximal portion of the nail bed may be light pink, exhibiting a more normal appearance, rather than white.
Muehrcke nails present as paired, white, narrow transverse bands of the nail bed, separated by normal-appearing thin pink bands.15,22 Muehrcke nails have been associated with chronic hypoalbuminemia. Resolution of this nail finding correlates with normalization of serum albumin levels.15
Clubbing
When the normal angle between the proximal nail fold and the nail plate exceeds 180°, digital clubbing is present. The morphologic changes of clubbing typically include hypertrophy of the surrounding soft tissue of the nail folds as a result of hyper-plasia of dermal fibrovasculature and edematous infiltration of the pulp tip.21 Radiologic changes are identified in fewer than 20% of cases.15
Clubbing may be hereditary, or it may be seen in association with several underlying disease states, such as hypertrophic pulmonary osteoarthropathy, chronic congestive heart failure, congenital heart disease associated with cyanosis, poly-cythemias associated with hypoxia, Graves disease, chronic hepatic cirrhosis, lung cancer, Crohn disease, and irritable bowel disease.15,22,23 When clubbing is unilateral, consideration should be given to underlying causes of obstructed circulation, such as aneurysm, arteriovenous fistula, and a pulmonary sulcus tumor (Pancoast tumor); disorders producing soft tissue edema; and diseases causing localized changes in underlying digital bone (e.g., sarcoidosis). Unilateral clubbing can also be found in cases of hemiplegia,24 and a case of subungual perineurioma caused by unilateral clubbing has been reported.25 Paronychia and distal phalangeal resorption may cause changes that simulate true clubbing (pseudoclubbing).
Nail-plate pitting
Nail-plate pitting (onychia punctata) develops as a result of focal defects in nail-plate formation from the proximal nail matrix. The number, size, and shape of the superficial depressions may vary.15 The extent and duration of involvement with nail pitting correlates with the duration of nail-matrix abnormality. Psoriasis, the most common association with nail pitting, may produce a random array of shallow or deep pitted indentations, usually affecting one or more fingernails.26,27
Psoriasis of the nails often responds poorly to treatment, and it tends to recur. Topical corticosteroids, topical tazarotene, and intralesional corticosteroid injection may help in some cases.28,29 It is a common misconception that nail pitting is pathogno-monic for psoriasis.27 Nail pitting may also be seen in association with alopecia areata, punctate keratoderma, idiopathic tra-chyonychia, occasionally in normal nails, and rarely in association with collagen vascular disease or syphilis. Fingernail pitting occurs in one third of children with alopecia areata; mild disease involving only a few nails is observed in approximately 20% of cases.27 Compared to psoriasis, nail pitting seen in alopecia areata is typically more uniform and patterned, often presenting as orderly rows of shallow pitted depressions. Currently, there is no available treatment for this type of nail pitting.