Contact dermatitis is an acute or chronic skin inflammation resulting from interaction with a chemical, biologic, or physical agent.1 It is one of the most common conditions seen by physicians, accounting for more than 6.5 million physician visits a year and 95% of all reported occupational skin diseases.2 Substances that produce contact dermatitis after a single exposure or multiple exposures may be irritant or allergenic. Direct tissue damage results from contact with irritants. Tissue damage by allergic substances is mediated through immunologic mechanisms. Eczema or dermatitis is the most common clinical expression of this induced inflammation. Of the more than 85,000 chemicals in our environment, most can be irritants, depending on the circumstances of exposure.1 More than 3,700 substances have been identified as contact allergens.3 The potential for these substances to cause contact dermatitis varies greatly, and the severity of the dermatitis ranges from a mild, short-lived condition to a severe, persistent, job-threatening, and possibly life-threatening disease.
Major Types of Contact Dermatitis
Irritant contact dermatitis
Irritants cause as much as 80% of cases of contact dermatitis, act by direct nonimmunologic chemical or physical action on the skin, and are divided into marginal and acute types. Marginal irritants are the most common. Repeated daily exposures to low-grade irritants such as soap, detergents, surfactants, organic solvents, and oils may not cause clinical changes for days or months. Dryness of the skin with a glazed, parched appearance are often the initial signs; erythema, hyperkeratosis, and fissur-ing may supervene.
In contrast, acute irritants cause a more immediate reaction. Some irritants, such as strong acids and alkalis, aromatic amines, phosphorus, and metallic salts, produce a marked observable effect within minutes.4,5 Others, such as hydrofluoric acid, ethyl-ene oxide, podophyllin, and anthralin, produce a reaction within 8 to 24 hours after exposure.4 Acute irritant contact dermatitis (ICD) is usually easily diagnosed by the patient history and often results from occupational accidents. The clinical appearance varies depending on the irritant and ranges from burns and deep-red ulcerations with sharp circumspection of the dermatitis, sometimes with a gravitational, dripping effect, to a vesicular dermatitis that is indistinguishable from acute allergic contact dermatitis.
Almost any substance can be an irritant, depending on the conditions of exposure [see Figure 1]. The nature of the irritant (i.e., its pH, solubility, physical state, and concentration), the duration of contact, and the nature of the vehicle affect disease severity. Host factors that predispose to ICD include preexisting dermatitis, skin dryness, sweating, and decreased thickness or breaks in the stratum corneum; environmental factors include high temperature, low humidity, friction, and pressure.
ICD provoked by work materials is believed to be a frequent cause of occupational skin disease. In one large population- based study, the highest annual incidence rates of ICD were reported for hairdressers (46.9 per 10,000 workers per year), bakers (23.5 per 10,000 workers per year), and pastry cooks (16.9 per 10,000 workers per year).6 The causative factors of ICD are complex and usually involve exposure to a combination of irritants. The sentinel event for irritant hand eczema in hairdressers is dermatitis developing in moist areas that are difficult to rinse and dry, such as under rings and in the web spaces of the fin-gers.7 Dermatitis may spread to the dorsum of the hand, where the skin is thinner and less resistant than on the palms.
No universally accepted test exists for diagnosing ICD, which is often diagnosed by excluding allergic contact dermatitis (ACD). Because of the clinical similarities between allergic and irritant contact dermatitis, it is important that patients who are thought to have either disorder undergo patch testing, the results of which are positive with ACD and negative with ICD.
ICD may become chronic if it is not treated early [see Treatment of Irritant and Allergic Contact Dermatitis, below]. Even when the skin appears to be healed, its protective capacity remains impaired for weeks or months. Additionally, ICD impairs the barrier function of the skin, allowing penetration of potential contact allergens. Individuals who had childhood atopic eczema are more likely than others to develop ICD of the hands when their jobs involve wet work.
Allergic contact dermatitis
Allergic contact dermatitis is a type 4, T cell-mediated, delayed hypersensitivity reaction in the skin. The disorder affects only certain sensitized individuals, typically after two or more exposures, and accounts for about 20% of contact dermatitis cases.
Figure 1 Wearing a plastic bib resulted in irritant dermatitis in an 18-month-old child.
Table 1 Body Sites Often Affected by 10 Common Contact Allergens
|
Allergen |
Common Uses |
Localization Site |
|
Nickel |
Costume jewelry |
Earlobes, neck, fingers, wrists, abdomen |
|
Neomycin |
Topical antibiotics (dermatologic; ophthalmologic; ear, nose, throat) |
Face, neck, trunk, extremities |
|
Balsam of Peru |
Fragrances, cosmetics, medications, flavorings |
Face, trunk, extremities, perianal area |
|
Fragrance mix |
Toothpaste, fragrances, toiletries, cosmetics |
Same as for balsam of Peru |
|
Thimerosal |
Topical antiseptic, contact lens solutions, eye cosmetics, nasal sprays |
Eyelids, face, neck (relevance hard to prove) |
|
Gold |
Jewelry |
Eyelids, earlobes, wrists, fingers |
|
Formaldehyde |
Cosmetics (preservative), shampoos, nail enamel |
Eyelids, face, neck, trunk (especially intertriginous areas) |
|
Quaternium-15 |
Cosmetics (preservative), shampoos, soaps, lotions |
Face, trunk, extremities, hands |
|
Cobalt |
Metal-plated objects, jewelry |
Earlobes, neck, fingers, wrists |
|
Bacitracin |
Topical antibiotics (dermatologic; ophthalmologic; ear, nose, throat) |
Face, neck, trunk, extremities |
Predisposing Factors
Immunologic status Predisposing factors to ACD include the patient’s immunologic status, which in turn is influenced by genetics, age, gender, and the presence of systemic disease. Patients with AIDS, severe combined immunodeficiency, advanced lymphoma or other malignancy, sarcoidosis, leproma-tous leprosy, cachexia, and atopic dermatitis may have impaired cell-mediated immunity or anergy.8 However, contact allergy should not be excluded in these individuals, especially those with atopic eczema. In experimental models, agents that affect the immune system, such as ultraviolet light (ultraviolet B or psoralen and ultraviolet A [PUVA]), glucocorticoids, cyclo-sporine, and various other drugs, may downregulate ACD.8 Administration of systemic corticosteroids below certain dosages (e.g., prednisone, 20 mg or less daily), however, does not inhibit strong patch-test reactions.
In patients with occupational dermatitis, a form of natural hyporeactivity termed hardening may occur with diminished but continued exposure to chemical irritants. The process is inducible and is not localized.10 This acquired state of unrespon-siveness, when describing adaptation to allergens, is called tolerance.
Environment The chemical environment in which we live defines opportunities for exposure to various allergens. A patient’s age, gender, occupation, avocation, habits, and nationality are among the factors that determine the environment and thus the chemicals to which an individual is exposed. The most common source of contact allergy in the United States is Toxico-dendron, a plant genus that includes poison ivy, poison oak, and poison sumac. In addition to Toxicodendron, 10 sources of contact allergens are commonly encountered in North America [see Table 1],11 and numerous other allergens are known to cause contact reactions.3
Other cutaneous disorders Skin that is infected, inflamed, burned, or eczematous predisposes a patient to ACD. Patients with stasis, hand and foot eczema, or chronic actinic dermatitis are at high risk for ACD. ACD occasionally occurs with other skin disorders, including seborrheic dermatitis, psoriasis, pruri-go nodularis, and benign familial pemphigus (Hailey-Hailey disease).12 Noneczematous contact reactions have also been reported: purpuric reactions caused by black rubber; lichen planus-like eruptions caused by color-film developers, gold, and other dental metals (oral mucosa); and granulomas caused by beryllium and zirconium.12
Pathogenesis
Some inflammatory immune reactions in ACD are the same as those in ICD—specifically, the two disorders have similar cytokine activity (tumor necrosis factor-a and interferon gamma) and accessory molecule activity (HLA-DR and intercellular adhesion molecule-1) producing the cascade of inflammation. However, there is no memory T cell function in ICD,13 and the extent of reaction is directly related to the amount of irritant and duration of exposure.14 In contrast, even small amounts of an allergen can trigger the T cell reaction in ACD. Minor variations in an allergen’s physical and chemical properties may affect its ability to induce sensitization.8 Most environmental allergens are haptens-that is, they are small (< 500 daltons) molecules that penetrate the skin and undergo in vivo conjugation with tissue, or carrier, protein. Once the complex forms, the carrier protein is no longer recognized by the immune system as self. ACD represents a delayed-type hypersensitivity reaction to this complex.
During the sensitization phase, which usually takes a minimum of 5 to 21 days, an individual acquires a specific hypersen-sitivity to a particular contact allergen. Sensitization not only can evoke a type 4 delayed hypersensitivity response (mediated by lymphocytes) but also can produce a type 1 immediate hyper-sensitivity reaction (mediated by circulating antibodies).
On reexposure to an allergen, a hapten-carrier complex capable of eliciting a specific reaction re-forms. The reaction time— the time required for a previously sensitized individual to manifest a clinical dermatitis after reexposure to the antigen—is usually 12 to 48 hours but may range from 8 to 120 hours.
A spontaneous flare may occur within 10 to 21 days without reexposure, possibly because enough allergen remains at the site to cause a reaction once the sensitization phase has occurred.
Cross-sensitization occurs when a patient who is allergic to one chemical also reacts to structurally related chemicals. Examples include Toxicodendron antigens (poison ivy, oak and sumac Japanese lacquer, mango, and cashew nutshell oil), aromatic amines (p-phenylenediamine, procaine, benzocaine, and p-aminobenzoic acid), and perfumes or flavors (balsam of Peru, benzoin, cinnamates, and vanilla). This phenomenon may explain persistence or reactivation of dermatitis when such exposures are unknown.8,12,15
Diagnosis
Diagnosis of ACD is based on the patient history; on the appearance, periodicity, and localization of the eruption; and on the clinical course. The history is especially important in cases of chronic dermatitis and putative occupational contact dermatitis. The history alone may be accurate only 50% of the time, on average, ranging from 80% accuracy for nickel to 50% accuracy for moderately common allergens to about 10% accuracy for less common allergens. Even with causes that are considered obvious, the specific allergen may not be known, and ACD that is caused by other chemicals may also be present. Skillful history taking is required to differentiate ACD from contact urticaria and ICD, with differentiation being especially difficult in chronic cases [see Table 2].16 Also important is detailed questioning of the patient about all topical medications (over-the-counter and prescription), systemic medication, cosmetics, other lotions and creams, occupation, hobbies, travel, and clothing. A history of hypersensitivity to one or more of the major contact allergens (e.g., nickel, rubber, topical medications, and cosmetics [fragrances, preservatives, and dyes]) or obvious occupational or avocational exposures to certain substances or chemicals (e.g., chrome, epoxy, acrylics, latex gloves, clothing, first-aid creams, preservatives, and plants) may point to the diagnosis of ACD in an otherwise unexplained eruption.16
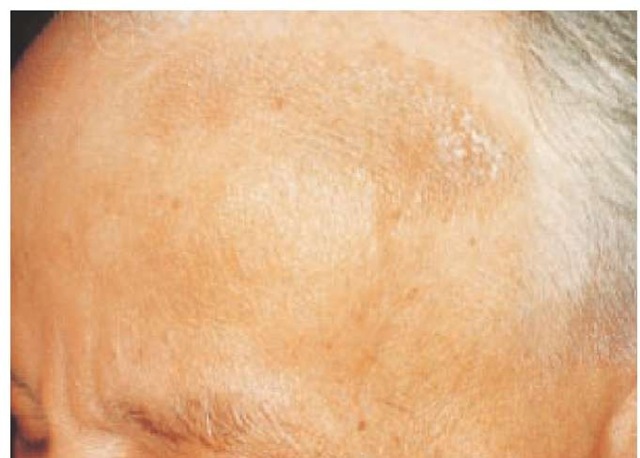
Clinical features In the acute stage, papules, oozing vesicles, and crusting lesions that are surrounded by inflammation predominate. These clinical features may occur anywhere, but they are best visualized on the palms, sides of the fingers, peri-ungual areas, and soles of the feet. Frequently occurring or persistent episodes of ACD often become chronic; lesions associated with chronic ACD may appear thickened and exhibit licheni-fication, scaling, and fissuring [see Figures 2 and 3]. Post-inflammatory hyperpigmentation or hypopigmentation may occur. In the subacute stage of ACD, features characteristic of both acute and chronic ACD may be present. All forms of contact dermatitis frequently cause pruritus. The onset of ACD is often subtle. A low-grade, subacute to chronic eczema may appear as primarily a scaly or chapped eruption, especially on the face or on the dor-sa of the hands.12,16
The distribution of dermatitis is often the single most important clue to the diagnosis of ACD. The area of most intense dermatitis usually corresponds to the site of most intense contact with the allergen. Exceptions occur, such as nail-polish allergy, which typically appears on ectopic sites, especially the eyelids, face, and neck. In addition to the transfer of allergens to distant sites, volatile airborne chemicals may cause dermatitis on exposed body areas. Regional differences in susceptibility to contact allergens exist. Thinner eyelid and genital skin is more susceptible to both allergic and irritant contact dermatitis. Because head hair is often protective of the scalp, allergic reactions to hair cosmetics frequently involve the upper face, eyelids, postauricu-lar area, and neck. Other areas of the body have higher or lower exposures to various allergens; these exposures are not always clear and are reflected in unusual distributions of dermatitis.
Table 2 Common Misconceptions about ACD49
|
Fallacy |
Truth |
|
Rash quickly follows contact |
Rash is often delayed 1 to 2 days and may not appear for 1 wk after contact |
|
Allergy develops only to new substances |
Allergy can develop years after contact; an induction period may last virtually a lifetime |
|
Allergy is dose-dependent |
Allergy is not, within a wide range, dose-dependent |
|
If changes in medications or cosmetics do not lead to clearing of the rash, those products are not the cause |
Many products contain the same or cross-reacting allergens; also, the composition of the product may be altered without a change in the trade name of the product |
|
Contact allergy occurs only at the site of exposure to the offending agent |
Contact allergy can spread by direct or indirect contact, airborne exposure, connubial contact, or autoeczematization |
|
Expensive products are not allergenic |
Allergy is not related to cost |
|
Negative prick or scratch test or RAST excludes ACD |
Only patch testing is diagnostic of ACD |
|
ACD is always bilateral if allergen exposure is bilateral |
Shoe and glove allergy are often bilateral but may be unilateral |
|
ACD is of the same intensity at all areas of exposure |
Body sites may differ in responsiveness to allergens; ACD may be patchy (e.g., hand dermatitis from gloves) |
|
ACD does not affect the palms and soles |
ACD may occur on the palms and soles (e.g., from gloves, topical medicaments, shoes) |
ACD—allergic contact dermatitis RAST—radioallergosorbent test
Figure 2 Exposure to poison oak produced this acute Toxicodendron dermatitis with erythema, edema, and linear vesicles and bullae.
Figure 3 Chronic eczematous dermatitis, with scaling, lichenification, and hyperpigmentation, was caused by an allergy to leather components in a hatband.
Allergens in lotions and creams applied all over the body sometimes produce reactions in skin folds and intertriginous areas, where the chemicals tend to concentrate. Recognition of ACD on the basis of the physical examination alone may be only partially accurate. Linear vesicular streaks are commonly seen in poison ivy, poison oak, and poison sumac dermatitis, but contact with other plants can give a similar picture. Contact with liquids may also produce linear vesicles. Failure to examine the entire skin surface may result in misdiagnosis. Eczema on the trunk and arms may in fact represent autoeczematization from contact or stasis dermatitis of the legs. Significant regional variations are associated with contact dermatitis, and knowledge of substances that cause dermatitis of specific body sites facilitates the diagnosis. Three such areas are the hands, face and neck, and feet [see Figures 4 through 7].
If the history and clinical presentation reveal one or more risk factors for ACD, a patch test is indicated [see Table 3 and Patch Test, below]. The differential diagnosis of ACD is extensive, and a list of key points can be useful in establishing an accurate diagnosis [see Table 4].
Histopathology Biopsies are of limited help in diagnosing contact dermatitis. Microscopic findings vary according to the stage of the process: acute, subacute, or chronic. The hallmark of eczema is spongiosis, or intercellular edema, associated with spongiotic vesicles. Intracellular edema may cause reticular degeneration of the epidermis with multilocular bullae formation. Most types of eczema show similar pathologic changes and cannot be distinguished with certainty.17
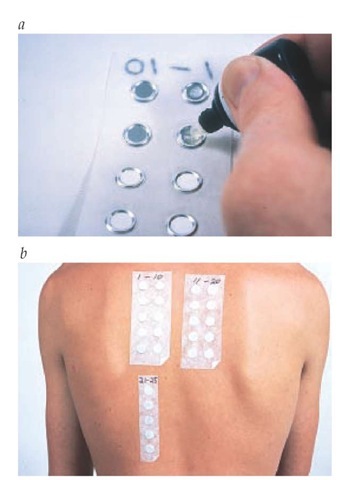
Patch test The patch test is the only useful and reliable method—the gold standard—for the diagnosis of ACD. The proper performance and interpretation of this bioassay require considerable experience.
Figure 4 Acute contact dermatitis caused by wearing sandals typically involves the dorsal surface of the feet.
Figure 5 Hairdresser with acute allergic contact dermatitis of the hands, caused by glyceryl thioglycolate.
Figure 6 Ectopic allergic contact dermatitis of the eyelids from tosylamide formaldehyde resin in nail polish.
Because the procedure is subject to patient variability and observer error, the technique has been standardized by the North American Contact Dermatitis Group. First, the allergen is diluted in petrolatum or water to a concentration that does not produce active sensitization or irritation. A widely used patch-test system consists of strips of paper tape, onto which are fixed aluminum disks 8 mm in diameter (Finn Chambers on Scanpor tape). A small amount of allergen is placed within these disks, covering slightly more than one half of its diameter [see Figure #]. Currently, the only commercially available patch-test system in the United States is the thin-layer rapid-use epicutaneous (T.R.U.E.) test. The T.R.U.E. test contains 23 preloaded allergens that are crystallized, micronized, or emulsified into gels that are affixed to paper tape.
With both systems, the tests are applied to the upper back or midback, which must be free of dermatitis. The patches are left in place and kept dry. When removed at 48 hours, the first reading is performed after 20 to 30 minutes, which allows time for pressure erythema to resolve. It is important to perform a second reading between 4 and 7 days after the patches are initially applied; otherwise, almost 20% of positive reactions will be missed. Neomycin, formaldehyde and formaldehyde-releasing preservatives, and tixocortol pivolate are often late reactors. Results at both readings are graded according to intensity of the reaction covering at least 50% of the patch-test site on a scale of 0 to 3+, as follows:
0 = no reaction
? (doubtful) = weak erythema only
1+ = erythema and edema
2+ = erythema, edema, and papules
3+ = vesicles or bullae
Both false positive and false negative reactions can result. Thus, patch testing is best done by physicians who are familiar with the intricacies of the procedure and who have been trained to advise patients about allergen substitution, relevance of the test, and prognosis. Reading test results and interpreting relevance are as important as performing the test. Any reaction must be evaluated with regard to the individual patient. Thus, when an allergen is found to be positive, it cannot always be assumed to be the cause of ACD.
Figure 7 Allergic contact dermatitis of the hands (a) and neck (b), with a positive patch test to rosin (colophony) (c).
|
Table 3 Criteria* for Determining Which Patients with Putative ACD Should Be Patch Tested49 |
|
Presence of a specific type of eczema that places patient at higher risk for ACD (stasis, hand, foot, or chronic) |
|
Patient is in a high-risk occupation |
|
Health care worker |
|
Cosmetologist (hairdresser) |
|
Rubber compounder |
|
Plastics processor |
|
Chemical worker |
|
Printer |
|
Machinist |
|
Woodworker |
|
Specific allergen or substance is suspected |
|
Patient has a highly suggestive history or distribution of dermatitis |
|
Dermatitis flares or does not respond to treatment |
|
Patient has previously undiagnosed dermatoses and erythroderma |
|
Patient has putative occupational dermatitis |
|
Special situation applies, such as photosensitivity or systemic contact dermatitis |
*Test is ordered if any one of the risk factors is present.
The relevance of positive reactions to present or past episodes of ACD ranges from a low of 7.2% for thimerosal to 93.4% for dimethylol-dimethylhydantoin (DMDM hydantoin) and diazolidinyl urea [see Table 5]. Thus, relevance is determined by correlating the patch-test results with chemicals, products, and processes encountered in the environment. Occasionally, when patients are allergic to chemicals in products they use, the allergen may be present in only minimal amounts and may not be responsible for the dermati-tis.8 In these cases, repeat open application testing (ROAT), in which the patient applies the commercial product to normal skin twice daily for several days, can be helpful. ROAT is typically used with products that are left on rather than washed off after application.
In the United States, patch testing for ACD is often initially performed using the T.R.U.E. test; however, because there are over 3,700 environmental contact allergens and this test screens for only 23 allergens, testing with additional chemicals is imperative for a thorough evaluation. In one study, the T.R.U.E. test series of 23 allergens would have completely identified all allergens in only 25.5% of patients and clinically relevant allergens in 28% of patients.18 Additional substances can be obtained from chemical suppliers and prepared by a compounding pharmacist in appropriate concentrations, as detailed in a standard text, for testing with the Finn Chamber system. As an alternative, many centers in the United States use individual patch-test chemicals or series (e.g., corticosteroid, plastics and glues, acrylic, dental, machinist, hairdresser) that are available in Europe but have not been approved in the United States.11,19
Reproducibility and validity of patch testing In a study in which 383 patients received simultaneous duplicate patch tests on opposite sides of the upper back, 8% of patients had completely discordant results: positive on one side of the back and negative on the other.20 The intensity of the reactions was not disclosed, and clinical relevance of this problem was considered small. The most reproducible positive patch tests were for fragrance mix, nickel, and balsam of Peru. Formaldehyde and lanolin were the least reproducible positive reactors, both of which may be weak irritants.20 The sensitivity, specificity, and validity of a standard screening series has been estimated at about 70%,21 indicating that about 30% of these patch-test results were not valid. The patients whose screening results were negative later had positive results to other allergens. It was assumed that the earlier screening results had been false negative. A study of 500 consecutive patients who received identical patch testing reported discordant results in 5% of patients; the investigators concluded that patch testing is a reasonably reproducible procedure as long as methodological error is minimized.22
The positive predictive value of a diagnosis of ACD is a function of the prevalence of ACD in the population and a function of the sensitivity and specificity of the patch test.23 A large dose-response study that tested the impact of seasonal variation on the irritant susceptibility of skin identified a stronger reaction to irritants in winter.24
Table 4 Key Points in the Diagnosis of ACD
|
Key Points |
Examples |
|
ACD may be identical to another disease |
Tinea pedis misdiagnosed as ACD; a positive potassium hydroxide preparation made the diagnosis |
|
Psoriasis of the soles misdiagnosed as ACD caused by shoes; patch tests were negative |
|
|
Factitial eczema of the dorsal hand misdiagnosed as ACD; cured with an Unna Boot occlusive dressing ACD caused by fragrances and preservatives; misdiagnosed for 5 yr as lupus erythematosus |
|
|
ACD caused by hair tonic; misdiagnosed as seb-orrheic dermatitis |
|
|
ACD caused by sunscreen; misdiagnosed as sunburn |
|
|
ACD may be concurrent with another disorder |
ACD caused by neomycin; misdiagnosed as worsening atopic eczema |
|
Chronic actinic dermatitis of the face can be present with ACD caused by a fragrance |
|
|
Morphea of the leg can be present with ACD caused by a topical corticosteroid cream |
|
|
ACD may be caused by an occult exposure to an allergen |
Keys in pants pocket caused ACD of the lateral thigh in a man allergic to nickel |
|
ACD caused by the preservative imidazolidinyl urea, present in a sunscreen with a label that listed only the active ingredients |
|
|
Chronic hand eczema from ACD caused by red dye in window curtains |
|
|
Diagnosis of ACD may be elusive because of inadequate or deceptive history |
Patient allergic to neomycin had periorbital contact eczema caused by an ophthalmic ointment that contained tobramycin, which was not recognized as a cross-reacting allergen |
|
Chronic eczema worsened by use of a topical cream (doxepin) identified only from a pharmacy prescription list |
|
|
Initial patch testing may not provide accurate diagnosis |
Occupational contact dermatitis of the hands attributed to a false positive irritant-patch-test reaction to a cleanser |
|
Occupational contact dermatitis of the hands with a false negative patch-test reaction to latex surgical gloves; further patch testing indicated an allergy to thiurams, which were present as accelerators in the gloves |
Figure 8 Patch-test allergens to be tested, usually in petrolatum and occasionally aqueous, are placed on Finn Chambers on Scanpor tape (a) for application to the patient’s back (b) for 48 hours. See patch testing in text and Figure 7c for a positive patch test.