Polyarteritis nodosa
Polyarteritis nodosa is an inflammatory condition that affects muscular arteries [see 15:VIII Systemic Vasculitis Syndromes]. Aneurysms form in many arteries, including those leading to the kidneys and subcutaneous tissue. Diagnosis of the systemic form of polyarteritis can be made by demonstrating aneurysms of the renal arteries on renal arteriograms.
A localized cutaneous form of polyarteritis nodosa most commonly presents as painful nodules of the lower extremities.63
Figure 19 Several of the characteristic cutaneous findings of tuberous sclerosis are shown: adenoma sebaceum (a); ash-leaf macule (b); and periungual fibromas (c).
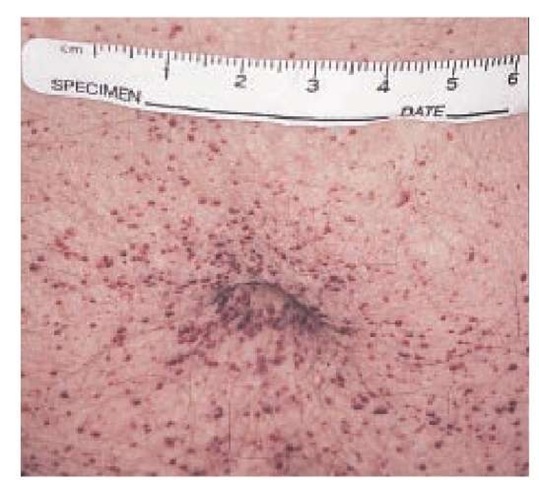
Figure 20 Angiokeratomas are particularly common in the periumbilical area of patients with Fabry disease.
In mild cases, patients may only have livedo reticularis; but in severe cases, skin lesions can ulcerate. A polyneuropathy may be associated with the disorder. Patients with classic poly-arteritis and microaneurysms have an increased incidence of hepatitis B antigenemia; in contrast to patients with other vas-culitides, they usually do not have antineutrophil cytoplasmic antibodies.
Perforating disorders
Perforating disorders include several conditions characterized by extrusion of dermal material through the epidermis. These lesions often develop in association with renal failure and diabetes mellitus.65 Skin lesions are characterized by hyperkera-totic papules with central white craters that histologically can be shown to contain dermal material. Reactive perforating col-lagenosis, perforating folliculitis, and Kyrle disease are all examples of perforating disorders associated with renal failure.
Calciphylaxis
Calciphylaxis, also known as calcific uremic arteriolopathy, is a condition of patients with renal failure in which localized areas of skin become necrotic as a result of vascular calcification. Calci-phylaxis begins with painful purpuric patches that may be reticulated, resembling livedo reticularis. These patches progress to indurated plaques that may ulcerate, becoming necrotic [see Figure 21]. Calciphylaxis often eventuates in amputation or death. Parathyroidectomy may result in healing of affected skin without amputation.66
Figure 21 Calcification of arteries in patients with renal failure results in calciphylaxis. Affected skin forms a black, necrotic eschar.
Rheumatologic Diseases
Dermatomyositis
The best-known cutaneous manifestations of dermatomyosi-tis, an inflammatory disorder of muscle and skin, are Gottron papules and heliotrope erythema. Gottron papules are erythe-matous scaling macules and papules that occur on the dorsa of the knuckles [see Figure 22]. Heliotrope erythema consists of periorbital erythema and edema. Scalp lesions, which can be associated with alopecia, have been described.67 The lesions are often misdiagnosed as seborrheic dermatitis or psoriasis.
The association between dermatomyositis and malignancy has been established68,69; one epidemiologic study indicates patients with dermatomyositis are at particular risk for ovarian and lung cancer.69
Classifications of dermatomyositis include a juvenile variant characterized by calcification of skin or muscle. A vasculitic form in children is complicated by cutaneous infarcts and ulcer-ation and by gastrointestinal vasculitis with abdominal pain, bleeding, or perforation. The vasculitic form carries a poor prognosis, with many of the patients dying of this disease.
Scleroderma and scleroderma-like diseases
The sclerodermas include a number of distinct syndromes sharing a common feature, induration of the skin [see 15:V Scle-roderma and Related Diseases].
Progressive Systemic Sclerosis and CREST Syndrome
Progressive systemic sclerosis, also known as systemic sclero-derma, is a frequently fatal disease in which patients present with Raynaud phenomenon and sclerodactyly (induration of the skin of the digits) [see Figure 23]. Cutaneous induration can become widespread. Involvement of the face can lead to a characteristic appearance with pursed lips and bound-down skin of the nose that creates a beaklike appearance. Patients with antibodies to Scl-70 have a poor prognosis, often succumbing to renal disease and malignant hypertension. Pulmonary fibrosis can occur. Patients with anticentromere antibodies have a more slowly progressive variant of scleroderma known as the CREST syndrome, which is characterized by cutaneous calcinosis, Ray-naud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia. With time, pulmonary hypertension and right-sided heart failure develop.
Figure 22 Erythematous scaling papules on the dorsal aspects of the knuckles (Gottron papules) are a sign of dermatomyositis.
Figure 23 Sclerodactyly with a nonhealing digital ulcer commonly occurs in progressive systemic sclerosis.
Morphea
Morphea, also called localized scleroderma, is characterized by sharply demarcated patches of indurated skin that can become generalized. It is distinguished from progressive systemic sclerosis by the absence of Raynaud phenomenon, sclerodacty-ly, or the systemic complications of scleroderma. There have been innovations in the treatment of both progressive systemic sclerosis and morphea. Exposure to psoralen and longwave ultraviolet light (PUVA) has been reported to improve progressive systemic sclerosis and morphea dramatically,70 and exposure to UVA1 (the longer UVA spectrum, from 340 to 400 nm) has been reported to benefit patients with localized scleroderma.71 Anecdotal evidence suggests that topical calcipotriene is an effective treatment for morphea.72 Further studies must be done to confirm the efficacy of these treatments. Anecdotal reports have indicated that minocycline may benefit patients with progressive systemic sclerosis, but controlled trials are needed.73
Graft versus Host Disease
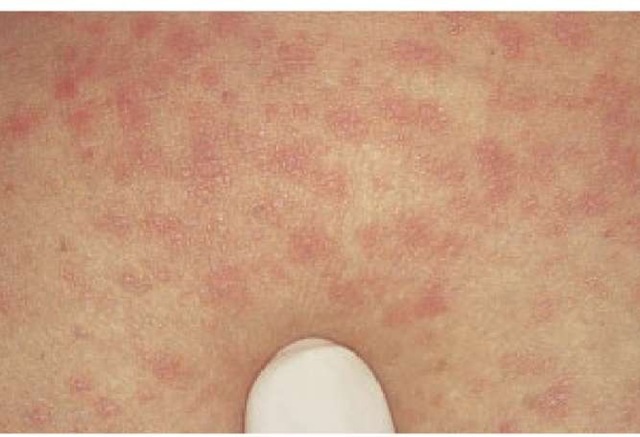
As organ transplantation becomes more common, another scleroderma-like illness, graft versus host disease, increases in frequency, particularly after bone marrow transplantation [see 5:X Transfusion Therapy and 5:XI Hematopoietic Stem Cell Transplantation]. There are two stages of graft versus host disease. The first, acute graft versus host disease, develops 10 to 40 days after transplantation and consists of an erythematous macular and papular rash that is often associated with fever, hepatomegaly, lym-phadenopathy, or gastrointestinal symptoms. Chronic graft versus host disease usually develops 3 months after transplantation but can occur later; it consists of purple papules resembling lichen planus [see Figure 24]. Sclerodermatous skin changes with telan-giectasia, reticulated hyperpigmentation, and alopecia are most characteristic. Both cyclosporine and PUVA have proved to be useful in the prevention and treatment of graft versus host dis-ease.74,75 Infliximab has been used very successfully to treat acute graft versus host disease.76
Eosinophilic Fasciitis
Scleroderma-like hardening of the skin also occurs in eosinophilic fasciitis. Puckering of the skin on the extremities typically develops and is associated with pain. In contrast to progressive systemic sclerosis, Raynaud phenomenon does not occur. Definitive diagnosis requires biopsy of skin and fascia overlying the affected muscle. In some cases of eosinophilic fasciitis, hematologic abnormalities develop, including aplastic anemia, thrombocytopenia, Hodgkin disease, and leukemias.77
Systemic lupus erythematosus
There are many cutaneous manifestations of systemic lupus erythematosus (SLE), including nonspecific manifestations such as Raynaud phenomenon, photosensitivity, alopecia, and mu-cosal ulcers. More specific cutaneous manifestations of SLE include so-called discoid lupus (characterized by round scarred skin lesions with central hypopigmentation and a rim of hyper-pigmentation) and malar erythema [see 15:IV Systemic Lupus Erythematosus]. As we learn more about lupus, the spectrum of skin diseases associated with this disorder continues to expand. Subacute cutaneous lupus, a variant characterized serologically by anti-Ro and anti-La antibodies, is associated with annular or psoriasiform skin lesions [see Figure 25].
Anticardiolipin Antibody Syndrome
The anticardiolipin antibody syndrome, which can occur in patients with SLE, has been described in patients who suffer repeated episodes of phlebitis, arterial thromboses, and repeated miscarriages.
Figure 24 Flat-topped papules are seen in this chronic lichenoid graft versus host reaction.
Figure 25 Annular scaling erythematous patches are characteristic of subacute cutaneous lupus erythematosus.
Cutaneous infarcts are common manifestations, and livedo reticularis can occur. Patients may have false positive serologies for syphilis and have a circulating lupus anticoagulant. Circulating antiphospholipid antibodies are the serologic hallmark of this syndrome; however, many asymptomatic persons have antiphospholipid antibodies,78 and antiphospholipid antibody tests can have false negative results. In some patients, a battery of tests may be needed to establish diagnosis; the dilute Russell viper venom time, an assay for circulating lupus anticoagulant, has been found to be among the more sensitive tests.79
Livedo Vasculitis
Livedo vasculitis, another disorder that has been associated with lupus, is characterized by painful recurrent ulcers over the lower legs and ankles. The ulcers heal, leaving white sclerotic scars. Affected patients often have livedo reticularis. This condition, also known as atrophie blanche, has been attributed to thrombotic processes rather than immune complex deposition or leukocytoclastic vasculitis.80
Neonatal Lupus
Neonatal lupus is a distinct syndrome of annular, erythema-tous macules and papules occurring on the face of newborn infants. The disorder has been attributed to transplacental passage of anti-Ro and occasionally anti-La antibodies. Mothers are often asymptomatic, but some may have lupus or Sjogren syndrome. Congenital heart block is the most serious complication of this disorder.81