Pit vipers
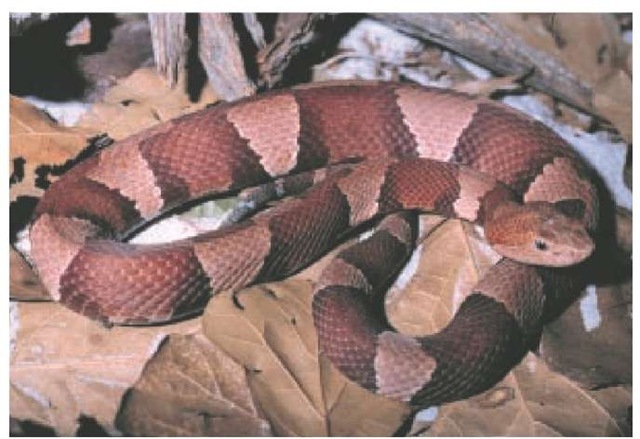
In the United States, pit vipers (Crotalidae) are found in all states except Maine, Alaska, and Hawaii. South America has nine subspecies of rattlesnakes; Mexico and Central America have four subspecies of rattlesnakes. These snakes can be found in a variety of habitats and at elevations up to 14,000 ft. The eastern and western diamondback rattlesnakes (Crotalus adamanteus and C. strox) [see Figure 2] are the largest and most dangerous in the United States and are found in the southwestern states and in Nevada, California, and Oklahoma.54,55 The timber rattlesnake (C. horridus) is the second most dangerous rattlesnake common to the eastern United States, but it is rarely found in Delaware, Maine, Michigan, or Washington, D.C. Pigmy rattlesnakes (Sistrurus catenatus and S. miliarius) are found in areas ranging from New York to Michigan and from Texas to Arizona; they have the least toxic venom of all of the rattlesnakes.51 Overall, rattlesnakes are responsible for 65% of envenomations in the United States. Their venom is 2.5 to 5 times more toxic than other North American species of venomous snakes.50 Cottonmouths (Agkis-trodon piscivorus), also known as water moccasins, live in the southern and southeastern states along streams and in low-lying trees. Copperheads (A. contortix) [see Figure 3] are found in mountains, rock piles, and sawdust piles. Their range extends from Massachusetts southwest to Texas. Cottonmouths and copperheads have only moderately toxic venom; their bite is painful but rarely fatal. In a study of 400 copperhead bites, 32 of which were treated with antivenin, 88% of bites responded to the antivenin, as evidenced by a cessation of local tissue injury progression.
Pit vipers are identified by a small depression (pit) between the eyes and the nostrils bilaterally. They have a triangular-shaped head, an elliptical pupil, and fangs that fold back when the mouth is closed and unfold via a hingelike mechanism when the mouth is opened. The pit is a heat-sensitive organ that enables the snake to locate live, warm-blooded prey. Snakes can detect movement at a distance of about 40 ft. They can strike at a distance of approximately half their body length. Rattlesnakes use their rattle when threatened or endangered, not necessarily just when they are about to attack. The pit viper is aggressive and will stand its ground when provoked or cornered.54,55 The venom is stored in glands that are located on each side of the head above the maxillae and behind the eyes. The glands are similar in function to the human submaxillary glands. The snake may discharge anywhere from 25% to 75% of its venom when biting a human. The fangs are either hollow or grooved. Even young snakes are venomous, and the venom of young snakes may be 12 times as strong as the venom of adult snakes.
Envenomation
Toxicology
Snake venom has both neurotoxic and hematotoxic properties. The venom is a complex mixture of hydrolases, polypep-tides, glycoproteins, and low-molecular-weight compounds. Snake venom, especially that of the Elapidae and Hydrophidae families, contains polypeptides that produce neuromuscular blockade at the presynaptic or postsynaptic terminals, or both, causing a flaccid paralysis. Composition of the venom varies greatly between species and between individual snakes. Viper venom is mainly cytotoxic, Elapidae (cobra, coral) venom is usually neurotoxic, and Hydrophidae (sea snake) venom is mainly myotoxic.57
Figure 1 The nose of the coral snake is black, and the body has black, red, and yellow bands. The black bands do not separate the red and yellow bands, as they do on the nonvenomous but similarly banded kingsnake. Snake shown is an eastern coral snake, Micrurus fulvius.
Figure 2 Diamondback rattlesnakes are the largest and most dangerous rattlesnakes in the United States. Shown is an eastern diamondback rattlesnake, Crotalus adamanteus.
Figure 3 The copperhead (Agkistrodon contortix) has a geographic range that extends from Massachusetts southwest to Texas. Bites from these snakes are painful but rarely fatal.
Snake venom has profound effects on coagulation pathways, causing a hypercoagulable state. Over the first few hours after a person is bitten, thrombocytopenia occurs, with a platelet count of less than 10,000/mm3, a decrease in fibrinogen, and an increase in fibrin degradation products. The venom proteins may induce distention of the vascular basement membrane and capillary matrix.58 Prothrombin time and partial thromboplastin time increase with severe envenomation. Usually, these increases occur because consumption of coagulation factors results in clinical anticoagulation. In dog experiments, activation of fibrinolysis may be preceded by thrombus formation, with clotting of critical vessels in the coronary vasculature, which can lead to cardiac arrest and death. This may also explain pulmonary emboli, as the thrombus formation may occur in the legs and cause deep vein thrombosis.59 Drops in hematocrit may also occur, along with so-called burring of erythrocytes.54 Approximately 53% of patients experience coagulopathy 2 to 14 days after envenomation. In one study, 76% of patients with pit viper envenomations developed coagulopathy during their hospital course.60 The coagulopathy may last up to 26 days.
Clinical Features
From 30% to 50% of snakebites do not result in envenomation. The snake can control the amount of venom injected and may inject up to 90% of its venom to immobilize its prey. Other factors involved in the injection of venom include the health of the snake; its satiety; the condition of the fangs; the toxicity of the venom; whether the snake is injured; and the size, age, and health of the victim.
Minor pit viper envenomation causes local pain and swelling (edema with a diameter of approximately 1 to 5 in.), without systemic symptoms or signs. Moderate envenomation is characterized by greater edema (diameter of 6 to 12 in.), weakness, sweating, nausea, fainting, dizziness, ecchymoses, and tender ade-nopathy.51 As the envenomation becomes more severe, the symptoms increase to include tachycardia, tachypnea, hypothermia, hypotension, ecchymoses, paresthesias, fasciculations, gin-gival bleeding, hematemesis, hematuria, melena, oliguria, epi-staxis, intracerebral hemorrhage, or coma.58 Fasciculations are a characteristic manifestation of bites from the eastern diamond-back rattlesnake.61 The skin around and over the snakebite will develop a tense, discolored bulla with serous or hemorrhagic fluid. Death usually results from hemorrhage, increased vascular permeability, and thromboembolic events secondary to disruption of the coagulation pathways.
Coral snake envenomation is painful and has the appearance of scratch marks with no surrounding edema. Systemic symptoms are delayed by about 1 to 6 hours. They begin with pares-thesias around the wound margins, followed by weakness, apprehension, giddiness, nausea, vomiting, and a sense of euphoria. Excess salivation is nearly always present.61 Bulbar and cranial nerve paralysis and ptosis may develop. Ptosis is very common and is often the first sign of coral snake envenomation. Diplopia, papillary dilatation, salivation, dysphagia, and respiratory failure may occur. The paralysis may last up to 14 hours, and full strength may not return for 6 to 8 weeks. In fatal cases, the usual cause of death is respiratory failure.
Viperid venom may increase vascular permeability, leading to bleeding into the gastrointestinal or genitourinary tract. In addition to the obvious signs and symptoms, renal failure may occur secondary to hemorrhage, coagulopathy, or secondary shock. Intracranial hemorrhage, especially into the anterior pituitary gland (leading to Sheehan syndrome) has been seen in envenomation by the Russell viper. Nephrotic syndrome, glomeru-lonephritis, hemolytic-uremic syndrome, and DIC have an incidence of 1.4% to 28%, especially in envenomations by the Russell viper, puff adder, and sea snake.
Treatment
First Aid
Treatment in the field should focus on preventing systemic absorption of the toxin. This may be done with compressive dressings and immobilization of the bitten extremity. Stabilization may be accomplished via an inflatable splint. Nothing should be given by mouth.
If signs of envenomation begin to occur, a constriction band to impede lymphatic flow should be placed on the extremity, proximal to the bite.63 The Commonwealth Serum Laboratory technique (Australia) uses an elastic band or air splint for wrapping the extremity. The Monash method uses a thick pad and tight bandage over the wound site to impede flow of the venom. Both of these methods have proven efficacy only with Elapidae bites. Transport to a hospital should take place immediately, because the absorption of neurotoxic venoms may result in respiratory compromise or arrest. In patients with a facial envenomation, edema may cause airway obstruction, so emergency response personnel may have to establish immediate airway control.
The site should be wiped off and cleaned. However, the old practice of incising the bite site and applying suction to remove the snake venom should not be used. This practice, which dates from the 1920s, was tested in animal models and found not to increase survival. In fact, incision and suction at the wound site poses more hazard than benefit. The incision may aggravate bleeding, damage nerves and tendons, introduce infection, and delay healing. Cryotherapy (e.g., placing ice on the bite site), which was once thought to lower venom enzyme activity and absorption into the systemic circulation, has also been shown to provide no significant benefit; rather, it causes tissue loss, cold injury, and possible permanent disability.
Extraction therapy has also fallen out of favor. In this procedure, a suction device is placed over the fang wounds, and suction is applied to remove the venom from the bite site and the surrounding tissue without an incision. Prehospital personnel who find a suction device already in place when they arrive at the scene should remove the device, provided there is no fluid accumulating in the cup.64 The use of field first-aid methods such as incision and suction, tourniquets, and cryotherapy has been associated with a threefold increase in the likelihood of the need for surgical intervention.50
Although popular belief has it that snakebites kill within minutes, in fact, the toxicity from snake venom usually does not even begin to affect the body for several hours. In one review, 64% of deaths from snakebite occurred between 6 and 48 hours after the patient was bitten.
Emergency Department Management
History When a snakebite victim arrives at the hospital, the history of the bite should be obtained. This should include (1) a description of the snake, (2) the time elapsed since the bite, (3) the circumstances surrounding the bite, (4) the number of bites, (5) the location of the bite, (6) the type of first aid administered, and (7) any symptoms that have occurred since the bite. The patient’s past medical history and allergy history should be reviewed briefly. In particular, the clinician should ask whether the patient has ever experienced allergic symptoms around horses or on exposure to horse serum and whether the patient has asthma, hay fever, or urticaria.
Physical examination Special attention should be paid to the area around the snakebite. The wound should be examined for fang marks, edema, petechiae, ecchymoses, and bullae. Thorough neurologic and cardiovascular examinations are indicated. If the patient was bitten on an extremity, circumferential measurements of the extremity should be taken at the site of injury and 5 in. proximal to the site. Distal pulses and neurologic status should be assessed and recorded, because edema from snakebites may result in elevated compartment pressures, leading to compartment syndrome.50,64 The patient should be monitored in an intensive care setting.
Laboratory tests All patients should have baseline laboratory studies performed, including a complete blood count, urinal-ysis, electrocardiogram, prothrombin time, partial thromboplas-tin time, fibrinogen levels, fibrin split products, serum electrolytes, blood urea nitrogen, and serum creatinine. Blood should be typed and screened. In severe envenomations, arterial blood gas determinations also are indicated. In patients with extremity edema, arterial Doppler evaluation and, in some cases, compartmental pressure determinations may be necessary.
Antivenin Therapy
Antivenins are available for bites of North American pit vipers and eastern coral snakes. Water moccasin and copperhead bites are typically managed without the use of antivenin. The choice whether to use antivenin is based on many factors, including clinical signs and symptoms of envenomation and the physiologic status of the victim. Antivenin is indicated only for severe envenomations.
Antivenin can be obtained through hospital pharmacies, veterinarians, local zoos, and poison control centers. Antivenin is most therapeutic when given within 4 hours after the bite. It is of limited value when given after 12 hours.52
Classification of envenomation Envenomations are classified according to a five-level system. The amount of antivenin given correlates with the grade of envenomation.
In grade 0 envenomations, the patient may have fang marks or superficial abrasions of the skin at the bite site but has minimal local edema or pain and no associated systemic manifestations.
Grade 1 envenomations involve some pain or throbbing at the bite site, with 1 to 5 in. of edema and erythema surrounding it. There are no systemic manifestations.
Grade 2 envenomations produce more severe pain over a larger area. The edema spreads toward the trunk, and petechiae and ecchymosis are present in the edematous area. There may be systemic involvement consisting of nausea, vomiting, and temperature elevation.
Grade 3 envenomation is considered severe. Edema spreads up the extremity and may move to the trunk. There may be generalized ecchymosis and petechiae. The patient may have a rapid pulse, hypotension, and hypothermia and may go into shock.
Grade 4 envenomation is very severe and usually results from the bite of a large snake or from a very large venom load. Edema, petechiae, ecchymosis, and necrosis rapidly overtake the extremity and a large portion of the trunk. Muscle fasciculations, sweating, nausea, vomiting, cramping, pallor, weak pulse, incontinence, convulsions, and coma may all occur.
Antivenins Multiple types of antivenin are on the market. The first marketed antivenin (Antivenin [Crotalidae] polyvalent [ACP]) was a horse-serum-based, whole antibody preparation. The dosage for that preparation was three to five ampules of an-tivenin diluted in 500 ml of intravenous fluid. Up to 54% of patients treated in studies were allergic to the ACP antivenin. Rash, hypotension, wheezing, and phlebitis occurred in 20% of patients.67 Nevertheless, clinicians would frequently forgo skin testing for allergy to ACP because it delayed administration of the antivenin.
Although the ACP antivenin is still produced and is used in some areas, a polyvalent crotalid (ovine) Fab antivenin (CroFab) has been introduced. This antivenin minimizes the risk of immediate hypersensitivity and prevents delayed serum sickness. It is based on sheep serum and is four to five times more potent than ACP.60 CroFab is made by immunizing sheep with crotaline snake venom and digesting the immune serum with papain to produce antibody fragments (Fab and Fc); the antigenic Fc segment is removed during purification.66 In a study of 1,000 treated patients, none showed evidence of true anaphylaxis.68 Each vial of CroFab contains 750 mg of Fab and is reconstituted in 10 ml of normal saline; four vials are diluted in 250 ml of normal saline. Studies have shown improvement at the 4-hour mark in all patients given this regimen, although some patients subsequently worsened.68 The half-life of Fab antivenin is less than 12 hours, compared with 61 to 194 hours for ACP,69,70 so repeat dosing of Fab may be needed to maintain therapeutic serum levels.71 In studies, only 16% of patients experienced serum sickness after administration of Fab antivenin, and the severity of the serum sickness was classified as only mild to moderate; in one study, the only reaction in 64 of 65 patients receiving antivenin was simple urticaria.72 The Fab antivenin is given in interval doses, with the first dose given to achieve initial control (defined as cessation of all symptoms—local, systemic, and coagulopathy) and subsequent doses given 6, 12, and 18 hours after the first dose. It is presumed that in some cases, coagulopathy may recur after initial neutralization of the venom. Recurrence may result from a depot of unneutralized venom at the bite site that is released into the circulation after the venom-antivenin complexes are cleared. A combination of edema, circulatory injury, and a lesser amount of subcutaneous tissue at the site of the bite may inhibit the antivenin from reaching the venom depot.60,73 Alternatively, uncleared complexes may dissociate, leaving free venom to recirculate.60,68
Adjunctive Therapy
A number of adjunctive therapies have been proposed for snakebite envenomations. Excision of tissue around the snakebite to remove the depot of venom was proposed at one time, but this approach is no longer used. The strategy of excising only necrotic-appearing tissue has likewise proved inadvisable, because histologic examination of the excised tissue revealed live muscle fibers interwoven with the macroscopically necrotic tissue. Aggressive debridement and antibiotic therapy may be indicated in the event of complications from infection. This may be seen with necrotizing fasciitis from either Vibrio vulnificans or Aeromonas hydrophila.
Extremity edema from a snakebite may mimic compartment syndrome, but true compartment syndrome is rare in such cases.
Most often, the subcutaneous tissue rather than the deep com-partmental space is involved. When a deep envenomation occurs and a true compartment syndrome does develop, first-line treatment is antivenin administration, which diminishes the compartmental pressure and swelling. Compartmental pressures greater than 30 mm Hg may indicate a need for fascioto-my, but fasciotomy and debridement should be avoided if possible because this procedure is associated with worse functional results. Fasciotomy is recommended only if a patient’s fingertip was bitten and has swelled, with loss of neurovascular or functional activity. Such patients are candidates for so-called digit dermotomy. The incision should be made on the lateral or medial aspect of the finger, through the skin only, and should extend from the web to the middle of the distal phalanx.
General Management
A regional poison control center or the local zoo should be used as a resource when dealing with a venomous snakebite. This is especially true if the snake is not believed to be native to the area, as might occur with hobbyists who keep exotic snakes as pets. For cases in which an expert is not available, the Department of Surgery at the University of California, San Diego, School of Medicine has established a Web site that lists protocols (including antivenin availability) for management of snakebites from venomous species around the world.
Other therapeutic measures are keyed to specific symptoms. Isotonic fluid replacement should be given if the patient is hy-potensive. Abnormalities of the clotting mechanism should be corrected with blood product replacement as necessary, but this should be done only after antivenin therapy has been started. In fact, common treatments for standard coagulopathies are ineffective or dangerous for snakebite-induced coagulopathies. Instead, the effects of the venom should be treated (with antivenin) before usual coagulopathy treatment is initiated.59 Cortico-steroids are contraindicated during the acute stages of enveno-mation, but they may be used if the patient experiences serum sickness from antivenin use. Studies in Costa Rica have shown that in viper bites, the release of inflammatory cytokines leads to clinical and pathologic alterations similar to those found in trauma patients.76 Further research on this reaction and on the potential use of steroids is indicated. Patients should be placed on oxygen and should be given mechanical support if necessary for signs of trismus, laryngeal spasm, or excessive salivation. Tetanus therapy should be given if indicated [see Table 3]. Antibiotics are recommended only if signs of infection are present. In one study, there were no wound infections in patients with nonen-venomated snakebite.
The wounds should be examined daily. Superficial necrosis and hemorrhagic blebs should be debrided at days 3 through 10. Debridement may need to be done in stages.