Epidermoid cyst
Diagnosis
Commonly called wens, epidermoid cysts have a lining that resembles the epidermis. Several types of cyst exist, but they are usually clinically indistinguishable from one another. On histo-logic examination, most of these cysts appear to be derived from hair follicles.
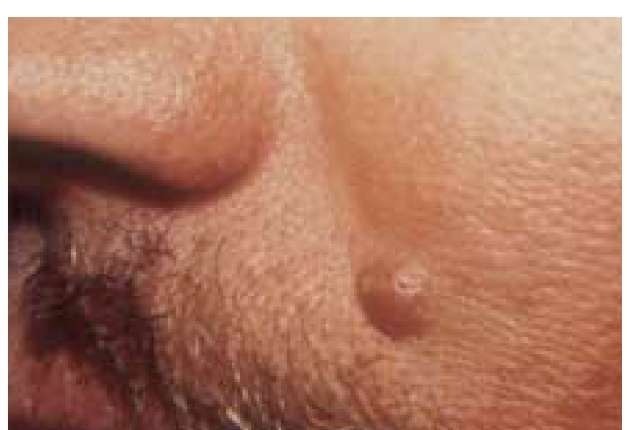
The epidermoid cyst is commonly located on the back and consists of one or more slow-growing, elevated, firm nodules, often with a central pore [see Figure 7]. The diameters of the lesions vary from 0.2 to 5.0 cm.
Treatment
The epidermoid cyst may be incised with a pointed scalpel to express its wall and contents, which consist of a thick kerati-nous material. If the cyst wall is not completely removed, there may be a recurrence of the lesion. Occasionally, the entire cyst has to be excised. Preliminary treatment with a systemic antibiotic, such as erythromycin, and warm-water compresses applied three or four times dally may be instituted if the cyst is inflamed and infected. When the inflammation and infection resolve, the lesion can be removed. Repeated episodes of infection may cause fibrosis, after which the cyst may have to be surgically excised.
Other Cysts
The pilar cyst, which is less common, has a wall that contains keratin similar to that found in hair. The contents of these cysts are semifluid and often have a rancid odor.
A milium is similar to an epidermoid cyst but differs mainly in size. Milia are white, hard subepidermal keratin cysts, 1 to 2 mm in diameter, that commonly arise spontaneously on the face [see Figure 8]. They may also arise secondarily in scars or in association with certain bullous diseases. Incision and expression of contents with a comedo extractor may be performed.
Familial Tumor Syndromes
Multiple cutaneous neoplasms may be a feature of familial tumor syndromes that are thought to be mediated by inactiva-tion of tumor suppressor genes. It is important to recognize these syndromes because they may be associated with underlying malignancies.
Figure 7 This large epidermoid cyst has a central pore, contains thick keratinous material, and has a lining that resembles the epidermis.
Figure 8 Milia, which are multiple small subepidermal inclusion cysts, can be observed in the periorbital area of this patient.
Muir-torre syndrome
Muir-Torre syndrome (MTS), previously known as Torre syndrome, consists of sebaceous gland neoplasms that are associated with visceral carcinoma and that arise from colonic epithelium. Sebaceous gland tumors may include, in decreasing order of frequency, adenomas, epitheliomas, and carcinomas.9 Keratoacan-thomas and sebaceous hyperplasia are also seen in patients with MTS. Colorectal cancer develops in 51% of patients with MTS a decade earlier than it develops in the general population. Genitourinary cancer develops in 24% of MTS patients. A germline mutation in the DNA mismatch repair gene hMSH2 has been identified in patients with MTS. Predictive diagnosis in family members should be preceded by careful genetic counseling.9
Gardner syndrome
Gardner syndrome consists of the triad of intestinal polypo-sis, bony tumors, and soft tissue lesions; it has an autosomal dominant inheritance. The colonic polyps eventually become malignant if left untreated. Soft tissue lesions include epider-moid cysts, sebaceous cysts, desmoid tumors, and scattered lentigines on the head and extremities.10
Cowden syndrome
Cowden syndrome is characterized by facial trichilemmo-mas and acral fibromas, and it is associated with an increased risk of cancer of the breast, thyroid, and gastrointestinal tract. This rare genodermatosis, which is also known as multiple hamartoma syndrome, is inherited as an autosomal dominant trait. It is important to make a prompt diagnosis of this syndrome because of the high risk of malignancy, particularly cancer of the breast in women.
Birt-hogg-dube syndrome
Birt-Hogg-Dube syndrome (BHDS) is an autosomal dominant multisystem disorder characterized by the cutaneous triad of fibrofolliculomas, trichodiscomas, and acrochordons. Fibro-folliculomas are benign tumors of the hair follicle. Fibrofolliculomas are firm, pink or skin-colored papules measuring 1 to 3 mm that appear on the face, particularly the nose, earlobes, and forehead. In the original kindred described by Birt (a dermatologist), Hogg (a pathologist), and Dube (a pathologist), family members were afflicted with medullary carcinoma of the thyroid. Subsequently, there appeared reports of patients with BHDS who had intestinal polyps, adenocarcinoma of the colon, parathyroid adenomas, and renal cell carcinoma. The skin tumors begin in early adulthood; systemic tumors appear years later. In families with recognized renal cell carcinoma, BHDS may account for 6% of the cases.11,12
Melanocytic (Pigment-Forming) Tumors
Benign tumors of pigment-forming cells, including those containing nevus cells (melanocytic nevi) and those of epidermal or dermal melanocytes, are of neuroectodermal origin.
Melanocytic nevus
Melanocytic nevus, also called nevus cell nevus, has a characteristic life history of evolution and involution. Melanocytic nevi are the most common of all skin tumors; each young adult has an average of 20 to 40 of them. Their incidence increases with age up to the second or third decade of life, after which they occur less commonly.
Risk Factors for Melanoma
An increase in the total number of melanocytic nevi is a risk factor for melanoma.13 In a study of 716 patients with newly diagnosed melanoma, an increased number of small nevi (25 to 49) was associated with a twofold increase in risk of melanoma; greater numbers of nevi were associated with further increased risk.14 The presence of one clinically dysplastic nevus was associated with a twofold increase in risk of melanoma; and 10 or more, with a 12-fold increase in risk. Criteria for dysplastic nevi included large size (over 5 mm), flatness (entirely macular or having a macular component), and at least two of the following: irregular pigmentation, asymmetry, and indistinct borders [see 2:XMalignant Cutaneous Tumors]. The presence of freckling conferred additional risk of melanoma for all types of nevi.
The relation between sun exposure and melanocytic nevi has been investigated to determine what environmental factors influence melanoma and to facilitate preventive measures. Studies suggest that melanocytic nevi are more common on sun-exposed skin sites and reach a peak incidence earlier in age on these sites than on covered areas of the body.15 A study of Australian schoolchildren showed an increasing prevalence of nevi with decreasing latitude, particularly in children 6 and 9 years of age.16 Sun exposure during childhood was considered to be a factor in the development of melanocytic nevi and an associated risk factor for melanoma.16 In Australia, however, sun exposure may be sufficient to maximally induce nevi regardless of latitude. Further studies need to be performed on persons living at higher latitudes to see whether the relation between sun exposure and nevi continues into adulthood.
Diagnosis
A melanocytic nevus that is present at birth or appears during the first year of life is considered to be congenital. Certain syndromes are associated with congenital nevi, including epidermal (linear sebaceous) nevus syndrome, neurocutaneous melanosis, premature-aging syndrome, and occult spinal dys-raphism or tethered cord syndrome.17 Various neuroectodermal defects and multisystem abnormalities may also be present. Giant congenital melanocytic nevi are associated with an increased risk of melanoma (see below).
Acquired melanocytic nevi vary considerably in form, ranging from flat to pedunculate. They may be hairy or hairless and may be skin colored, dark brown, or even black. Nevi that are flat and darkly pigmented are called junctional nevi. Slightly raised nevi are often compound; that is, they contain both epidermal and dermal components. Nevi that are predominantly intradermal are usually more elevated and contain less pigment than compound or junctional nevi. Nevi that are papillomatous, dome shaped, or pedunculate are usually intradermal [see Figures 9 through 11].
Differential Diagnosis
The differential diagnosis of melanocytic nevi includes ephelis (freckle), lentigo, cafe au lait spot (see below), wart, seb-orrheic keratosis, and skin tag (a small pedunculate protrusion of skin that does not contain nevus cells). Ephelis is a tan mac-ule, commonly seen in children after sun exposure; it often dis-appears in the winter.
Figure 9 A flat junctional nevus with dark pigmentation is seen in this patient.
Figure 10 This slightly raised compound nevus typically has less pigmentation than a junctional nevus.
Figure 11 A skin-colored intradermal nevus with a dome-shaped configuration is seen on the face.
Lentigo, also called senile lentigo or liver spot, is a tan or brown macule commonly seen on exposed skin areas, such as the face, the backs of the hands, and the neck. The labial melanotic macule is a distinct entity that appears in adults as a well-defined brown or black pigmented macule on the lip. In a study of 79 patients, the majority of melanocytic lesions (94%) were on the central third of the lower lip, suggesting that exposure to ultraviolet light has a causative role.18 Patients followed for up to 13 years had no adverse developments, a finding indicative of the benign nature of this lesion.
Treatment
No treatment is required for melanocytic nevi. However, shave biopsy or excisional biopsy may be performed for cosmetic reasons or when a nevus is subject to irritation because of pressure from clothing or because it is located in an intertrigi-nous area. Patients should be followed with serial photographs. Biopsy should be performed for nevi that appear prone to malignant transformation; nevi that show severe dys-plasia should be removed. Removal of mildly or moderately dysplastic nevi is advocated by some but not all experts [see 2:XIMalignant Cutaneous Tumors].
Cafe au lait spots
Cafe au lait spots are common benign congenital or acquired birthmarks. They are tan, round to oval macules ranging in size from several millimeters to 10 to 20 cm. They can occur on any area of the body but are more common on the trunk, buttocks, and lower extremities. The presence in a prepubertal child of five or more cafe au lait spots larger than 0.5 cm may be a marker for neurofibromatosis-1 (NF-1) (see below).19 Histologi-cally, cafe au lait spots show an increased number of dihydrox-yphenylalanine (DOPA)-positive melanocytes that produce an increased concentration of melanosomes. The cafe au lait spots seen in Albright hereditary osteodystrophy are usually unilateral and show jagged rather than smooth margins. An association of juvenile xanthogranulomas with cafe au lait macules carries an increased risk of underlying systemic disorders, including leukemia.20
Halo nevus
A halo nevus consists of an acquired zone of hypopigmenta-tion surrounding a pigmented tumor, most commonly a compound nevus [see Figure 12]; other tumors, even malignant melanoma, may also be surrounded by a depigmented halo. The halo lesion typically involutes during a period of months in the absence of clinical signs of inflammation. Histologically, a chronic lymphocytic infiltrate surrounds the nevus cells, which may represent an autoimmune phenomenon.
Spindle cell nevus
Formerly called benign juvenile melanoma, spindle cell nevus usually arises in childhood as a pink or reddish-brown, smooth or slightly scaly, firm papule with a predilection for the face, especially the cheeks [see Figure 13].21 Although benign, spindle cell nevus may closely resemble a malignant melanoma. Excisional biopsy is therefore advisable in many cases.
Mongolian spot
The mongolian spot is a bluish macule that is seen in new-borns of dark-skinned races. The discoloration is caused by persistence of dermal melanocytes, often in the lumbosacral region [see Figure 14]. The lesion usually disappears by 3 or 4 years of age.
Blue nevus
The common blue nevus occurs as a solitary, sharply circumscribed, blue-black papule [see Figure 15]. This malformation consists of a group of melanocytes with long, thin surface projections in the middle and lower thirds of the dermis andin subcutaneous fat.
Figure 12 The halo nevus may represent an autoimmune phenomenon; a zone of hypopigmentation may appear around a nevus, with subsequent involution of the pigmented tumor.
Figure 13 The spindle cell nevus is an active compound nevus that may be difficult to distinguish histologically from a melanoma.
Figure 14 The bluish pigmentation of a mongolian spot is seen in the lumbosacral area and is caused by the persistence of dermal melanocytes.
The common blue nevus does not show a tendency toward malignant transformation. The cellular blue nevus, which appears as a blue-black nodule or an indurated plaque, contains two types of cells: spindle shaped and rounded. The cellular blue nevus may in rare instances become malignant.