Information Technology Reference
In-Depth Information
low time effort in the sagittal reformations of non-dedicated routine abdominal
contrast-enhanced MDCT [
53
]. This offers the possibility to determine lumbar
BMD values in the same reformations which are known for a substantial better
detection of osteoporotic vertebral fractures [
35
,
36
]. Thus, radiologists can assess
vertebral fracture status and BMD in the sagittal reformations in an acceptable time
which is critical in clinical routine. Baum et al. determined in ten patients standard
QCT-based BMD of L1
L3 in the sagittal refor-
mations of routine abdominal contrast-enhanced MDCT images [
53
]. Apparent
BMD values of contrast-enhanced MDCT were on average 56 mg/cm
3
higher than
those of standard QCT. A correlation coef
L3 and apparent BMD of L1
-
-
cient of r = 0.94 was calculated for the
BMD values of MDCT and standard QCT with the conversion equation
BMD
QCT
=0.69
BMD
MDCT
-11 mg/ml. Using this conversion equation, lumbar
BMD measurements in the sagittal reformations of routine abdominal contrast-
enhanced MDCT images could adequately differentiate patients with versus without
osteoporotic vertebral fractures. Furthermore, baseline converted lumbar BMD
values predicted incident osteoporotic vertebral fractures during a follow-up of
20
×
12 months [
54
]. The BMD measurements in the sagittal reformations were
performed by placing manually circular regions of interest (ROIs) in the ventral
halves of the trabecular compartment of the vertebral bodies of L1
±
L3, in each case
equidistant to both endplates (Fig.
8
). The attenuation values measured in the ROIs
in Hounsfield Unit were converted into mg/cm
3
calcium hydroxyapatite using a
-
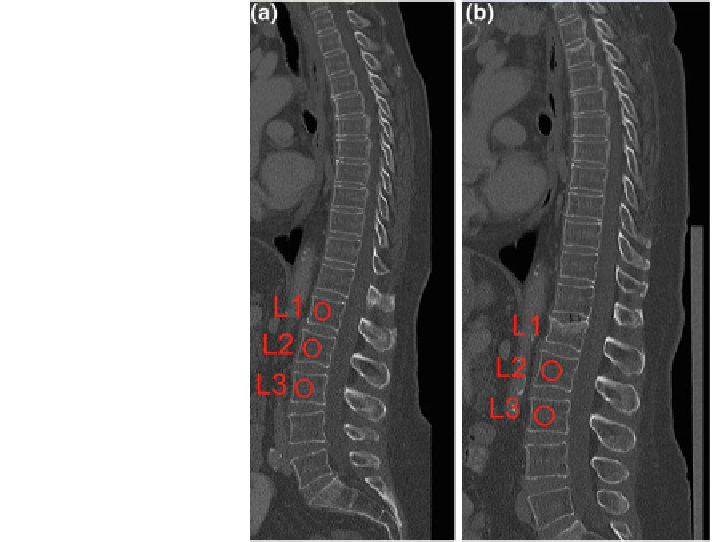
Fig. 8 BMD measurements
in sagittal reformations of
routine contrast-enhanced
MDCT in a patient at baseline
(a) and follow-up (b).
Circular ROIs (red) were
manually placed in L1
-
L3.
Note the incident osteoporotic
vertebral fracture of L1 at
8-month follow-up