Biomedical Engineering Reference
In-Depth Information
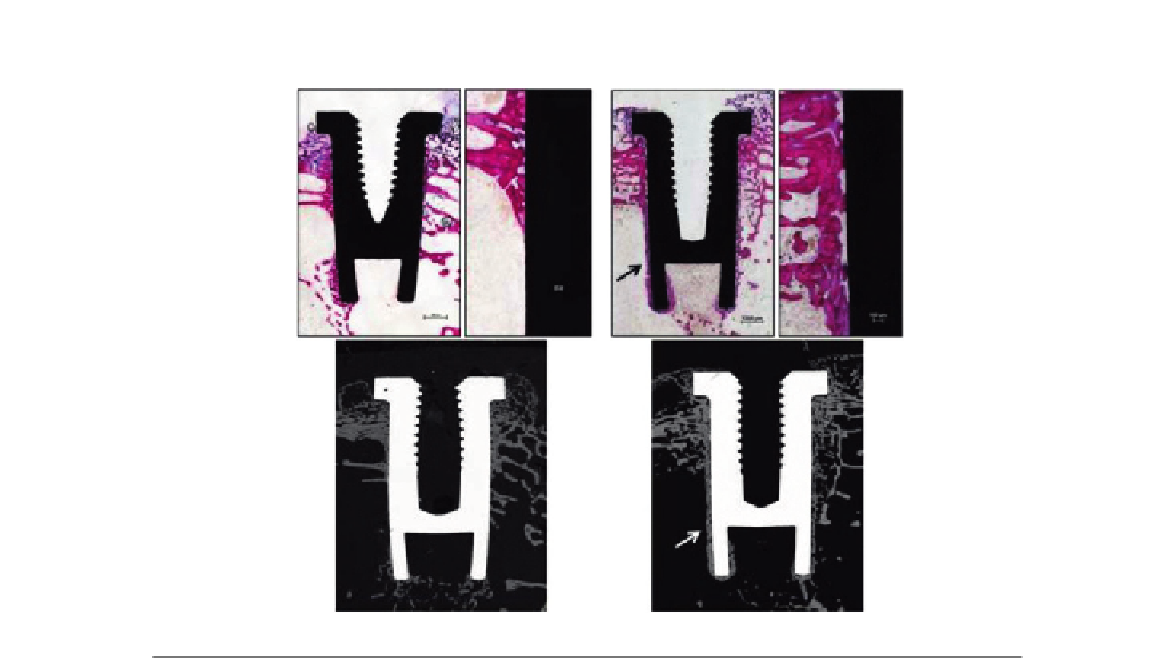
Ti
CaP
FIGURE 16.6
Micrographs showing the osseointegration of bare titanium (Ti) and CaP-coated implants after implantation in
femoral condyles of rabbits for 4 weeks. Note the direct bone apposition on CaP-coated implants (arrows) on
both histology (basic fuchsine, toluidine blue staining) and back-scattered electron microscopy (BSEM)
images.
implant interface are influenced by the chemistry, topography, and wettability of dental implant
surfaces. The challenge in developing new implant surface is increasing the clinical success rate as
well as decreasing the tissue healing time for immediate loading of implants, particularly in esthetic
situations
[66
68]
. One of the objectives is to develop implant surfaces having predictable, con-
trolled, and guided tissue healing. For instance, surfaces that promote contact osteogenesis rather
than distance osteogenesis would be desired in bone site while intimate fibrous tissue healing would
be in the gingival tissue (
Figure 16.1
). In order to enhance this intimate contact between tissues
and implant, surface treatments at the nanometer scale have been performed on metal implants and
tested in various animal models. Implant surface with various roughness has been used to increase
the total area available for osteoapposition. Kubo et al.
[66]
observed a substantial increase by 3.1
times in bone
titanium interfacial strength by Ti nanotube (300 nm) at 2 weeks of implantation in
femur of rats. These results suggest the establishment of nanostructured surfaces for improved
osteoconductivity. Moreover, Ogawa et al.
[69]
have prepared Ti nanostructure by physical vapor
deposition and tested their osseointegration in femur of rats. They found an increased surface area
by up to 40% and a greater strength of osseointegration for the nanostructured compared to an